Volume 13, Issue 4 (Winter 2019)
Salmand: Iranian Journal of Ageing 2019, 13(4): 452-463 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ahmadi A, Sahaf R, Rashedi V, Akbari Kamrani A A, Shati M, Delbari A. Relationship Between Oral Health and Demographic Characteristics in Retired Elderly People in Iran. Salmand: Iranian Journal of Ageing 2019; 13 (4) :452-463
URL: http://salmandj.uswr.ac.ir/article-1-1399-en.html
URL: http://salmandj.uswr.ac.ir/article-1-1399-en.html
Amir Ahmadi1 

 , Robab Sahaf2
, Robab Sahaf2 

 , Vahid Rashedi3
, Vahid Rashedi3 

 , Ahmad Ali Akbari Kamrani2
, Ahmad Ali Akbari Kamrani2 

 , Mohsen Shati2
, Mohsen Shati2 

 , Ahmad Delbari *
, Ahmad Delbari * 

 4
4


 , Robab Sahaf2
, Robab Sahaf2 

 , Vahid Rashedi3
, Vahid Rashedi3 

 , Ahmad Ali Akbari Kamrani2
, Ahmad Ali Akbari Kamrani2 

 , Mohsen Shati2
, Mohsen Shati2 

 , Ahmad Delbari *
, Ahmad Delbari * 

 4
4
1- Department of Ageing, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Aging, Iranian Research Center on Aging, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- School of Behavioral Sciences and Mental Health (Tehran Psychiatric Institute), Iran University of Medical Sciences, Tehran, Iran.
4- Department of Aging, Iranian Research Center on Aging, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,ahmad_1128@yahoo.com
2- Department of Aging, Iranian Research Center on Aging, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- School of Behavioral Sciences and Mental Health (Tehran Psychiatric Institute), Iran University of Medical Sciences, Tehran, Iran.
4- Department of Aging, Iranian Research Center on Aging, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
Full-Text [PDF 4321 kb]
(2949 Downloads)
| Abstract (HTML) (7414 Views)
Full-Text: (4542 Views)
Extended Abstract
1. Objectives
In recent years, there has been a rapid growth of the elderly population in Iran. According to 2016 national census, with 9.3% of Iranian people aged ≥60 years, Iranian population has become older [1]. Oral health of the elderly is a major public health issue calling for more attention worldwide. With the increase in the elderly population, the prevalence of oral and dental problems increases [2]. The factors associated with oral health vary because of socioeconomic and cultural differences among the elderly in different societies [3]. Several studies in Iran investigated the oral health status of elderly and its relationship with their quality of life and knowledge. However, information is scarce about the relationship between their oral health and demographic characteristics. This study aimed to investigate the association between these 2 variables among retired elderly people in Iran.
2. Methods and Materials
This cross-sectional study was conducted on 158 retired elderlies under the support of Retirement Organization of Tehran Municipality. The subjects were randomly selected based on their pension code. Inclusion criteria were ≥60 years of age, willingness to participate in the study, the ability to answer the questions and communicate, and being retired from Tehran Municipality. Returning incomplete questionnaires and post-sampling mortality were the exclusion criteria. The data collection tool was a 2-part questionnaire.
The first part surveyed sociodemographic and medical profile of the samples. The second part was the Geriatric Oral Health Assessment Index (GOHAI), designed by Atchison and Dolan [4]. In many studies, the validity and reliability of this tool have been validated, and has been used as an instrument for assessing the oral health in elderly [5, 6]. The validity and reliability of its Persian version has been examined by Rezaei and colleagues [7]. It has 12 items scored based on a 5-point Likert-type scale (1=never; 2=seldom; 3=sometimes; 4=often; 5=always). Its total score ranges from 12 to 60. A higher score indicates better oral health, and vice versa. Questionnaires were completed by the researcher using face-to-face interviewing. This study was approved by the Ethics Committee of University of Social Welfare and Rehabilitation Sciences (code: IR.USWR.REC.1395.48).
3. Results
Of 158 samples, 90 (57%) were male and 68 (43%) female. Their Mean±SD age was 68.78±5.45 years. In terms of education, 27 (17.1%) were illiterate, 52 (32.9%) had primary school education, 37 (23.4%) middle school level of education, 26 (16.5%) high school level of education, 8 (5.1%) had associate degree, and 8 (5.1%) had bachelor degree or higher. In terms of oral health behaviors, 29 (18.4%) washed their mouths once a day, 47 (29.7%) twice a day, 56 (35.4%) 3 times a day, 18 (11.4%) more than 3 times a day, and 8 (5.1%) reported that they did not wash their mouths and teeth.
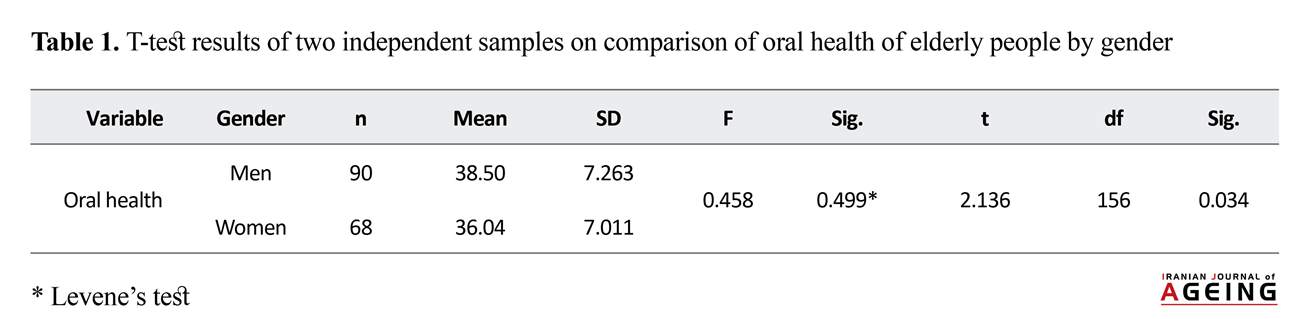
The mean oral health score of samples was 37.44 indicating their moderate level of oral health. There was a negative and significant correlation between the subjects’ oral health and age (P=0.04). This finding indicates that those with higher ages, had worse oral health and vice versa. Moreover, the results suggest that those with higher education level have better oral health. Those with primary education had poor oral health, compared to those with the higher levels of education. According to t-test results, oral health status between men and women was different and elder men had better oral health status. The mean oral health score in men was 38.5, and in elder women it was 36.4 (Table 1).
4. Conclusion
The oral health of elderly people had a significant and negative relationship with their age. With the increase in age, factors such as physical limitations and reduced social relations, make elderly people pay less attention to their oral health. This could contribute to the worsening of oral health status in elderly people. Oral health in elderly men was better than that in elderly women. Throughout their lives, women face severe bio-psychological conditions like fertility and multiple births which greatly impact their oral and dental health. Oral and dental health are important in improving the quality of life in the elderly. Therefore, in designing interventions to promote their oral health, authorities should pay attention to the elderlies’ demographic characteristics.
Ethical Considerations
Compliance with ethical guidelines
This study has been approved by the Research Ethics Committee of University of Social Welfare and Rehabilitation Sciences (code: IR.USWR.REC.1395.48)
1. Objectives
In recent years, there has been a rapid growth of the elderly population in Iran. According to 2016 national census, with 9.3% of Iranian people aged ≥60 years, Iranian population has become older [1]. Oral health of the elderly is a major public health issue calling for more attention worldwide. With the increase in the elderly population, the prevalence of oral and dental problems increases [2]. The factors associated with oral health vary because of socioeconomic and cultural differences among the elderly in different societies [3]. Several studies in Iran investigated the oral health status of elderly and its relationship with their quality of life and knowledge. However, information is scarce about the relationship between their oral health and demographic characteristics. This study aimed to investigate the association between these 2 variables among retired elderly people in Iran.
2. Methods and Materials
This cross-sectional study was conducted on 158 retired elderlies under the support of Retirement Organization of Tehran Municipality. The subjects were randomly selected based on their pension code. Inclusion criteria were ≥60 years of age, willingness to participate in the study, the ability to answer the questions and communicate, and being retired from Tehran Municipality. Returning incomplete questionnaires and post-sampling mortality were the exclusion criteria. The data collection tool was a 2-part questionnaire.
The first part surveyed sociodemographic and medical profile of the samples. The second part was the Geriatric Oral Health Assessment Index (GOHAI), designed by Atchison and Dolan [4]. In many studies, the validity and reliability of this tool have been validated, and has been used as an instrument for assessing the oral health in elderly [5, 6]. The validity and reliability of its Persian version has been examined by Rezaei and colleagues [7]. It has 12 items scored based on a 5-point Likert-type scale (1=never; 2=seldom; 3=sometimes; 4=often; 5=always). Its total score ranges from 12 to 60. A higher score indicates better oral health, and vice versa. Questionnaires were completed by the researcher using face-to-face interviewing. This study was approved by the Ethics Committee of University of Social Welfare and Rehabilitation Sciences (code: IR.USWR.REC.1395.48).
3. Results
Of 158 samples, 90 (57%) were male and 68 (43%) female. Their Mean±SD age was 68.78±5.45 years. In terms of education, 27 (17.1%) were illiterate, 52 (32.9%) had primary school education, 37 (23.4%) middle school level of education, 26 (16.5%) high school level of education, 8 (5.1%) had associate degree, and 8 (5.1%) had bachelor degree or higher. In terms of oral health behaviors, 29 (18.4%) washed their mouths once a day, 47 (29.7%) twice a day, 56 (35.4%) 3 times a day, 18 (11.4%) more than 3 times a day, and 8 (5.1%) reported that they did not wash their mouths and teeth.
The mean oral health score of samples was 37.44 indicating their moderate level of oral health. There was a negative and significant correlation between the subjects’ oral health and age (P=0.04). This finding indicates that those with higher ages, had worse oral health and vice versa. Moreover, the results suggest that those with higher education level have better oral health. Those with primary education had poor oral health, compared to those with the higher levels of education. According to t-test results, oral health status between men and women was different and elder men had better oral health status. The mean oral health score in men was 38.5, and in elder women it was 36.4 (Table 1).
4. Conclusion
The oral health of elderly people had a significant and negative relationship with their age. With the increase in age, factors such as physical limitations and reduced social relations, make elderly people pay less attention to their oral health. This could contribute to the worsening of oral health status in elderly people. Oral health in elderly men was better than that in elderly women. Throughout their lives, women face severe bio-psychological conditions like fertility and multiple births which greatly impact their oral and dental health. Oral and dental health are important in improving the quality of life in the elderly. Therefore, in designing interventions to promote their oral health, authorities should pay attention to the elderlies’ demographic characteristics.
Ethical Considerations
Compliance with ethical guidelines
This study has been approved by the Research Ethics Committee of University of Social Welfare and Rehabilitation Sciences (code: IR.USWR.REC.1395.48)
Funding
The present paper was extracted from the MSc. thesis of the first author in Department of Ageing, University of Social Welfare and Rehabilitation Sciences.
Authors contributions
All authors contributed in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank Deputy of Research and Technology, department of Gerontology at University of Social Welfare and Rehabilitation Sciences, and Retirement Organization of Tehran Municipality for their valuable cooperation.
The present paper was extracted from the MSc. thesis of the first author in Department of Ageing, University of Social Welfare and Rehabilitation Sciences.
Authors contributions
All authors contributed in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank Deputy of Research and Technology, department of Gerontology at University of Social Welfare and Rehabilitation Sciences, and Retirement Organization of Tehran Municipality for their valuable cooperation.
References
- Mokhberi A, Nedae Fard A, Sahaf R. [Barriers and facilitators of Iranian elderly in use of ATM machines: A qualitative research in the way of cultural probes (Persian)]. Iranian Journal of Ageing. 2013; 8(3):17-24.
- World Health Organization. World report on ageing and health 2015. Geneva: World Health Organization; 2015.
- Motallebnejad M, Mehdizadeh S, Najafi N, Sayyadi F. The evaluation of oral health-related factors on the quality of life of the elderly in Babol. Contemporary Clinical Dentistry. 2015; 6(3):313-7. [DOI:10.4103/0976-237X.161867] [PMID] [PMCID]
- United Nations. World population ageing: 1950-2050. New York: United Nations; 2015.
- Rodakowska E, Mierzyńska K, Bagińska J, Jamiołkowski J. Quality of life measured by OHIP-14 and GOHAI in elderly people from Bialystok, north-east Poland. BMC Oral Health. 2014; 14(1):106. [DOI:10.1186/1472-6831-14-106] [PMID] [PMCID]
- Locker D. Dental status, xerostomia and the oral health related quality of life of an elderly institutionalized population. Special Care in Dentistry. 2003; 23(3):86-93. [DOI:10.1111/j.1754-4505.2003.tb01667.x] [PMID]
- McGrath C. Oral health behind bars: A study of oral disease and its impact on the life quality of an older prison population. Gerodontology. 2002; 19(2):109-14. [PMID]
- Petersen PE, Kandelman D, Arpin S, Ogawa H. Global oral health of older people-call for public health action. Community Dental Health. 2010; 27(4):257-67. [PMID]
- Ettinger RL. Oral health and the aging population. The Journal of the American Dental Association. 2007; 138:S5-6. [DOI:10.14219/jada.archive.2007.0357]
- Coleman P. Improving oral health care for the frail elderly: a review of widespread problems and best practices. Geriatric Nursing. 2002; 23(4):189-98. [DOI:10.1067/mgn.2002.126964] [PMID]
- Azarpazhooh A, Leake JL. Systematic review of the association between respiratory diseases and oral health. Journal of Periodontology. 2006; 77(9):1465-82. [DOI:10.1902/jop.2006.060010] [PMID]
- Tuominen R, Reunanen A, Paunio M, Paunio I, Aromaa A. Oral health indicators poorly predict coronary heart disease deaths. Journal of Dental Research. 2003; 82(9):713-8. [DOI:10.1177/154405910308200911] [PMID]
- De Marchi RJ, Hugo FN, Hilgert JB, Padilha DM. Association between oral health status and nutritional status in South Brazilian independent-living older people. Nutrition. 2008; 24(6):546-53. [DOI:10.1016/j.nut.2008.01.054] [PMID]
- Beck JD, Offenbacher S. The association between periodontal diseases and cardiovascular diseases: A state-of-the-science review. Annals of Periodontology. 2001; 6(1):9-15. [DOI:10.1902/annals.2001.6.1.9] [PMID]
- Hung HC, Joshipura KJ, Colditz G, Manson JE, Rimm EB, Speizer FE, Willett WC. The association between tooth loss and coronary heart disease in men and women. Journal of Public Health Dentistry. 2004; 64(4):209-15. [DOI:10.1111/j.1752-7325.2004.tb02755.x] [PMID]
- Lee KS, Kim EK, Kim JW, Choi YH, Mechant AT, Song KB, et al. The relationship between metabolic conditions and prevalence of periodontal disease in rural Korean elderly. Archives of Gerontology and Geriatrics. 2014; 58(1):125-9. [DOI:10.1016/j.archger.2013.08.011] [PMID]
- Southerland JH. Periodontitis may contribute to poor control of hypertension in older adults. Journal of Evidence Based Dental Practice. 2013; 13(3):125-7. [DOI:10.1016/j.jebdp.2013.07.016] [PMID]
- Taylor GW, Loesche WJ, Terpenning MS. Impact of oral diseases on systemic health in the elderly: Diabetes mellitus and aspiration pneumonia. Journal of Public Health Dentistry. 2000; 60(4):313-20. [DOI:10.1111/j.1752-7325.2000.tb03341.x] [PMID]
- Hassel AJ, Koke U, Schmitter M, Rammelsberg P. Factors associated with oral health-related quality of life in institutionalized elderly. Acta Odontologica Scandinavica. 2006; 64(1):9-15.[DOI:10.1080/00016350500326211] [PMID]
- Hajiebrahimi MH, Charkazi A, Rastgarimehr B, Homayonpour A, Hajiebrahimi Z, Mansourian M, et al. Oral health situation in elder people in Gorgan City. Iranian journal of Diabetes and Metabolism. 2014; 13(6):505-12.
- Khadem P, Jabbarifar E, Maroofi V, Feiz A. The effect of using dentures in the improvement of lifestyle among the elderly population of Isfahan, Iran. Journal of Isfahan Dental School. 2009; 5(3): 148-155.
- Rabiei M, Masoudirad H, Javadinia A. Dental status among urban and rural elderly of Talesh (2009). Iranian Journal of Medical Sciences. 2012; 60(3):69-75.
- Atchison KA, Dolan TA. Development of the geriatric oral health assessment index. Journal of Dental Education. 1990; 54(11):680-7. [PMID]
- Locker D, Matear D, Stephens M, Lawrence H, Payne B. Comparison of the GOHAI and OHIP 14 as measures of the oral health related quality of life of the elderly. Community Dentistry and Oral Epidemiology. 2001; 29(5):373-81. [DOI:10.1111/j.1600-0528.2001.290507.x] [PMID]
- El Osta N, Tubert-Jeannin S, Hennequin M, Naaman NB, El Osta L, Geahchan N. Comparison of the OHIP-14 and GOHAI as measures of oral health among elderly in Lebanon. Health and Quality of Life Outcomes. 2012; 10(1):131. [DOI:10.1186/1477-7525-10-131] [PMID] [PMCID]
- Rezaei M, Rashedi V, Khedmati Morasae E. A Persian version of Geriatric Oral Health Assessment Index. Gerodontology. 2016; 33(3):335-41. [DOI:10.1111/ger.12161] [PMID]
- Nicolau B, Srisilapana P, Marcenes W. Number of teeth and risk of root caries. Gerodontology. 2000; 17(2):91-6. [DOI:10.1111/j.1741-2358.2000.00091.x] [PMID]
- Lukacs JR. Sex differences in dental caries experience: Clinical evidence, complex etiology. Clinical Oral Investigations. 2011; 15(5):649-56. [DOI:10.1007/s00784-010-0445-3] [PMID]
- Acharya S, Bhat PV, Acharya S. Factors affecting oral healthrelated quality of life among pregnant women. International Journal of Dental Hygiene. 2009; 7(2):102-7. [DOI:10.1111/j.1601-5037.2008.00351.x] [PMID]
- Shah N, Sundaram KR. Impact of socio demographic variables, oral hygiene practices, oral habits and diet on dental caries experience of Indian elderly: a community based study. Gerodontology. 2004; 21(1):43-50. [DOI:10.1111/j.1741-2358.2004.00010.x] [PMID]
- Hernández-Palacios RD, Ramírez-Amador V, Jarillo-Soto EC, Irigoyen-Camacho ME, Mendoza-Nú-ez VM. Relationship between gender, income and education and self-perceived oral health among elderly Mexicans: An exploratory study. Ciencia & Saude Coletiva. 2015; 20(4):997-1004. [DOI:10.1590/1413-81232015204.00702014] [PMID]
- Paulander J, Axelsson P, Lindhe J. Association between level of education and oral health status in 35-, 50-, 65- and 75-year-olds. Journal of Clinical Periodontology. 2003; 30(8):697-704. [DOI:10.1034/j.1600-051X.2003.00357.x] [PMID]
- Tsakos G, Sheiham A, Iliffe S, Kharicha K, Harari D, Swift CG, et al. The impact of educational level on oral health-related quality of life in older people in London. European Journal of Oral Sciences. 2009; 117(3):286-92. [DOI:10.1111/j.1600-0722.2009.00619.x] [PMID]
- Modanloo MM, Khosravee H, Ghobadee K, Abdollahi H, Ziaea T, Behnampour N. Dental health status in elderly (Gorgan-Iran). Journal of Gorgan University of Medical Sciences. 2010; 12(3):68-73.
Type of Study: Research |
Subject:
gerontology
Received: 2018/08/08 | Accepted: 2018/11/29 | Published: 2019/01/01
Received: 2018/08/08 | Accepted: 2018/11/29 | Published: 2019/01/01
References
1. Mokhberi A, Nedae Fard A, Sahaf R. [Barriers and facilitators of Iranian elderly in use of ATM machines: A qualitative research in the way of cultural probes (Persian)]. Iranian Journal of Ageing. 2013; 8(3):17-24.
2. World Health Organization. World report on ageing and health 2015. Geneva: World Health Organization; 2015.
3. Motallebnejad M, Mehdizadeh S, Najafi N, Sayyadi F. The evaluation of oral health-related factors on the quality of life of the elderly in Babol. Contemporary Clinical Dentistry. 2015; 6(3):313-7. [DOI:10.4103/0976-237X.161867] [PMID] [PMCID] [DOI:10.4103/0976-237X.161867]
4. United Nations. World population ageing: 1950-2050. New York: United Nations; 2015.
5. Rodakowska E, Mierzyńska K, Bagińska J, Jamiołkowski J. Quality of life measured by OHIP-14 and GOHAI in elderly people from Bialystok, north-east Poland. BMC Oral Health. 2014; 14(1):106. [DOI:10.1186/1472-6831-14-106] [PMID] [PMCID] [DOI:10.1186/1472-6831-14-106]
6. Locker D. Dental status, xerostomia and the oral health related quality of life of an elderly institutionalized population. Special Care in Dentistry. 2003; 23(3):86-93. [DOI:10.1111/j.1754-4505.2003.tb01667.x] [PMID] [DOI:10.1111/j.1754-4505.2003.tb01667.x]
7. McGrath C. Oral health behind bars: A study of oral disease and its impact on the life quality of an older prison population. Gerodontology. 2002; 19(2):109-14. [PMID] [DOI:10.1111/j.1741-2358.2002.00109.x] [PMID]
8. Petersen PE, Kandelman D, Arpin S, Ogawa H. Global oral health of older people-call for public health action. Community Dental Health. 2010; 27(4):257-67. [PMID] [PMID]
9. Ettinger RL. Oral health and the aging population. The Journal of the American Dental Association. 2007; 138:S5-6. [DOI:10.14219/jada.archive.2007.0357] [DOI:10.14219/jada.archive.2007.0357]
10. Coleman P. Improving oral health care for the frail elderly: a review of widespread problems and best practices. Geriatric Nursing. 2002; 23(4):189-98. [DOI:10.1067/mgn.2002.126964] [PMID] [DOI:10.1067/mgn.2002.126964]
11. Azarpazhooh A, Leake JL. Systematic review of the association between respiratory diseases and oral health. Journal of Periodontology. 2006; 77(9):1465-82. [DOI:10.1902/jop.2006.060010] [PMID] [DOI:10.1902/jop.2006.060010]
12. Tuominen R, Reunanen A, Paunio M, Paunio I, Aromaa A. Oral health indicators poorly predict coronary heart disease deaths. Journal of Dental Research. 2003; 82(9):713-8. [DOI:10.1177/154405910308200911] [PMID] [DOI:10.1177/154405910308200911]
13. De Marchi RJ, Hugo FN, Hilgert JB, Padilha DM. Association between oral health status and nutritional status in South Brazilian independent-living older people. Nutrition. 2008; 24(6):546-53. [DOI:10.1016/j.nut.2008.01.054] [PMID] [DOI:10.1016/j.nut.2008.01.054]
14. Beck JD, Offenbacher S. The association between periodontal diseases and cardiovascular diseases: A state-of-the-science review. Annals of Periodontology. 2001; 6(1):9-15. [DOI:10.1902/annals.2001.6.1.9] [PMID] [DOI:10.1902/annals.2001.6.1.9]
15. Hung HC, Joshipura KJ, Colditz G, Manson JE, Rimm EB, Speizer FE, Willett WC. The association between tooth loss and coronary heart disease in men and women. Journal of Public Health Dentistry. 2004; 64(4):209-15. [DOI:10.1111/j.1752-7325.2004.tb02755.x] [PMID] [DOI:10.1111/j.1752-7325.2004.tb02755.x]
16. Lee KS, Kim EK, Kim JW, Choi YH, Mechant AT, Song KB, et al. The relationship between metabolic conditions and prevalence of periodontal disease in rural Korean elderly. Archives of Gerontology and Geriatrics. 2014; 58(1):125-9. [DOI:10.1016/j.archger.2013.08.011] [PMID] [DOI:10.1016/j.archger.2013.08.011]
17. Southerland JH. Periodontitis may contribute to poor control of hypertension in older adults. Journal of Evidence Based Dental Practice. 2013; 13(3):125-7. [DOI:10.1016/j.jebdp.2013.07.016] [PMID] [DOI:10.1016/j.jebdp.2013.07.016]
18. Taylor GW, Loesche WJ, Terpenning MS. Impact of oral diseases on systemic health in the elderly: Diabetes mellitus and aspiration pneumonia. Journal of Public Health Dentistry. 2000; 60(4):313-20. [DOI:10.1111/j.1752-7325.2000.tb03341.x] [PMID] [DOI:10.1111/j.1752-7325.2000.tb03341.x]
19. Hassel AJ, Koke U, Schmitter M, Rammelsberg P. Factors associated with oral health-related quality of life in institutionalized elderly. Acta Odontologica Scandinavica. 2006; 64(1):9-15.[DOI:10.1080/00016350500326211] [PMID] [DOI:10.1080/00016350500326211]
20. Hajiebrahimi MH, Charkazi A, Rastgarimehr B, Homayonpour A, Hajiebrahimi Z, Mansourian M, et al. Oral health situation in elder people in Gorgan City. Iranian journal of Diabetes and Metabolism. 2014; 13(6):505-12.
21. Khadem P, Jabbarifar E, Maroofi V, Feiz A. The effect of using dentures in the improvement of lifestyle among the elderly population of Isfahan, Iran. Journal of Isfahan Dental School. 2009; 5(3): 148-155.
22. Rabiei M, Masoudirad H, Javadinia A. Dental status among urban and rural elderly of Talesh (2009). Iranian Journal of Medical Sciences. 2012; 60(3):69-75.
23. Atchison KA, Dolan TA. Development of the geriatric oral health assessment index. Journal of Dental Education. 1990; 54(11):680-7. [PMID] [PMID]
24. Locker D, Matear D, Stephens M, Lawrence H, Payne B. Comparison of the GOHAI and OHIP 14 as measures of the oral health related quality of life of the elderly. Community Dentistry and Oral Epidemiology. 2001; 29(5):373-81. [DOI:10.1111/j.1600-0528.2001.290507.x] [PMID] [DOI:10.1111/j.1600-0528.2001.290507.x]
25. El Osta N, Tubert-Jeannin S, Hennequin M, Naaman NB, El Osta L, Geahchan N. Comparison of the OHIP-14 and GOHAI as measures of oral health among elderly in Lebanon. Health and Quality of Life Outcomes. 2012; 10(1):131. [DOI:10.1186/1477-7525-10-131] [PMID] [PMCID] [DOI:10.1186/1477-7525-10-131]
26. Rezaei M, Rashedi V, Khedmati Morasae E. A Persian version of Geriatric Oral Health Assessment Index. Gerodontology. 2016; 33(3):335-41. [DOI:10.1111/ger.12161] [PMID] [DOI:10.1111/ger.12161]
27. Nicolau B, Srisilapana P, Marcenes W. Number of teeth and risk of root caries. Gerodontology. 2000; 17(2):91-6. [DOI:10.1111/j.1741-2358.2000.00091.x] [PMID] [DOI:10.1111/j.1741-2358.2000.00091.x]
28. Lukacs JR. Sex differences in dental caries experience: Clinical evidence, complex etiology. Clinical Oral Investigations. 2011; 15(5):649-56. [DOI:10.1007/s00784-010-0445-3] [PMID] [DOI:10.1007/s00784-010-0445-3]
29. Acharya S, Bhat PV, Acharya S. Factors affecting oral healthrelated quality of life among pregnant women. International Journal of Dental Hygiene. 2009; 7(2):102-7. [DOI:10.1111/j.1601-5037.2008.00351.x] [PMID] [DOI:10.1111/j.1601-5037.2008.00351.x]
30. Shah N, Sundaram KR. Impact of socio demographic variables, oral hygiene practices, oral habits and diet on dental caries experience of Indian elderly: a community based study. Gerodontology. 2004; 21(1):43-50. [DOI:10.1111/j.1741-2358.2004.00010.x] [PMID] [DOI:10.1111/j.1741-2358.2004.00010.x]
31. Hernández-Palacios RD, Ramírez-Amador V, Jarillo-Soto EC, Irigoyen-Camacho ME, Mendoza-Nú-ez VM. Relationship between gender, income and education and self-perceived oral health among elderly Mexicans: An exploratory study. Ciencia & Saude Coletiva. 2015; 20(4):997-1004. [DOI:10.1590/1413-81232015204.00702014] [PMID] [DOI:10.1590/1413-81232015204.00702014]
32. Paulander J, Axelsson P, Lindhe J. Association between level of education and oral health status in 35-, 50-, 65- and 75-year-olds. Journal of Clinical Periodontology. 2003; 30(8):697-704. [DOI:10.1034/j.1600-051X.2003.00357.x] [PMID] [DOI:10.1034/j.1600-051X.2003.00357.x]
33. Tsakos G, Sheiham A, Iliffe S, Kharicha K, Harari D, Swift CG, et al. The impact of educational level on oral health-related quality of life in older people in London. European Journal of Oral Sciences. 2009; 117(3):286-92. [DOI:10.1111/j.1600-0722.2009.00619.x] [PMID] [DOI:10.1111/j.1600-0722.2009.00619.x]
34. Modanloo MM, Khosravee H, Ghobadee K, Abdollahi H, Ziaea T, Behnampour N. Dental health status in elderly (Gorgan-Iran). Journal of Gorgan University of Medical Sciences. 2010; 12(3):68-73.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |