Volume 14, Issue 4 (Winter 2020)
Salmand: Iranian Journal of Ageing 2020, 14(4): 380-391 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fadayevatan R, Bahrami M, Mohamadzadeh M, Borhaninejad V. Relationship of Sleep Quality with Mental Health and Blood Sugar Control in Elderly People with Diabetes Mellitus. Salmand: Iranian Journal of Ageing 2020; 14 (4) :380-391
URL: http://salmandj.uswr.ac.ir/article-1-1532-en.html
URL: http://salmandj.uswr.ac.ir/article-1-1532-en.html
1- Iranian Research Center on Aging, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Faculty of Nursing and Midwifery, Islamic Azad University, Shahr-e Babak Branch, Kerman, Iran.
3- School of Health, North Khorasan University of Medical Sciences, North Khorasan, Iran.
4- Social Determinants of Health Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran. ,v.borhaninejad@kmu.ac.ir
2- Faculty of Nursing and Midwifery, Islamic Azad University, Shahr-e Babak Branch, Kerman, Iran.
3- School of Health, North Khorasan University of Medical Sciences, North Khorasan, Iran.
4- Social Determinants of Health Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran. ,
Full-Text [PDF 4506 kb]
(3433 Downloads)
| Abstract (HTML) (8959 Views)
Full-Text: (3474 Views)
Extended Abstract
1. Introduction
Diabetes, as the most common hormone deficiency in the elderly people, can lead to many physical and psychological problems in this population [1]. One of the most common problems caused by diabetes is sleep disorder, which puts patients at greater risk of sleep disorders compared to the normal population [2]. Sleep disorder has been reported to be associated with an increased incidence of diabetes or inadequate blood sugar control in diabetic patients [3-5]. Sleep quality in older people with diabetes may also be impaired due to psychological problems such as depression [6, 7]. Investigating the factors affecting the sleep quality of older people can have an effective role in providing non-pharmaceutical solutions for this group and improving their sleep quality. In this regard, this study aimed to examine association of sleep quality with mental health and blood sugar control in elderly people with diabetes.
2. Materials and Methods
This is cross-sectional study conducted in 2017. The study population consisted of all seniors with diabetes aged >60 referred to Shahid Bahonar and Shafa hospitals in Kerman, Iran. Samples were selected using a convenience sampling technique. The sample size was determined 200 using formula. Data were collected using the Kessler Psychological Distress Scale (K6), Yield questionnaire and Pittsburgh Sleep Quality Index (PSQI) questionnaire. The validity and reliability of these questionnaires for Iranian population have already been examined and confirmed [8-12]. glycated hemoglobin(HbA1c) level recorded in patients’ files was used to monitor blood glucose control. In this regard, HbA1c<7% was considered as proper control and HbA1c>7% represents poor control [12].
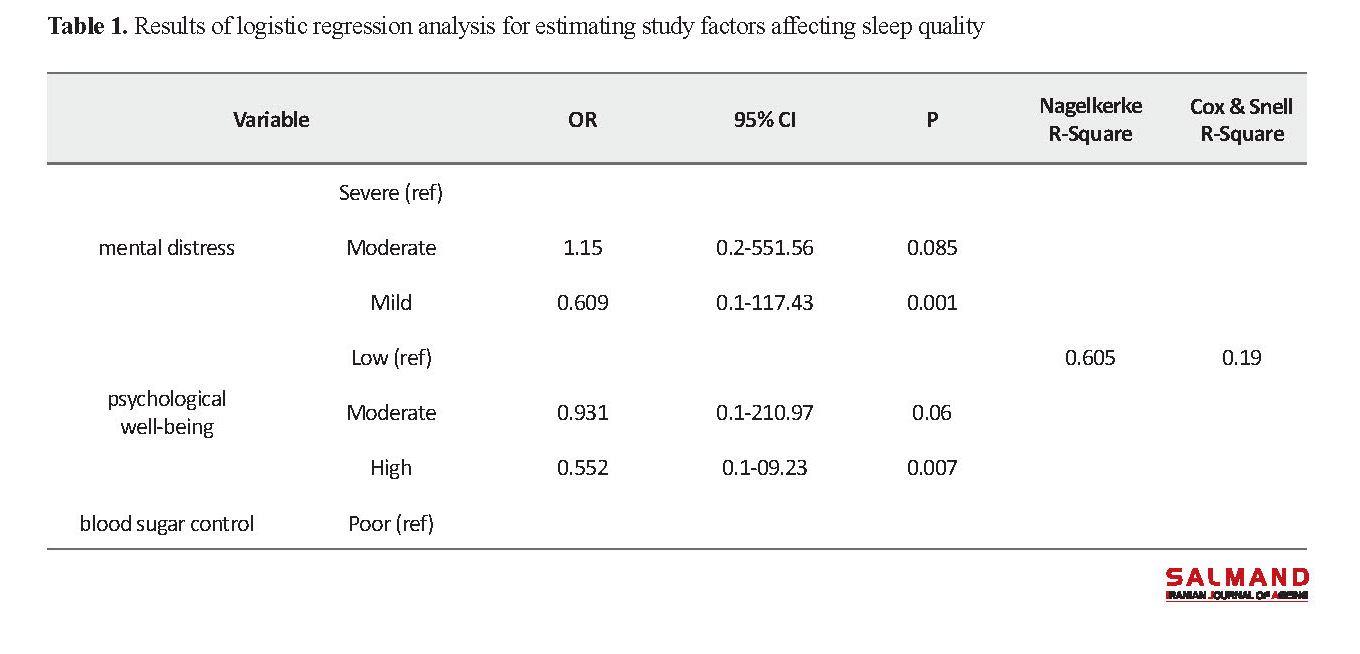
To test the relationship of demographic variables with mental health and sleep quality, Chi-square and Pearson correlation tests were used, and to compare sleep quality (nominal level independent variable) in terms of mental health and blood sugar control, multivariate logistic regression analysis was employed. In the regression model, the Independent variables of mental distress, psychological wellbeing, and blood sugar control were entered. Since in the univariate analysis, all three independent variables had a significance level of less than 0.2, It can be said that they are able to predict dependent variable changes (sleep quality). Therefore, in the final regression model, independent variables were entered into the model simultaneously and the analysis was performed using multivariate logistic regression analysis in SPSS V. 21 software.
3. Results
The mean age of participants was 69.33±9.65 years. Most of them were female (n=98, 55.4%), married (n=139, 78.8%), illiterate or primary education (n=99, 55.9%), and had disease for more than 10 years (n=102, 57. 6%).The majority of them were treating with taking pills and insulin (n=107, 60.5%). Moreover, most of were taking sleeping pills (n=121, 68.4%), where benzodiazepine was the most common used pill (75.3%). According to the K6 scale scores, most of participants had moderate mental distress (54.8%) and psychological wellbeing (46.3%), and poor blood sugar control (65.5%). Moreover, most of participants had poor sleep quality (63.8%). Age (r=0.309, P=0.001), marital status (P<0001), gender (P=0.02), and duration of disease (P=0.003) had a significant relationship with sleep quality. Lower mental distress, higher psychological well-being, and more favorable blood sugar control are protective factors against sleep disorders. Based on the results of regression analysis, seniors with low mental distress were 40% more likely (P<0.001) and those with high psychological well-being were 45% more likely to have a good sleep quality than compared to other subjects (P= 0.007). Moreover, odds of favorable sleep quality were 48% higher for those with proper blood sugar control compared to those with poor control (P<0.001). Overall, mental distress, psychological well-being, and more blood sugar control could explain only 19% of sleep disorders.
4. Conclusion
The findings of this study indicated the effect of mental health and optimal blood sugar control on the prevention of sleep disorders in the elderly people. Given the increasing population of older people and the higher prevalence of diabetes in them, attention to diabetes control and improvement of their mental health and sleep quality should be considered by health care policy makers. It is recommended that in addition to adopting self-care strategies, mental health services should be provided to these patients along with other services they receive. It is also necessary to improve the quality of sleep in diabetic elderly people using effective non-pharmacological methods such as sleep health education. Regarding the importance of sleep disorder, interventional studies are recommended to investigate the effect of psychological and educational interventions and further studies should be conducted on other factors affecting sleep disorders.
1. Introduction
Diabetes, as the most common hormone deficiency in the elderly people, can lead to many physical and psychological problems in this population [1]. One of the most common problems caused by diabetes is sleep disorder, which puts patients at greater risk of sleep disorders compared to the normal population [2]. Sleep disorder has been reported to be associated with an increased incidence of diabetes or inadequate blood sugar control in diabetic patients [3-5]. Sleep quality in older people with diabetes may also be impaired due to psychological problems such as depression [6, 7]. Investigating the factors affecting the sleep quality of older people can have an effective role in providing non-pharmaceutical solutions for this group and improving their sleep quality. In this regard, this study aimed to examine association of sleep quality with mental health and blood sugar control in elderly people with diabetes.
2. Materials and Methods
This is cross-sectional study conducted in 2017. The study population consisted of all seniors with diabetes aged >60 referred to Shahid Bahonar and Shafa hospitals in Kerman, Iran. Samples were selected using a convenience sampling technique. The sample size was determined 200 using formula. Data were collected using the Kessler Psychological Distress Scale (K6), Yield questionnaire and Pittsburgh Sleep Quality Index (PSQI) questionnaire. The validity and reliability of these questionnaires for Iranian population have already been examined and confirmed [8-12]. glycated hemoglobin(HbA1c) level recorded in patients’ files was used to monitor blood glucose control. In this regard, HbA1c<7% was considered as proper control and HbA1c>7% represents poor control [12].
To test the relationship of demographic variables with mental health and sleep quality, Chi-square and Pearson correlation tests were used, and to compare sleep quality (nominal level independent variable) in terms of mental health and blood sugar control, multivariate logistic regression analysis was employed. In the regression model, the Independent variables of mental distress, psychological wellbeing, and blood sugar control were entered. Since in the univariate analysis, all three independent variables had a significance level of less than 0.2, It can be said that they are able to predict dependent variable changes (sleep quality). Therefore, in the final regression model, independent variables were entered into the model simultaneously and the analysis was performed using multivariate logistic regression analysis in SPSS V. 21 software.
3. Results
The mean age of participants was 69.33±9.65 years. Most of them were female (n=98, 55.4%), married (n=139, 78.8%), illiterate or primary education (n=99, 55.9%), and had disease for more than 10 years (n=102, 57. 6%).The majority of them were treating with taking pills and insulin (n=107, 60.5%). Moreover, most of were taking sleeping pills (n=121, 68.4%), where benzodiazepine was the most common used pill (75.3%). According to the K6 scale scores, most of participants had moderate mental distress (54.8%) and psychological wellbeing (46.3%), and poor blood sugar control (65.5%). Moreover, most of participants had poor sleep quality (63.8%). Age (r=0.309, P=0.001), marital status (P<0001), gender (P=0.02), and duration of disease (P=0.003) had a significant relationship with sleep quality. Lower mental distress, higher psychological well-being, and more favorable blood sugar control are protective factors against sleep disorders. Based on the results of regression analysis, seniors with low mental distress were 40% more likely (P<0.001) and those with high psychological well-being were 45% more likely to have a good sleep quality than compared to other subjects (P= 0.007). Moreover, odds of favorable sleep quality were 48% higher for those with proper blood sugar control compared to those with poor control (P<0.001). Overall, mental distress, psychological well-being, and more blood sugar control could explain only 19% of sleep disorders.
4. Conclusion
The findings of this study indicated the effect of mental health and optimal blood sugar control on the prevention of sleep disorders in the elderly people. Given the increasing population of older people and the higher prevalence of diabetes in them, attention to diabetes control and improvement of their mental health and sleep quality should be considered by health care policy makers. It is recommended that in addition to adopting self-care strategies, mental health services should be provided to these patients along with other services they receive. It is also necessary to improve the quality of sleep in diabetic elderly people using effective non-pharmacological methods such as sleep health education. Regarding the importance of sleep disorder, interventional studies are recommended to investigate the effect of psychological and educational interventions and further studies should be conducted on other factors affecting sleep disorders.
Ethical Considerations
Compliance with ethical guidelines
Ethical permission was obtained from the institutional review board of Kerman University of Medical Sciences ( IR.KMU.REC.1396.1380).
Funding
This project was supported by Social Determinants of Health Research Center, Vice Chancellor for Research at the Kerman University of Medical Sciences.
Authors' contributions
Conceptualization, supervision, methodology: Reza Fadayevatan nad Vahidreza Borhaninejad; Writing-original draft, investigation: All author; Writing-review & editing, funding acquisition, resources: Vahidreza Borhaninejad.
Conflicts of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgements
The authors would like to thank the staffs of diabetes-related centers in Kerman for their kind cooperation in this study.
Compliance with ethical guidelines
Ethical permission was obtained from the institutional review board of Kerman University of Medical Sciences ( IR.KMU.REC.1396.1380).
Funding
This project was supported by Social Determinants of Health Research Center, Vice Chancellor for Research at the Kerman University of Medical Sciences.
Authors' contributions
Conceptualization, supervision, methodology: Reza Fadayevatan nad Vahidreza Borhaninejad; Writing-original draft, investigation: All author; Writing-review & editing, funding acquisition, resources: Vahidreza Borhaninejad.
Conflicts of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgements
The authors would like to thank the staffs of diabetes-related centers in Kerman for their kind cooperation in this study.
Type of Study: Research |
Subject:
Psychology
Received: 2018/04/29 | Accepted: 2018/07/09 | Published: 2020/02/29
Received: 2018/04/29 | Accepted: 2018/07/09 | Published: 2020/02/29
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |