Volume 18, Issue 3 (Autumn 2023)
Salmand: Iranian Journal of Ageing 2023, 18(3): 460-473 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Azarmi E, Azadi F, Mosallanezhad Z, Vahedi M. Relationship of Low Back Pain and Knee Pain With Dynamic Balance of the Elderly Living in Nursing Homes in Mashhad, Iran. Salmand: Iranian Journal of Ageing 2023; 18 (3) :460-473
URL: http://salmandj.uswr.ac.ir/article-1-2499-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2499-en.html
1- Department of Physiotherapy, Faculty of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Ageing, Faculty of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,fa.azadi@uswr.ac.ir
3- Ageing Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Ageing, Faculty of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Ageing Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Full-Text [PDF 4188 kb]
(590 Downloads)
| Abstract (HTML) (1457 Views)
Full-Text: (716 Views)
Introduction
The number of aged people in the world is growing, such that, by 2050, the number of older people is expected to increase to about two billion people, equivalent to 15% of the world's population [1]. Iran's population is also moving from a young population to an aged population, such that the proportion of people over 65 years old is expected to increase to 20-25% by 2030 [2]. One of the problems that affects the health of the elderly is the loss of balance while walking, which is known as a strong risk factor of falling in older people [3]. Falling is the second largest cause of unintentional injuries in the US and one of the most important factors in the mortality of the elderly [4]. In addition to falling, the fear of falling again in older people with a history of falling causes loss of confidence, immobility and, subsequently, muscle weakness and limitations in daily activities [5, 6].
Knee pain (KP) and low back pain (LBP) are the most common disabling conditions in the elderly [7]. Knee pain is a common musculoskeletal problem in the elderly, the prevalence of which increases with age [8]. In previous studies, the study of low KP and LBP caused by aging and its effect on balance has been done separately [14-16]. In this study, we aim to assess the relationship of chronic KP and LBP with dynamic balance in the elderly in Iran.
Methods
In this analytical cross-sectional study, 79 older adults aged ≥65 years living in a nursing home in Mashhad, Iran, were selected using the census method and based on the inclusion and exclusion criteria of the study. In addition to measuring demographic information (Age, gender, height and weight), fear of falling was assessed with the Persian version of the falls efficacy scale - international (FES-I), and the pain was assessed using the visual analog scale (VAS). To assess dynamic balance, the timed up & go (TUG) test was used. Data analysis was done in SPSS software, version 23.
Results
The mean values of demographic variables and FES-I score in three groups of healthy, KP, and LBP are given in Table 1.
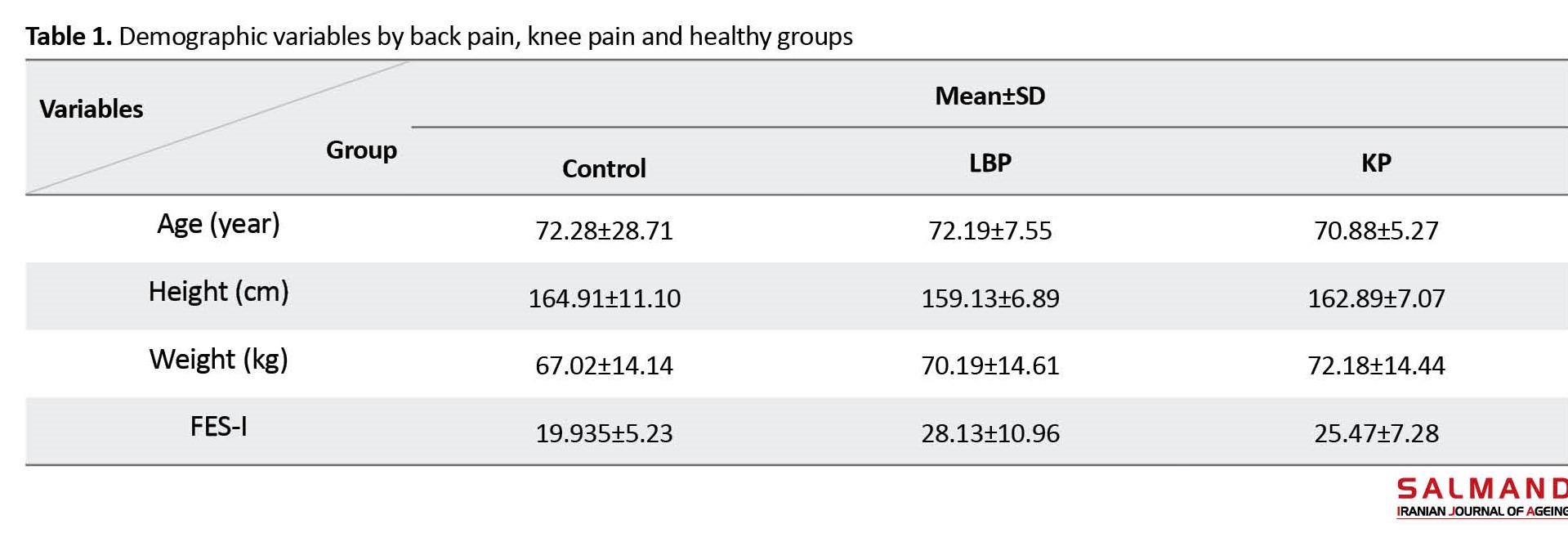
The mean age of the participants was 71.38±5.66. They included 45 (57%) males and 34 (43%) females. The participants included 46 older people (58.2%) in the pain-free group, 16 in the LBP group (20.3%), and 17 in the KP group (21.5%).
According to the Spearman's correlation test results in Table 2, there was a moderate and positive correlation between age and values of TUG test which was statistically significant (P<0.05); with increasing age, the duration of the TUG test increased.
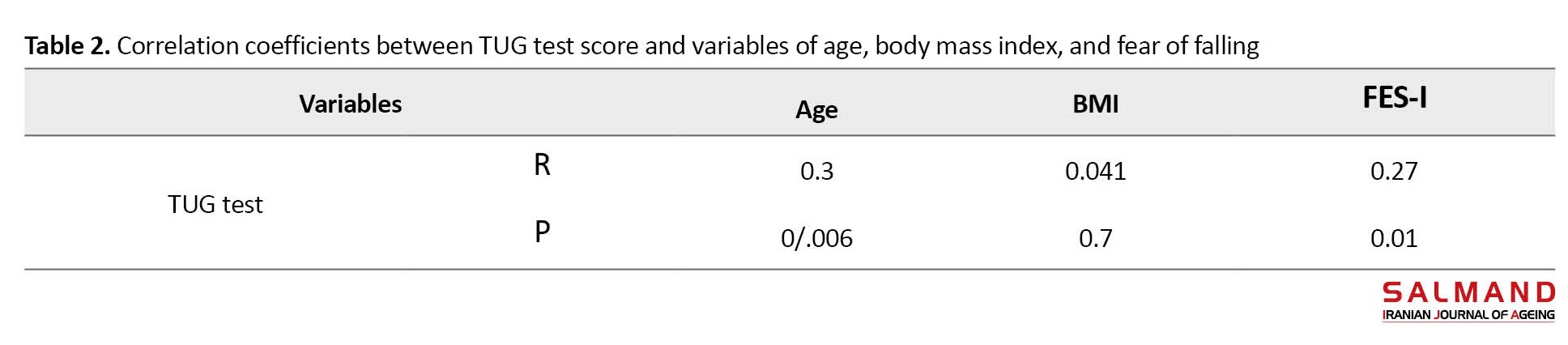
There was a weak and positive correlation between FES-I score and TUG test score and this was statistically significant (P>0.05); with increasing FES-I score, the duration of the TUG test increased. There was a weak and positive correlation between BMI and TUG test score but it was not statistically significant (P>0.05).
By conducting the Mann-Whitney U test, no significant difference was found between men and women in TUG test score (P=0.38). Kruskal-Wallis test results showed that the mean TUG test score was different among the three groups, which were significantly higher in the elderly with KP than those with LBP and healthy people (P=0.05).
Conclusion
The results of this study showed that the mean score of TUG test in older people with KP were significantly higher than in healthy people and those with LBP, which indicates that dynamic balance is poorer in people with KP. Among similar studies, Munch et al. examined the relationship between joint pain and falls in older men. According to their results, any pain in the knee and back joints increases the risk of falling in older men [24]. In the study by Kitayuchi et al., it was found that LBP and KP are associated with the occurrence of falls [25]. The results of these two studies are not consistent with our results, perhaps because they used a questionnaire to evaluate falls. A study for examining the association of KP and LBP with balance test scores has not been conducted so far. In Bennell and Hinman's study on balance disorders in people with knee osteoarthritis compared to the control group, using clinical tests, it was found that the dynamic balance was weaker in the group with knee osteoarthritis [26]. Knee osteoarthritis is one of the causes of KP in the elderly; hence, their results are in line with our results. In the study by Yanardag et al., by investigating the relationship between pain, balance, walking performance and quality of life in elderly people with LBP and KP, the authors found a significant relationship between LBP and KP with the TUG test [27].
In the present study, with increasing age, the TUG test score of older adults increased, i.e. their dynamic balance decreased. Takacs et al. in a study on factors related to dynamic balance in older people with knee osteoarthritis, found that dynamic balance significantly decreased with aging [28]. This is consistent with our results. Kiss et al. examined perturbation-based balance in older adults with varying degrees of knee osteoarthritis. They found no significant relationship between age and static balance in the group with severe knee osteoarthritis. They used the static balance test which can be the reason for the lack of consistency with the present study.
In the present study, with increasing fear of falling, the TUG test score of older adults increased, i.e. their dynamic balance decreased. Ulus et al. and Halaweh et al. also found a positive and significant correlation between the scores of FES-I and TUG test [29, 30]. This is consistent with our results. No significant relationship was found between body mass index and TUG test score. Mohd Said et al, by examining balance in older people and its relationship with physiological factors of the body in different ankle joint conditions, did not find a significant relationship between balance and body mass index [31]. In Gouveia et al.'s study on the demographic characteristics, balance, and mobility of the elderly in Portugal, it was found that balance decreased significantly with an increase in body mass index [32]. The reason for the discrepancy may be the difference in the study area and the lower average age of the participants. In the study by Sarshin et al., a significant relationship was found between body mass index and static and dynamic balances [33]. This discrepancy can be due to in the selection of young subjects and athletes in their study.
In the present study, no significant relationship was found between gender and TUG test score. In the study by Espinoza et al. on postural balance and temporal and spatial factors of gait in older men and women, it was found that the postural balance of older men was poorer than that of older women [35]. This discrepancy can be due to the difference in the measurement tools and the study factors, and balance was not measured with balance tests.
There is a significant difference among the healthy elderly and those with chronic LBP and chronic KP in dynamic balance. The older adults with chronic KP have a poorer dynamic balance. To prevent balance deficits in old age, prevention and treatment of knee injuries should be prioritized by doctors and therapists. Other factors related to balance deficiency in older adults should also be identified.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1400.065). All participants were informed about the study process. They were assured of the confidentiality of their information and were free to leave the study at any time. A written informed consent was obtained from them.
Funding
This article was extracted from the master’s degree of Elham Azarm registered by the Faculty of Rehabilitation, Department of Physiotherapy, University of Social Welfare and Rehabilitation Sciences. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors
Authors' contributions
The authors contributed equally to preparing this paper.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the General Welfare Organization of Khorasan Razavi province, all nursing homes in Mashhad city, and all seniors participated in this study for their cooperation.
References
The number of aged people in the world is growing, such that, by 2050, the number of older people is expected to increase to about two billion people, equivalent to 15% of the world's population [1]. Iran's population is also moving from a young population to an aged population, such that the proportion of people over 65 years old is expected to increase to 20-25% by 2030 [2]. One of the problems that affects the health of the elderly is the loss of balance while walking, which is known as a strong risk factor of falling in older people [3]. Falling is the second largest cause of unintentional injuries in the US and one of the most important factors in the mortality of the elderly [4]. In addition to falling, the fear of falling again in older people with a history of falling causes loss of confidence, immobility and, subsequently, muscle weakness and limitations in daily activities [5, 6].
Knee pain (KP) and low back pain (LBP) are the most common disabling conditions in the elderly [7]. Knee pain is a common musculoskeletal problem in the elderly, the prevalence of which increases with age [8]. In previous studies, the study of low KP and LBP caused by aging and its effect on balance has been done separately [14-16]. In this study, we aim to assess the relationship of chronic KP and LBP with dynamic balance in the elderly in Iran.
Methods
In this analytical cross-sectional study, 79 older adults aged ≥65 years living in a nursing home in Mashhad, Iran, were selected using the census method and based on the inclusion and exclusion criteria of the study. In addition to measuring demographic information (Age, gender, height and weight), fear of falling was assessed with the Persian version of the falls efficacy scale - international (FES-I), and the pain was assessed using the visual analog scale (VAS). To assess dynamic balance, the timed up & go (TUG) test was used. Data analysis was done in SPSS software, version 23.
Results
The mean values of demographic variables and FES-I score in three groups of healthy, KP, and LBP are given in Table 1.
The mean age of the participants was 71.38±5.66. They included 45 (57%) males and 34 (43%) females. The participants included 46 older people (58.2%) in the pain-free group, 16 in the LBP group (20.3%), and 17 in the KP group (21.5%).
According to the Spearman's correlation test results in Table 2, there was a moderate and positive correlation between age and values of TUG test which was statistically significant (P<0.05); with increasing age, the duration of the TUG test increased.
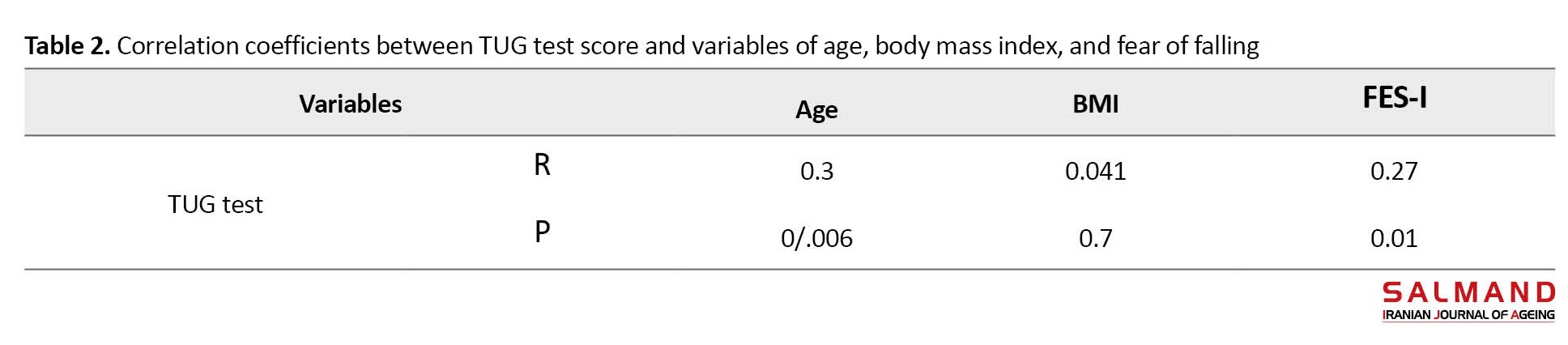
There was a weak and positive correlation between FES-I score and TUG test score and this was statistically significant (P>0.05); with increasing FES-I score, the duration of the TUG test increased. There was a weak and positive correlation between BMI and TUG test score but it was not statistically significant (P>0.05).
By conducting the Mann-Whitney U test, no significant difference was found between men and women in TUG test score (P=0.38). Kruskal-Wallis test results showed that the mean TUG test score was different among the three groups, which were significantly higher in the elderly with KP than those with LBP and healthy people (P=0.05).
Conclusion
The results of this study showed that the mean score of TUG test in older people with KP were significantly higher than in healthy people and those with LBP, which indicates that dynamic balance is poorer in people with KP. Among similar studies, Munch et al. examined the relationship between joint pain and falls in older men. According to their results, any pain in the knee and back joints increases the risk of falling in older men [24]. In the study by Kitayuchi et al., it was found that LBP and KP are associated with the occurrence of falls [25]. The results of these two studies are not consistent with our results, perhaps because they used a questionnaire to evaluate falls. A study for examining the association of KP and LBP with balance test scores has not been conducted so far. In Bennell and Hinman's study on balance disorders in people with knee osteoarthritis compared to the control group, using clinical tests, it was found that the dynamic balance was weaker in the group with knee osteoarthritis [26]. Knee osteoarthritis is one of the causes of KP in the elderly; hence, their results are in line with our results. In the study by Yanardag et al., by investigating the relationship between pain, balance, walking performance and quality of life in elderly people with LBP and KP, the authors found a significant relationship between LBP and KP with the TUG test [27].
In the present study, with increasing age, the TUG test score of older adults increased, i.e. their dynamic balance decreased. Takacs et al. in a study on factors related to dynamic balance in older people with knee osteoarthritis, found that dynamic balance significantly decreased with aging [28]. This is consistent with our results. Kiss et al. examined perturbation-based balance in older adults with varying degrees of knee osteoarthritis. They found no significant relationship between age and static balance in the group with severe knee osteoarthritis. They used the static balance test which can be the reason for the lack of consistency with the present study.
In the present study, with increasing fear of falling, the TUG test score of older adults increased, i.e. their dynamic balance decreased. Ulus et al. and Halaweh et al. also found a positive and significant correlation between the scores of FES-I and TUG test [29, 30]. This is consistent with our results. No significant relationship was found between body mass index and TUG test score. Mohd Said et al, by examining balance in older people and its relationship with physiological factors of the body in different ankle joint conditions, did not find a significant relationship between balance and body mass index [31]. In Gouveia et al.'s study on the demographic characteristics, balance, and mobility of the elderly in Portugal, it was found that balance decreased significantly with an increase in body mass index [32]. The reason for the discrepancy may be the difference in the study area and the lower average age of the participants. In the study by Sarshin et al., a significant relationship was found between body mass index and static and dynamic balances [33]. This discrepancy can be due to in the selection of young subjects and athletes in their study.
In the present study, no significant relationship was found between gender and TUG test score. In the study by Espinoza et al. on postural balance and temporal and spatial factors of gait in older men and women, it was found that the postural balance of older men was poorer than that of older women [35]. This discrepancy can be due to the difference in the measurement tools and the study factors, and balance was not measured with balance tests.
There is a significant difference among the healthy elderly and those with chronic LBP and chronic KP in dynamic balance. The older adults with chronic KP have a poorer dynamic balance. To prevent balance deficits in old age, prevention and treatment of knee injuries should be prioritized by doctors and therapists. Other factors related to balance deficiency in older adults should also be identified.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1400.065). All participants were informed about the study process. They were assured of the confidentiality of their information and were free to leave the study at any time. A written informed consent was obtained from them.
Funding
This article was extracted from the master’s degree of Elham Azarm registered by the Faculty of Rehabilitation, Department of Physiotherapy, University of Social Welfare and Rehabilitation Sciences. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors
Authors' contributions
The authors contributed equally to preparing this paper.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the General Welfare Organization of Khorasan Razavi province, all nursing homes in Mashhad city, and all seniors participated in this study for their cooperation.
References
- Olshansky SJ, Carnes BA, Cassel CK. The aging of the human species. Scientific American. 1993; 268(4):46-52. [DOI:10.1038/scientificamerican0493-46] [PMID]
- Mosallanezhad Z, Salavati M, Hellstrom K, Reza Sotoudeh G, Nilsson Wikmar L, Frandin K. Cross-cultural adaptation, reliability and validity of the Persian version of the Modified Falls Efficacy Scale. Disability and Rehabilitation. 2011; 33(25-26):2446-53. [DOI:10.3109/09638288.2011.574774] [PMID]
- Muir SW, Berg K, Chesworth B, Klar N, Speechley M. Quantifying the magnitude of risk for balance impairment on falls in community-dwelling older adults: A systematic review and meta-analysis. Journal of Clinical Epidemiology. 2010; 63(4):389-406. [DOI:10.1016/j.jclinepi.2009.06.010] [PMID]
- Shumway-Cook A, Baldwin M, Polissar NL, Gruber W. Predicting the probability for falls in community-dwelling older adults. Physical Therapy. 1997; 77(8):812-9. [DOI:10.1093/ptj/77.8.812] [PMID]
- Shumway-Cook A, Patla AE, Stewart A, Ferrucci L, Ciol MA, Guralnik JM. Environmental demands associated with community mobility in older adults with and without mobility disabilities. Physical Therapy. 2002; 82(7):670-81. [DOI:10.1093/ptj/82.7.670] [PMID]
- Legters K. Fear of falling. Physical Therapy. 2002; 82(3):264-72. [DOI:10.1093/ptj/82.3.264] [PMID]
- Nodehi Moghadam A, Ehsani Fard F. [Prevalence of physical impairment among the elderlly persons of the Tehran City in 1385 (Persian)]. Salmand: Iranian Journal of Ageing. 2007; 1(2):125-31. [Link]
- Kim IJ, Kim HA, Seo YI, Jung YO, Song YW, Jeong JY, et al. Prevalence of knee pain and its influence on quality of life and physical function in the Korean elderly population: A community based cross-sectional study. Journal of Korean Medical Science. 2011; 26(9):1140-6. [DOI:10.3346/jkms.2011.26.9.1140] [PMID] [PMCID]
- Bennell KL, Hinman RS. Effect of experimentally induced knee pain on standing balance in healthy older individuals. Rheumatology (Oxford, England). 2005; 44(3):378-81. [DOI:10.1093/rheumatology/keh493] [PMID]
- Nachemson A, Waddell G, Norlund A. Epidemiology of neck and low back pain. In: Nachemson A, Jonsson E, editors. Neck and back pain: The scientific evidence of causes, diagnos is and treatment. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins; 2000.
- Ebenbichler GR, Oddsson LI, Kollmitzer J, Erim Z. Sensory-motor control of the lower back: Implications for rehabilitation. Medicine and Science in Sports and Exercise. 2001; 33(11):1889-98. [DOI:10.1097/00005768-200111000-00014] [PMID]
- Wright VJ, Perricelli BC. Age-related rates of decline in performance among elite senior athletes. The American Journal of Sports Medicine. 2008; 36(3):443-50. [DOI:10.1177/0363546507309673] [PMID]
- Lin HW, Bhattacharyya N. Balance disorders in the elderly: Epidemiology and functional impact. The Laryngoscope. 2012; 122(8):1858-61. [DOI:10.1002/lary.23376] [PMID]
- Tsigkanos C, Gaskell L, Smirniotou A, Tsigkanos G. Static and dynamic balance deficiencies in chronic low back pain. Journal of Back and Musculoskeletal Rehabilitation. 2016; 29(4):887-93. [DOI:10.3233/BMR-160721] [PMID]
- Tsonga T, Michalopoulou M, Malliou P, Godolias G, Kapetanakis S, Gkasdaris G, et al. Analyzing the history of falls in patients with severe knee osteoarthritis. Clinics in Orthopedic Surgery. 2015; 7(4):449-56. [DOI:10.4055/cios.2015.7.4.449] [PMID] [PMCID]
- da Silva RA, Vieira ER, Fernandes KBP, Andraus RA, Oliveira MR, Sturion LA, et al. People with chronic low back pain have poorer balance than controls in challenging tasks. Disability and Rehabilitation. 2018; 40(11):1294-300. [DOI:10.1080/09638288.2017.1294627] [PMID]
- Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age and Ageing. 2005; 34(6):614-9. [DOI:10.1093/ageing/afi196] [PMID]
- Khajavi D. [Validation and Reliability of Persian Version of Fall Efficacy Scale-International (FES-I) in community-dwelling older adults (Persian)]. Salmand: Iranian Journal of Ageing. 2013; 8(2):39-47. [Link]
- Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Research in Nursing & Health. 1990; 13(4):227-36. [DOI:10.1002/nur.4770130405] [PMID]
- Babaei Khorzoghi M, Sajjadian PS. [The effectiveness of bedtime exercises on sleep quality parameters and chronic nonspecific chronic low back pain after sleep in the elderly male (Persian)]. Salmand: Iranian Journal of Ageing. 2022; 17(1):44-61. [DOI:10.32598/sija.2021.2111.3]
- Moshref-Razavi S, Sohrabi M, Sotoodeh MS. [Effect of neurofeedback interactions and mental imagery on the elderly’s balance (Persian)]. Salmand: Iranian Journal of Ageing. 2017; 12(3):288-99. [DOI:10.21859/sija.12.3.288]
- Mirzaee GH, Noori-zadeh S. Comparison of functional balance in elderlies with and withouth total hip arthroplasty. Iranian Journal of Ageing. 2009; 8(13):21-6.
- Ghavi S, Golmohamadi B, Sohrabi M, Karimi N, Rahimi M, Sahaf R. [The effect of whole body vibration exercise, mental practice on balance of elderly men (Persian)]. Salmand: Iranian Journal of Ageing. 2015; 9(4):306-15. [Link]
- Munch T, Harrison SL, Barrett-Connor E, Lane NE, Nevitt MC, Schousboe JT, et al. Pain and falls and fractures in community-dwelling older men. Age and Ageing. 2015; 44(6):973-9. [DOI:10.1093/ageing/afv125] [PMID] [PMCID]
- Kitayuguchi J, Kamada M, Inoue S, Kamioka H, Abe T, Okada S, et al. Association of low back and knee pain with falls in Japanese community-dwelling older adults: A 3-year prospective cohort study. Geriatrics & Gerontology International. 2017; 17(6):875-84. [DOI:10.1111/ggi.12799] [PMID]
- Hinman RS, Bennell KL, Metcalf BR, Crossley KM. Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology. 2002; 41(12):1388-94. [DOI:10.1093/rheumatology/41.12.1388] [PMID]
- Yanardag M, Şimşek TT, Yanardag F. Exploring the relationship of pain, balance, gait function, and quality of life in older adults with hip and knee pain. Pain Management Nursing. 2021; 22(4):503-8. [DOI:10.1016/j.pmn.2020.12.011] [PMID]
- Takacs J, Carpenter MG, Garland SJ, Hunt MA. Factors associated with dynamic balance in people with knee osteoarthritis. Archives of Physical Medicine and Rehabilitation. 2015; 96(10):1873-9. [DOI:10.1016/j.apmr.2015.06.014] [PMID]
- Ulus Y, Durmus D, Akyol Y, Terzi Y, Bilgici A, Kuru O. Reliability and validity of the Turkish version of the Falls Efficacy Scale International (FES-I) in community-dwelling older persons. Archives of Gerontology and Geriatrics. 2012; 54(3):429-33. [DOI:10.1016/j.archger.2011.06.010] [PMID]
- Halaweh H, Svantesson U, Rosberg S, Willen C. Cross-cultural adaptation, validity and reliability of the Arabic version of the Falls Efficacy Scale-International (FES-I). Medical Principles and Practice : International Journal of the Kuwait University, Health Science Centre. 2016; 25(1):1-7. [DOI:10.1159/000441128] [PMID] [PMCID]
- Mohd Said A, Manaf H, Bukry SA, Justine M. Mobility and balance and their correlation with physiological factors in elderly with different foot postures. BioMed Research International. 2015; 2015:385269. [DOI:10.1155/2015/385269] [PMID] [PMCID]
- Gouveia ÉR, Gouveia BR, Ihle A, Kliegel M, Marques A, Freitas DL. Balance and mobility relationships in older adults: A representative population-based cross-sectional study in Madeira, Portugal. Archives of Gerontology and Geriatrics. 2019; 80:65-9. [DOI:10.1016/j.archger.2018.10.009] [PMID]
- Sarshin A, Alijani E, Faiz Elahi F, Shojauddin S, Pashaei S, Abdi J. [Correlation of body composition indices with static and dynamic balance (Persian)]. Sports Science Quarterly. 2012; 4(9):69-93. [Link]
- Nakagawa HB, Ferraresi JR, Prata MG, Scheicher ME. Postural balance and functional independence of elderly people according to gender and age: Cross-sectional study. Sao Paulo Medical Journal = Revista paulista de medicina. 2017; 135(3):260-5. [DOI:10.1590/1516-3180.2016.0325280217] [PMID] [PMCID]
- Espinoza-Araneda J, Bravo-Carrasco V, Álvarez C, Marzuca-Nassr GN, Muñoz-Mendoza CL, Muñoz J, et al. Postural balance and gait parameters of independent older adults: A sex difference analysis. International Journal of Environmental Research and Public Health. 2022; 19(7):4064. [DOI:10.3390/ijerph19074064] [PMID] [PMCID]
Type of Study: Research |
Subject:
gerontology
Received: 2022/08/26 | Accepted: 2023/01/23 | Published: 2023/10/11
Received: 2022/08/26 | Accepted: 2023/01/23 | Published: 2023/10/11
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |