Volume 14, Issue 3 (Autumn 2019)
Salmand: Iranian Journal of Ageing 2019, 14(3): 342-355 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rakhshani Z, Nastiezaie N. Relationship of Design and Architectural Factors of Nursing Homes With the Mental Health of Their Residents. Salmand: Iranian Journal of Ageing 2019; 14 (3) :342-355
URL: http://salmandj.uswr.ac.ir/article-1-1497-en.html
URL: http://salmandj.uswr.ac.ir/article-1-1497-en.html
1- Department of Architecture, Faculty of Architecture and Urban Design, Isfahan Art University, Isfahan, Iran. , zohrerakhshani1479@yahoo.com
2- Department of Educational Management, Faculty of Education and Psychology, University of Sistan and Baluchestan, Zahedan, Iran.
2- Department of Educational Management, Faculty of Education and Psychology, University of Sistan and Baluchestan, Zahedan, Iran.
Keywords: Designing and Architecture, Nursing Home, Aging, Mental Health, Depression, Anxiety, Social function disorder
Full-Text [PDF 2909 kb]
(6907 Downloads)
| Abstract (HTML) (9095 Views)
Full-Text: (4279 Views)
1. Introduction
The older people are more susceptible to mental health problems because of their age and disability in physical and mental dimensions [1]. The mental disorders in older people living in the nursing homes are more common than those in older people living in the community [2], and a high proportion of them have significant mental disorders [3]. For example, in a study, the prevalence of depression was 23% to 40% in older people living in the community, 25% to 80% for those living in nursing homes, and 51.4% of them had mental disorders [4]. In other words, staying in a nursing home is a significant and independent factor in increasing the prevalence of mental disorders [5]. Disregarding the environmental quality of nursing homes can affect the mental health of older people. In this regard, this study aimed at evaluating the association of design and architecture of nursing homes with the mental health of their residents.
2. Materials and Methods
This research is a descriptive correlational study. The study population consisted of all older people living in nursing homes of Shahriar (n=78) and Qods (n=193) counties in Tehran Province, Iran in December 2017. Using a purposive sampling method, we recruited 158 older people (45 from Shahriar and 113 from Qods). The inclusion criterion included having at least 3 months of residence in the nursing home. After the research was approved by the Isfahan University of Art, the necessary arrangement was made with the authorities of nursing homes.
The data collection tools were two questionnaires; one was a researcher-made instrument surveying design and architecture of nursing homes, and the other was the General Health Questionnaire-28 (GHQ-28). To determine the validity of the questionnaires, the content validity method was used, and its reliability was examined on 30 samples, who were randomly selected. Then, the Cronbach α coefficient was calculated. The overall Cronbach α was 0.903 for the first questionnaire and 0.833, 0.968, 0.975, 0.797, and 0.863 for its subscales of lighting, public space, personal space, access space, and green space, respectively. The overall Cronbach α was 0.923 for the GHQ-28 and 0.865, 0.883, 0.746, and 0.897 for its subscales of somatic symptoms, anxiety/insomnia, social dysfunction, and severe depression, respectively. The subjects answered the questions individually. In cases where the older people were semi-literate, illiterate, or disabled, the researcher completed the questionnaire by interviewing them. Before the distribution of the questionnaires, the purpose of the research was explained to the participants. We assured them that their information would be completely confidential and would only be used for the study. They voluntarily participated in the research. So they were allowed to leave it if desired. In this study, no sample drop was reported. For analyzing the collected data, the Pearson correlation test and multiple regression analysis were used in SPSS V. 21.
3. Results
The participants were 158 older people (100 men and 58 women) with a Mean±SD age of 68.78±4.82 years and a Mean±SD stay of 27.71±16.97 months in the nursing homes. The results reported a Mean±SD score of 22.93±4.96 for lighting, 27.41±5.01 for public space, 25.15±7.27 for personal space, 28.62±3.69 for access space, 37.48±6.43 for green space, 16.47±2.99 for somatic symptoms, 16.51±3.99 for anxiety/insomnia, 12.13±2.72 for social dysfunction, and 16.39±3.08 for severe depression. As can be seen, the mean scores of lighting, personal space, and green space were higher than the theoretical average. Therefore, samples have higher than average satisfaction with these factors. However, given that the mean scores of public space and access space were lower than the theoretical average, samples had little satisfaction with their public and access spaces (P<0.05). In terms of general health, the mean score of 4 subscales was higher than that of the theoretical average; hence, the samples had lower than average mental health level (P<0.05).
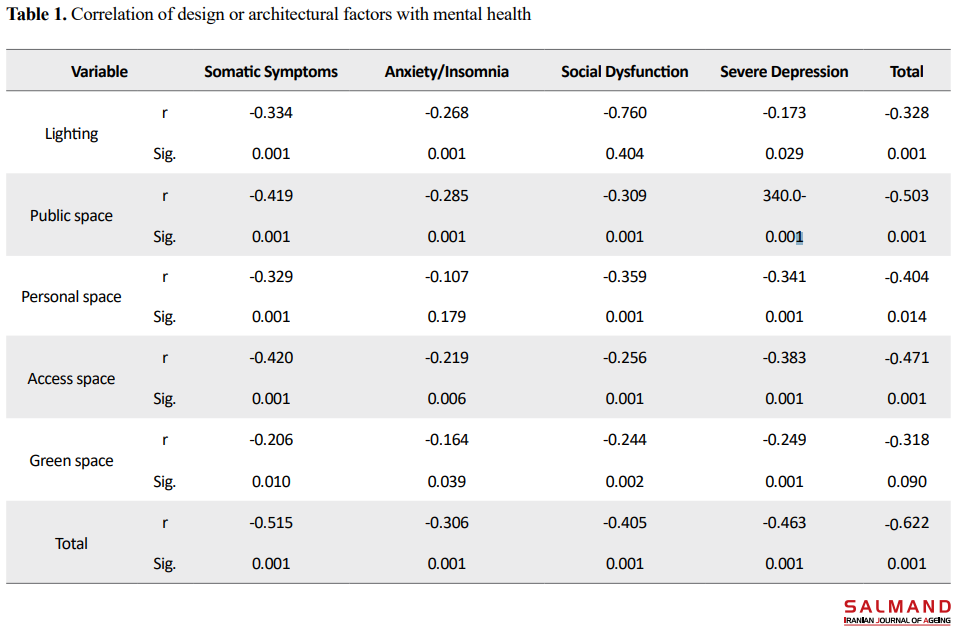
We used the Pearson correlation test to evaluate the relationship of design or architecture of the nursing homes with the mental health of their residents. Table 1 presents the findings. The correlation coefficients of the factors of lighting, public space, personal space, access space, and green space with mental health were -0.662, -0.328, -0.503, -0.404, -0.471, and -0.318, respectively (P<0.001). Then, we used multiple regression analysis to predict the mental health of elderly residents based on design or architectural factors. Based on the regression model, the F-value was significant at the 0.001 level. Therefore, the null hypothesis stating that the regression model is not significant was rejected at 0.99 confidence interval, and it is accepted that the linear regression model has a good fit. The coefficient of determination (R2) is 0.402, which means that the design/architectural factors of the nursing homes explain 40.2% of variations in the mental health of the elderly residents. Among these factors, public space (β=-0.276), personal space (β=-0.216), access space (β=-0.190) and green space (β=-0.145) had the highest prediction powers, respectively. The lighting factor was excluded from the model because it was not significant.
4. Conclusion
There was a negative and significant relationship between older people's satisfaction with the design and architecture of the nursing home and their mental health. This means that with lower satisfaction with the quality of the design and architecture of the nursing home, the mental health of the elderly will be at risk, which leads them to perceive more significant physical problems, anxiety/insomnia, depression, and social dysfunction. Regarding the effect of design and architecture of the nursing homes on the mental health of residents, the authorities should understand the importance of these factors for such places and consider it in their plans to improve the mental health of older people living in these settings. As one of the limitations of the study, we only investigated the older people living in sanatoriums, so the results could not be generalized to all cases.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; Moreover, They were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed in preparing this article.Conflicts of interest
The authors declared no conflict of interest.
The older people are more susceptible to mental health problems because of their age and disability in physical and mental dimensions [1]. The mental disorders in older people living in the nursing homes are more common than those in older people living in the community [2], and a high proportion of them have significant mental disorders [3]. For example, in a study, the prevalence of depression was 23% to 40% in older people living in the community, 25% to 80% for those living in nursing homes, and 51.4% of them had mental disorders [4]. In other words, staying in a nursing home is a significant and independent factor in increasing the prevalence of mental disorders [5]. Disregarding the environmental quality of nursing homes can affect the mental health of older people. In this regard, this study aimed at evaluating the association of design and architecture of nursing homes with the mental health of their residents.
2. Materials and Methods
This research is a descriptive correlational study. The study population consisted of all older people living in nursing homes of Shahriar (n=78) and Qods (n=193) counties in Tehran Province, Iran in December 2017. Using a purposive sampling method, we recruited 158 older people (45 from Shahriar and 113 from Qods). The inclusion criterion included having at least 3 months of residence in the nursing home. After the research was approved by the Isfahan University of Art, the necessary arrangement was made with the authorities of nursing homes.
The data collection tools were two questionnaires; one was a researcher-made instrument surveying design and architecture of nursing homes, and the other was the General Health Questionnaire-28 (GHQ-28). To determine the validity of the questionnaires, the content validity method was used, and its reliability was examined on 30 samples, who were randomly selected. Then, the Cronbach α coefficient was calculated. The overall Cronbach α was 0.903 for the first questionnaire and 0.833, 0.968, 0.975, 0.797, and 0.863 for its subscales of lighting, public space, personal space, access space, and green space, respectively. The overall Cronbach α was 0.923 for the GHQ-28 and 0.865, 0.883, 0.746, and 0.897 for its subscales of somatic symptoms, anxiety/insomnia, social dysfunction, and severe depression, respectively. The subjects answered the questions individually. In cases where the older people were semi-literate, illiterate, or disabled, the researcher completed the questionnaire by interviewing them. Before the distribution of the questionnaires, the purpose of the research was explained to the participants. We assured them that their information would be completely confidential and would only be used for the study. They voluntarily participated in the research. So they were allowed to leave it if desired. In this study, no sample drop was reported. For analyzing the collected data, the Pearson correlation test and multiple regression analysis were used in SPSS V. 21.
3. Results
The participants were 158 older people (100 men and 58 women) with a Mean±SD age of 68.78±4.82 years and a Mean±SD stay of 27.71±16.97 months in the nursing homes. The results reported a Mean±SD score of 22.93±4.96 for lighting, 27.41±5.01 for public space, 25.15±7.27 for personal space, 28.62±3.69 for access space, 37.48±6.43 for green space, 16.47±2.99 for somatic symptoms, 16.51±3.99 for anxiety/insomnia, 12.13±2.72 for social dysfunction, and 16.39±3.08 for severe depression. As can be seen, the mean scores of lighting, personal space, and green space were higher than the theoretical average. Therefore, samples have higher than average satisfaction with these factors. However, given that the mean scores of public space and access space were lower than the theoretical average, samples had little satisfaction with their public and access spaces (P<0.05). In terms of general health, the mean score of 4 subscales was higher than that of the theoretical average; hence, the samples had lower than average mental health level (P<0.05).
We used the Pearson correlation test to evaluate the relationship of design or architecture of the nursing homes with the mental health of their residents. Table 1 presents the findings. The correlation coefficients of the factors of lighting, public space, personal space, access space, and green space with mental health were -0.662, -0.328, -0.503, -0.404, -0.471, and -0.318, respectively (P<0.001). Then, we used multiple regression analysis to predict the mental health of elderly residents based on design or architectural factors. Based on the regression model, the F-value was significant at the 0.001 level. Therefore, the null hypothesis stating that the regression model is not significant was rejected at 0.99 confidence interval, and it is accepted that the linear regression model has a good fit. The coefficient of determination (R2) is 0.402, which means that the design/architectural factors of the nursing homes explain 40.2% of variations in the mental health of the elderly residents. Among these factors, public space (β=-0.276), personal space (β=-0.216), access space (β=-0.190) and green space (β=-0.145) had the highest prediction powers, respectively. The lighting factor was excluded from the model because it was not significant.
4. Conclusion
There was a negative and significant relationship between older people's satisfaction with the design and architecture of the nursing home and their mental health. This means that with lower satisfaction with the quality of the design and architecture of the nursing home, the mental health of the elderly will be at risk, which leads them to perceive more significant physical problems, anxiety/insomnia, depression, and social dysfunction. Regarding the effect of design and architecture of the nursing homes on the mental health of residents, the authorities should understand the importance of these factors for such places and consider it in their plans to improve the mental health of older people living in these settings. As one of the limitations of the study, we only investigated the older people living in sanatoriums, so the results could not be generalized to all cases.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; Moreover, They were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed in preparing this article.Conflicts of interest
The authors declared no conflict of interest.
References
- Barati M, Fathi Y, Soltanian AR, Moeini B. [Mental health condition and health promoting behaviors among elders in hamadan (Persian)]. Scientific Journal of Hamadan Nursing & Midwifery Faculty. 2012; 20(3):12-22.
- Saberian M, Haji Agajai S, Ghorbani R. [Study of the mental status of the elderly and its relationship with leisure time activities (Persian)]. Journal of Sabzevar University of Medical Sciences. 2009; 10(4):12-9.
- Pachana N, Laidlaw K. Oxford handbook of geropsychology.Oxford: Oxford University Press 2012.
- Najafi B, Arzaghi SM, Fakhrzadeh H, Sharifi F, Shaei Sh, et al. [Mental health status of the elderly in Tehran and its related factors to measure equity in health and related factors (Persian)]. Journal of Diabetes and Metabolism 2013; 13(1):62-73.
- Navabinejad SH, Dowkaneh F, Shirzadi S. [The effect of family factors on the mental health of elderly men and women (Persian)]. Research of Educational Management. 2113;5(1):119-31.
- Jafari E, Hajloo N, Faghani R, Khazan K. [The relationship between spiritual well-being, hardiness, and mental health in the elderly (Persian)]. Journal of Behavioral Science. 2012; 4(11):221-31.
- Mortazavi SS, EftekharArdebili H, Darali R. [Mental health of elderly and its relation to demographic and social factors (Persian)]. Payesh. 2011; 10(4):485-92.
- Shoja M, Nabavi S, Kassani A, Bagheri yazdi S. [Factor analysis of social capital and its relations with mental health of older people in 9 districts of Tehran (Persian)]. Journal of North Khorasan University of Medical Sciences. 2012; 3(5):81-90. [DOI:10.29252/jnkums.3.5.S5.81]
- Pourazar M, Sheikh M, Sohbatiha M, Mohamadnia S. [Comparison of mental health in senior male citizens with different levels of weekly exercise (Persian)].Journal of Research in Rehabilitation Sciences. 2013; 9(5):852-60.
- Sahebdel H, Khoshkonash A, Taghipoor E. [Effect of reality therapy on elderly mental health Hasheminejad Kahrizak (Persian)]. Iranian Journal of Ageing 2012;7(1):16-24.
- Brar R, Kaur J, Isha Sh. Mental health of elderly as related to their well being and self esteem. International Journal of Humanities and Social Science Invention. 2013; 2(11):54-7.
- Singh AP, Shukla A, Singh PA. Perceived self efficacy and mental health among elderly. Delhi Psychiatry Journal. 2010; 13(2):312-21.
- Mokhtari F, Ghasemi N. [Comparison of quality of life and mental health of elderly residents/ non-residents of nursing homes (Persian)]. Iranian Journal of Ageing. 2010; 5(18):53-63.
- Haggstrom E, Mbusa E, Wadensten B. Nurses workplace distress and etical dilemmas in Tanzanian health care. Nurs Ethics 2008; 15(4): 478-91. [DOI:10.1177/0969733008090519] [PMID]
- Jongenelis K, Pot AM, Eisses AM, Beekman AT, Kluiter H, Ribbe MW. Prevalence and risk indicators of depression in elderly nursing home patients: The AGED study. Journal of Affective Disorders. 2004; 83(2-3):135-42. [DOI:10.1016/j.jad.2004.06.001] [PMID]
- Grabowski DC, Aschbrenner KA, Rome VF, Bartels SJ. Review: Quality of mental health care for nursing home residents: A literature review, Medical Care Research and Review. 2010; 67(6):627-56. [DOI:10.1177/1077558710362538] [PMID] [PMCID]
- Lampert MA, Rosso ALP. Depression in elderly women resident in a long-stay nursing home. Dement Neuropsychol. 2015; 9(1):76-80. [DOI:10.1590/S1980-57642015DN91000012] [PMID] [PMCID]
- Etemadi A, Ahmadi K. [Psychological disorders of elderly home residents (Persian)]. Journal of Applied Sciences. 2009; 9(2009):549-54. [DOI:10.3923/jas.2009.549.554]
- Vila-Corcoles A, Aguirre-Chavarria C, Ochoa- Gondar O, de Diego C, Rodriguez-Blanco T, Gomez F, et al. Influence of chronic illnesses and underlying risk conditions on the incidence of pneumococcal pneumonia in older adults. Infection. 2015; 43(6):699-706. [DOI:10.1007/s15010-015-0801-y] [PMID]
- Marengoni A, Winblad B, Karp A, Fratiglioni L. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. American Journal of Public Health. 2008; 98(7):1198-200. [DOI:10.2105/AJPH.2007.121137] [PMID] [PMCID]
- Nasiri M, Foroughan M, Rashedi V, Makarem A, Jafari Mourjan B. [Compliance to universal design criteria in nursing homes of Tehran (Persian)]. Iranain Journal of Ageing. 2016; 11(2):340-47. [DOI:10.21859/sija-1102340]
- Ghazi K, Foroughan M, Hosseini M, Hosseinzadeh S, Askari, M. The client satisfaction of delivered services in private nursing homes for elderly: a survey in the Provinces of Golestan, Mazandaran, Semnan and Northern Khorasan in 2012 (Persian)]. Journal Of Sabzevar University of Medical Sciences. 2013; 20(3):320-30.
- Nazemi L, Skoog I, Karlsson I, Hosseini S, Hosseini M, Hosseinzadeh MJ, et al. [Depression, prevalence and some risk factors in elderly nursing homes in Tehran, Iran (Persian)]. Iranian Journal of Public Health. 2013; 42(6):559-69.
- World Health Organization. Ageing and life-course. Genev: World Health Organization; 2016.
- Danial Z, Motamedi MH, Mirhashemi S, Kazemi A, Mirhashemi AH. Ageing in Iran. The Lancet. 2014; 384(9958):1927-8.[DOI:10.1016/S0140-6736(14)62278-9]
- Hamid N, Babamiri M. [The Relationship of Green Space and Mental Health (Persian)]. Armaghane Danesh Journal. 2012; 17(4):309-15.
- Leith KH. A phenomenological exploration of the meaning of home for older women in congregate housing. Journal of Aging Studies. 2006, 20(4):317-33. [DOI:10.1016/j.jaging.2005.12.002]
- Andersson JE. Architecture for the silver generation: Exploring the meaning of appropriate space for ageing in a Swedish municipality. Health & Place. 2011; 17(2):572-87.[DOI:10.1016/j.healthplace.2010.12.015] [PMID]
- Lee Y, Hwang J, Lim S, Lee H, & Tai Kim J. Identifying space planning guidelines for elderly care environments from the holistic health perspective. Paper presented at: 6th International Symposium on Sustainable Healthy Buildings. 28 may 2012; Seoul, Korea.
- Zarghami E, Sharghi A, Olfat M. [Environmental features affecting the quality of life among elderly residents in nursing homes, case study: Shemiranat area in Tehran Province (Persian)]. Journal of Iran Architecture Studies. 2015; 1(7):111-26.
- Bowling A, Hankins M, Windle G, Bilotta C, Grant R. A short measure of quality of life in older age: The performance of the brief Older People's Quality of Life questionnaire (OPQOL-brief). Archives of Gerontology and Geriatrics. 2013; 56(1):181-7.[DOI:10.1016/j.archger.2012.08.012] [PMID]
- Matsuoka Y. The elderly housing as a place to age in place comparative study on the pattern of mortality/discharge in Denmark and Japan. Paper presented at: ENHR 2009 International Conference: Changing Housing Markets: Integration and Segmentation 2009. 28June-1 July 2009; Prague, Czech Republic.
- Kakooei H, Rahimi MH, Hosseini M. The role of bright light during night work on stress and health status of shift work nurses. International Journal of Occupational Hygiene. 2009; 1(1):46-50.
- Meesters Y, Dekker V, Schlangen L, Bos E, Ruiter M. Low-intensity blue-enriched white light (750 lux) and standard bright light (10 000 lux) are equally effective in treating SAD, A randomized controlled study. BMC psychiatry 2011; 11:17. [DOI:10.1186/1471-244X-11-17] [PMID] [PMCID]
- Dowling GA, Burr RL, Van Someren EJ, Hubbard EM, Luxenberg JS, Mastick J, et al. Melatonin and bright light treatment for rest-activity disruption in institutionalized patients with alzheimer’s disease. Journal of the American Geriatrics Society. 2008; 56(2):239-46. [DOI:10.1111/j.1532-5415.2007.01543.x] [PMID] [PMCID]
- Richter K, Acker J, Kamcev N, Bajraktarov S, Piehl A, Niklewski G. Recommendations for the prevention of breast cancer in shift workers. EPMA Journal. 2011; 2(4):351-6. [DOI:10.1007/s13167-011-0126-6] [PMID] [PMCID]
- Hickman SE, Barrick AL, Williams CS, Zimmerman S, Connell BR, Preisser JS, et al. The effect of ambient bright light therapy on depressive symptoms in persons with dementia, Journal of the American Geriatrics Society 2007; 55(11):1817-24. [DOI:10.1111/j.1532-5415.2007.01428.x] [PMID]
- Campbell SS, Dijk DJ, Boulos Z, Eastman CI, Lewy AJ, Terman M. Light treatment for sleep disorders: Consensus report III. Alerting and activating effects. Journal of Biological Rhythms. 1995; 10(2):129-32. [DOI:10.1177/074873049501000205] [PMID]
- Boyce P, Barriball E. Circadian rhythms and depression. Australian Family Physician. 2010; 39(5):307-10. [PMID]
- Ancoli-Israel S, Gehrman P, Martin JL, Shochat T, Marler M, Corey-Bloom J, et al. Increased light exposure consolidates sleep and strengthens circadian rhythms in severe Alzheimer’s disease patients. Behavioral Sleep Medicine. 2003; 1(1):22-36. [DOI:10.1207/S15402010BSM0101_4] [PMID]
- Karami Z, Golmohammadi R, HeidariPahlavian A, Heidari Moghaddam R, Poorolajal J. [The effect of daylight on mental health of elderly (Persian)]. Journal of Ergonomics. 2013; 1(2):49-54.
- Ebrahimzade I, Ebadijokandal E. Analysis of space-location administration of green space in three zone of Zahedan (Persian)]. Journal of Geography and Development. 2008; 11(2):39-58.
- Hartig T, Fransson U. Leisure home ownership, access to nature, and health: A longitudinal study of urban residents in Sweden. Environment and Planning. 2009; 41(1):82-96. [DOI:10.1068/a401]
- Velarde MD, Fry G, Tveit M. Health effects of viewing landscapes- landscape types in environmental psychology. Urban Foresty and Urban Greening. 2007; 6(4):199-212. [DOI:10.1016/j.ufug.2007.07.001]
- Pryor A, Townsend M, Maller C, Field K. Health and well-being naturally: 'Contact with nature'in health promotion for targeted individuals, communities and populations. Health Promotion Journal of Australia. 2006; 17(2):114-23. [DOI:10.1071/HE06114] [PMID]
Type of Study: Research |
Subject:
Psychiatry
Received: 2018/03/06 | Accepted: 2018/06/26 | Published: 2019/11/10
Received: 2018/03/06 | Accepted: 2018/06/26 | Published: 2019/11/10
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |