Volume 18, Issue 1 (Spring 2023)
Salmand: Iranian Journal of Ageing 2023, 18(1): 104-117 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Melali F, Hoseini H, Moeini M. Medication Adherence Among Elderly With Hypertension: Johnson Model-based Program. Salmand: Iranian Journal of Ageing 2023; 18 (1) :104-117
URL: http://salmandj.uswr.ac.ir/article-1-2391-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2391-en.html
1- Department of, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Nursing and Midwifery Care Research Center, Department of Health, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran. ,h_hoseini@nm.mui.ac.ir
3- Nursing and Midwifery Care Research Center, Department of Health, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Nursing and Midwifery Care Research Center, Department of Health, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran. ,
3- Nursing and Midwifery Care Research Center, Department of Health, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran.
Full-Text [PDF 4746 kb]
(1485 Downloads)
| Abstract (HTML) (2498 Views)
Full-Text: (1505 Views)
Introduction
High blood pressure is the most common cause of cerebral stroke and kidney failure in the elderly, which does not require advanced equipment to control it; it can be easily controlled by taking medicine. However, the critical point in this context is the medication non-adherence and its incorrect use or non-use, which can lead to unfortunate consequences, such as more hospitalizations, increased healthcare costs, low quality of life, reduced physical performance, and advanced cognitive disorders. The use of models is a suggestion to help improve medication adherence. Since the lack of care and failure of the elderly are the crucial reasons for the medication non-adherence, these models should be accompanied by targeted action, patterned behavior, and feedback. Therefore this study aims to determine the effect of the Johnson model-based program on medication adherence of the elderly with high blood pressure.
Methods
The present study was a randomized controlled clinical trial with a two-group and three-stage design. The statistical population included all elderly people with high blood pressure who were referred to three bases of the Shahid Aval comprehensive health service center of Isfahan City, Iran in 2019. A total of 70 people were selected based on the inclusion criteria, including diagnosis of high blood pressure by a specialist doctor of the confirmed center and undergoing treatment, not suffering from known mental illnesses, not smoking and other tobacco products, non-participation of the elderly in family-oriented programs in the last three months, access to fix phone or cell phone at home, familiarity with Farsi language and they were allocated in two intervention and control groups. Data collection tools were a Riester Nova 1032 mercury sphygmomanometer made in Germany, a stethoscope, an elderly blood pressure registration checklist, a needs assessment questionnaire, and demographic characteristics questionnaire of the research units. For the intervention test group, a program based on Johnson’s model was implemented once a week. For this purpose, the model of medication adherence consisting of three concepts of targeted action, patterned behavior, and feedback was used. The intervention in this study was conducted by focusing on the concepts of the adherence model as a combination of group meetings, group discussions, face-to-face interviews, lectures, giving educational booklets, and home visits. In addition to the elderly, an active family member (informal caregiver) also participated in the meetings. The first 3 sessions focused on the concept of purposeful action (perceived need, perceived effectiveness, perceived safety), and the fourth session focused on the concept of patterned behavior (access, routine, reminder). The meetings were held in groups of 5 to 6 people and in the meeting hall of the center every week for a period of 30 to 60 minutes. The third concept (feedback) was carried out during 2 home visit sessions. Data were analyzed with SPSS22 statistical software using independent t test, chi-square, and repeated analysis of variance (ANOVA).
Results
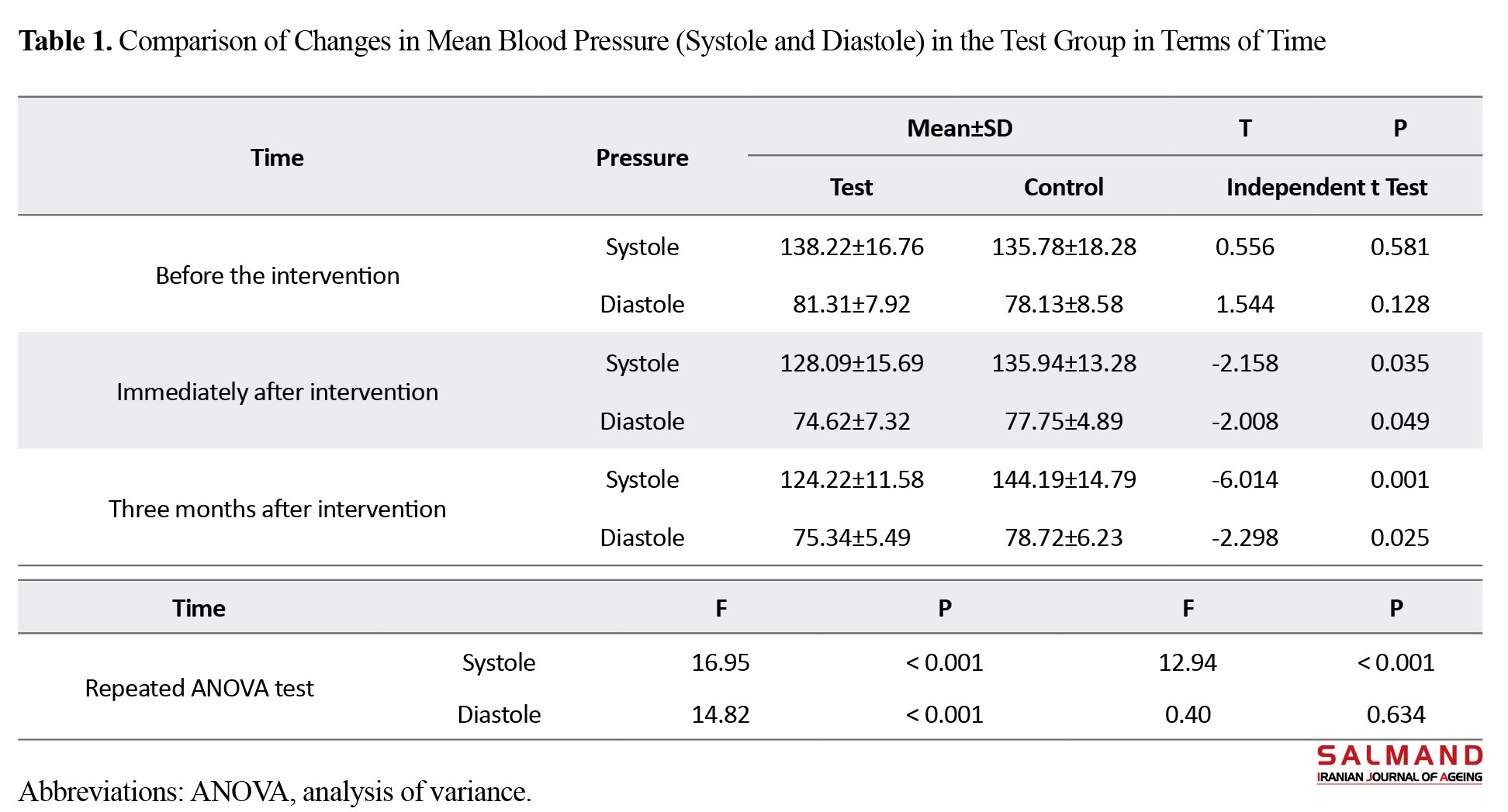
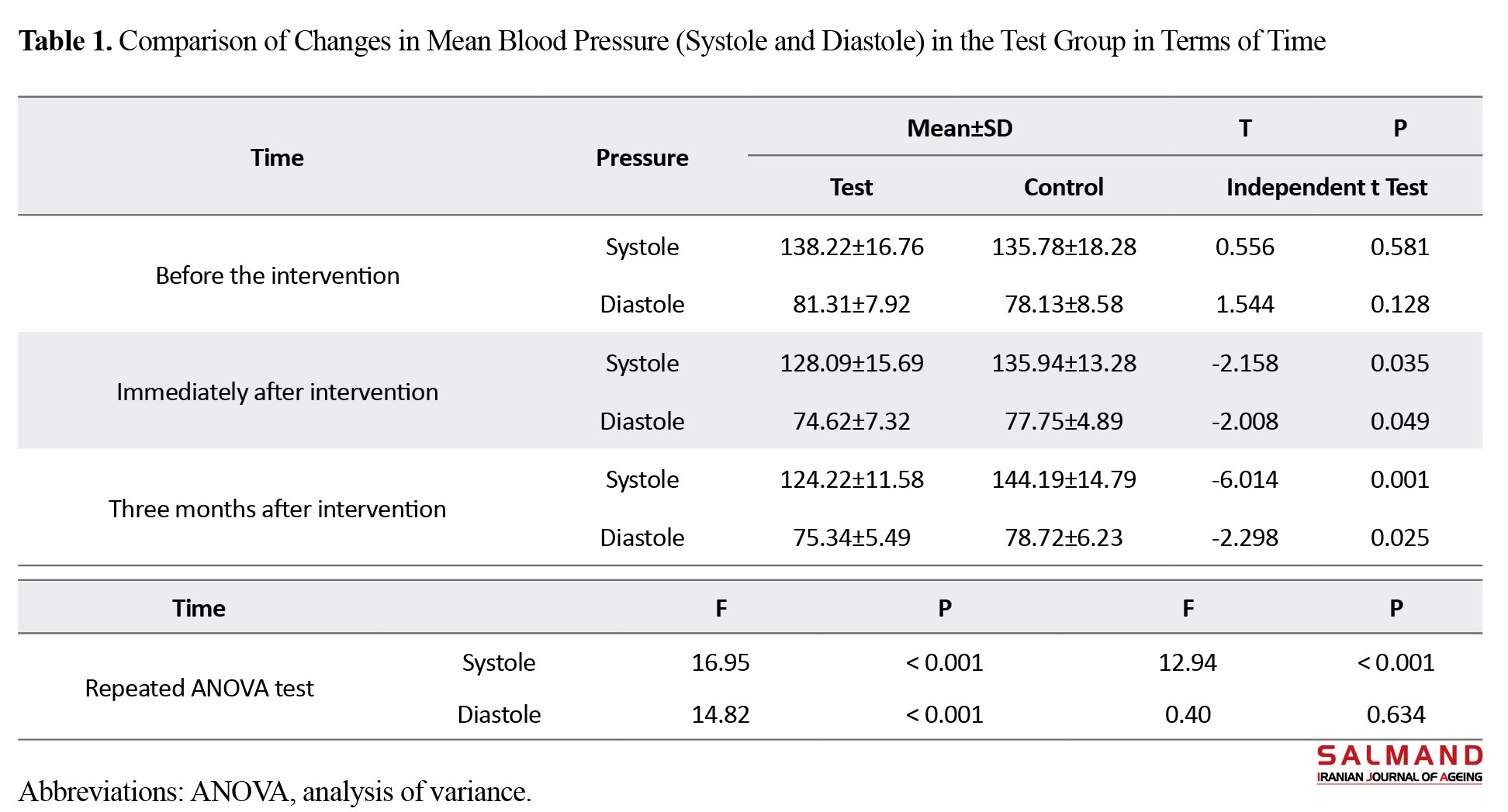
The results of the study showed that the two groups had no significant statistical differences in terms of demographic characteristics. According to the purpose of the study, the mean systolic and diastolic blood pressure of the two groups at the beginning of the study did not have a statistically significant difference (P<0.05). Immediately after the implementation of the intervention and also after 3 months of follow-up in the intervention group, it decreased significantly (P<0.05). Also, the repeated measurement analysis of variance (ANOVA) showed that in the test group, systolic and diastolic blood pressure had a decreasing trend in three times (P<0.001) but in the control group, the trend of changes in the mean systolic blood pressure increased significantly, and regarding diastolic blood pressure, despite the significant decrease in the post-test time, but three months, no significant difference was observed (P=0.63) (Table 1).
Discussion
Family-based medication adherence program based on Johnson’s model is effective in reducing blood pressure in the elderly with hypertension, and this means that this medication plan as a nursing intervention and an easy, low-cost, and accessible method can be vital in the medication program of these elderly people. Many elderly people and their families still have little information on the disease and its complications, despite passing a lot of time from the disease, and they do not follow the prescribed medication. In line with the comprehensive nurse and considering the importance of the role of the family in the treatment of the patient, it is necessary to pay attention to the education of the family in nursing care; hence training by the personnel of the pharmaceutical health service system, especially nurses, will be very helpful.
Ethical Considerations
Compliance with ethical guidelines
Ethical principles are fully observed in this article. Participants were allowed to withdraw from the study whenever they wanted. Also, all participants were aware of the research process. Their information was kept confidential. Also, all ethical principles have been approved by the Ethical Committee of Isfahan University of Medical Sciences (Code: IR.MUI.RESEARCH.REC.1398.410).
Funding
This study is part of a thesis approved at Isfahan University of Medical Sciences, which was conducted at Shahid Aval comprehensive health services center of Isfahan.
Authors' contributions
All authors contributed equally to the preparation of this article.
Conflicts of interest
The authors declared no conflict of interest in this article.
Acknowledgements
We appreciate the graduate studies of the university and the sincere cooperation of the honorable director and management of the center, seniors, and valuable companions that without their cooperation, this research was impossible.
References
High blood pressure is the most common cause of cerebral stroke and kidney failure in the elderly, which does not require advanced equipment to control it; it can be easily controlled by taking medicine. However, the critical point in this context is the medication non-adherence and its incorrect use or non-use, which can lead to unfortunate consequences, such as more hospitalizations, increased healthcare costs, low quality of life, reduced physical performance, and advanced cognitive disorders. The use of models is a suggestion to help improve medication adherence. Since the lack of care and failure of the elderly are the crucial reasons for the medication non-adherence, these models should be accompanied by targeted action, patterned behavior, and feedback. Therefore this study aims to determine the effect of the Johnson model-based program on medication adherence of the elderly with high blood pressure.
Methods
The present study was a randomized controlled clinical trial with a two-group and three-stage design. The statistical population included all elderly people with high blood pressure who were referred to three bases of the Shahid Aval comprehensive health service center of Isfahan City, Iran in 2019. A total of 70 people were selected based on the inclusion criteria, including diagnosis of high blood pressure by a specialist doctor of the confirmed center and undergoing treatment, not suffering from known mental illnesses, not smoking and other tobacco products, non-participation of the elderly in family-oriented programs in the last three months, access to fix phone or cell phone at home, familiarity with Farsi language and they were allocated in two intervention and control groups. Data collection tools were a Riester Nova 1032 mercury sphygmomanometer made in Germany, a stethoscope, an elderly blood pressure registration checklist, a needs assessment questionnaire, and demographic characteristics questionnaire of the research units. For the intervention test group, a program based on Johnson’s model was implemented once a week. For this purpose, the model of medication adherence consisting of three concepts of targeted action, patterned behavior, and feedback was used. The intervention in this study was conducted by focusing on the concepts of the adherence model as a combination of group meetings, group discussions, face-to-face interviews, lectures, giving educational booklets, and home visits. In addition to the elderly, an active family member (informal caregiver) also participated in the meetings. The first 3 sessions focused on the concept of purposeful action (perceived need, perceived effectiveness, perceived safety), and the fourth session focused on the concept of patterned behavior (access, routine, reminder). The meetings were held in groups of 5 to 6 people and in the meeting hall of the center every week for a period of 30 to 60 minutes. The third concept (feedback) was carried out during 2 home visit sessions. Data were analyzed with SPSS22 statistical software using independent t test, chi-square, and repeated analysis of variance (ANOVA).
Results
The results of the study showed that the two groups had no significant statistical differences in terms of demographic characteristics. According to the purpose of the study, the mean systolic and diastolic blood pressure of the two groups at the beginning of the study did not have a statistically significant difference (P<0.05). Immediately after the implementation of the intervention and also after 3 months of follow-up in the intervention group, it decreased significantly (P<0.05). Also, the repeated measurement analysis of variance (ANOVA) showed that in the test group, systolic and diastolic blood pressure had a decreasing trend in three times (P<0.001) but in the control group, the trend of changes in the mean systolic blood pressure increased significantly, and regarding diastolic blood pressure, despite the significant decrease in the post-test time, but three months, no significant difference was observed (P=0.63) (Table 1).
Discussion
Family-based medication adherence program based on Johnson’s model is effective in reducing blood pressure in the elderly with hypertension, and this means that this medication plan as a nursing intervention and an easy, low-cost, and accessible method can be vital in the medication program of these elderly people. Many elderly people and their families still have little information on the disease and its complications, despite passing a lot of time from the disease, and they do not follow the prescribed medication. In line with the comprehensive nurse and considering the importance of the role of the family in the treatment of the patient, it is necessary to pay attention to the education of the family in nursing care; hence training by the personnel of the pharmaceutical health service system, especially nurses, will be very helpful.
Ethical Considerations
Compliance with ethical guidelines
Ethical principles are fully observed in this article. Participants were allowed to withdraw from the study whenever they wanted. Also, all participants were aware of the research process. Their information was kept confidential. Also, all ethical principles have been approved by the Ethical Committee of Isfahan University of Medical Sciences (Code: IR.MUI.RESEARCH.REC.1398.410).
Funding
This study is part of a thesis approved at Isfahan University of Medical Sciences, which was conducted at Shahid Aval comprehensive health services center of Isfahan.
Authors' contributions
All authors contributed equally to the preparation of this article.
Conflicts of interest
The authors declared no conflict of interest in this article.
Acknowledgements
We appreciate the graduate studies of the university and the sincere cooperation of the honorable director and management of the center, seniors, and valuable companions that without their cooperation, this research was impossible.
References
- Kooshyar H, Shoorvazi M, Dalir Z, Hosseini M. [Health literacy and its relationship with medical adherence and health-related quality of life in diabetic community-residing elderly (Persian)]. Journal of Mazandaran University of Medical Sciences. 2014; 23(1):134-43. [Link]
- Tripathi N, Kishore J, Babu BV. Prevalence of hypertension in indian tribal adult population: A scoping review. Journal of Advanced Research in Medicine. 2020; 7(1):5-13. [DOI:10.24321/2349.7181.202002]
- Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. The Lancet. 2021; 398(10304):957-80. [DOI:10.1016/S0140-6736(21)01330-1] [PMID]
- Luo X, Yang H, He Z, Wang S, Chen T, Li C. Numbers and mortality risk of hypertensive patients with or without elevated body mass index in China. International Journal of Environmental Research and Public Health. 2022; 19(1):116. [DOI:10.3390/ijerph19010116] [PMID] [PMCID]
- Oori MJ, Mohammadi F, Norozi K, Fallahi-Khoshknab M, Ebadi A, Gheshlagh RG. Prevalence of HTN in Iran: Meta-analysis of published studies in 2004-2018. Current Hypertension Reviews. 2019; 15(2):113-22. [DOI:10.2174/1573402115666190118142818] [PMID] [PMCID]
- Cheraghi P, Mihandoost Yeganeh Z, Dosti Irani A, Sangestani M, Cheraghi Z, Khezeli M. Study on the prevalence of hypertension and its associated factors in the elderly population. Journal of Geriatric Nursing. 2015; 1(3):73-86. [Link]
- Bae SG, Jeon HJ, Yang HS, Kim BK, Park KS. Medication adherence and its predictors in community elderly patients with hypertension. Korean Journal of Health Promotion. 2015; 15(3):121-8. [DOI:10.15384/kjhp.2015.15.3.121]
- Fakhri A, Morshedi H, Mohammadi Zeidi I. Effectiveness of theory based education on medication adherence in older adults with hypertension. Jundishapur Scientific Medical Journal. 2017; 16(2):161-74. [Link]
- Haghighi M, Ilali E, Yazdani J, Taraghi Z. [Relationship between cognitive status and medication adherence among elderly patients with hypertension (Persian)]. Journal of Health Research in Community. 2020; 5(4):33-44. [Link]
- Hawkins LA, Kilian S, Firek A, Kashner TM, Firek CJ, Silvet H. Cognitive impairment and medication adherence in outpatients with heart failure. Heart & Lung. 2012; 41(6):572-82. [DOI:10.1016/j.hrtlng.2012.06.001] [PMID]
- Tabari F, Zakerimoghadam M, Hejazi ZS. The effect of the family-centered educational program on medication management in elderly patients with ischemic heart disease. Iranian Journal of Nursing Research. 2019; 14(1):14-20. [DOI:10.1016/j.hrtlng.2012.06.001] [PMID]
- Mikaili N, Ghasemi MA, Salari S, Sakeni Z. [Theoretical and practical dimensions of adherence to treatment in patients: A review study (Persian)]. Medical Journal of Mashhad University of Medical Sciences. 2019; 62(2):1403-19. [Link]
- Foley L, Larkin J, Lombard-Vance R, Murphy AW, Hynes L, Galvin E, et al. Prevalence and predictors of medication non-adherence among people living with multimorbidity: A systematic Review and Meta-Analysis. BMJ Open. 2021; 11(9):e044987. [DOI:10.1136/bmjopen-2020-044987] [PMID] [PMCID]
- Bastani P, Bikineh P, Mehralian G, Sadeghkhani O, Rezaee R, Kavosi Z, et al. Medication adherence among the elderly: Applying grounded theory approach in a developing country. Journal of Pharmaceutical Policy and Practice. 2021; 14(1):1-8. [DOI:10.1186/s40545-021-00340-9] [PMID] [PMCID]
- Hemmati Maslakpak M, Safaie M. Effect of reminder cards on adherence to treatment in patients with uncontrolled hypertension. Iranian Journal of Nursing Research. 2016; 11(5):26-31. [DOI:10.21859/ijnr-11055]
- Kaur RJ. Elderly and medication non-adherence. Journal of The Indian Academy of Geriatrics. 2019; 15(1):1-12. [Link]
- Johnson MO, Chesney MA, Goldstein RB, Remien RH, Catz S, Gore-Felton C, et al. Positive provider interactions, adherence self-efficacy, and adherence to antiretroviral medications among HIV-infected adults: A mediation model. AIDS Patient Care & STDs. 2006; 20(4):258-68. [DOI:10.1089/apc.2006.20.258] [PMID] [PMCID]
- Johnson MJ. The medication adherence model: A guide for assessing medication taking. Research and Theory for Nursing Practice. 2002; 16(3):179-92. [DOI:10.1891/rtnp.16.3.179.53008] [PMID]
- Stawarz K, Rodríguez MD, Cox AL, Blandford A. Understanding the use of contextual cues: Design implications for medication adherence technologies that support remembering. Digital Health. 2016; 2:2055207616678707. [DOI:10.1177/2055207616678707] [PMID] [PMCID]
- Kaakinen JR. Family health care nursing: Theory, practice, and research. Philadelphia: F.A. Davis Company; 2018. [Link]
- Heydari M, Sh E, Masoudi RE, Kheiri SO, Jivad NA. The effect of family-centered care on the family caregivers’ burden of patients with epilepsy. Journal of Clinical Nursing and Midwifery. 2018; 7(2):146-57. [Link]
- Saeid Y, Salaree MM, Ebadi A, Moradian ST. Family Intensive Care Unit Syndrome (FICUS): Letters to the editor. Journal of Critical Care Nursing. 2019; 12(2):1-3. [Link]
- Parvareshan S, Shamsalinia AB, Jahanshahi ME, Hajiahmadi MA. Impact of family-based empowering model on the per-ceived threat and self-efficacy of families of diabetic elderly at risk of falling. Journal of Clinical Nursing and Midwifery. 2018; 7(2):96-107. [Link]
- Hedayati B. Effect of family-based empowerment model on the self-efficacy of hypertensive elderly people. Iranian Journal of Ageing. 2018; 13(1):86-97. [DOI:10.21859/sija.13.1.86]
- Rezaie B, Khademvatan K, Alinejad V. [The impact of family-oriente lifestyle -based group discussion ion the controling hypertension (Persian)]. Nursing and Midwifery Journal. 2016; 14(6):535-42. [Link]
- Yazdanpanah Y, Saleh Moghadam AR, Mazlom SR, Haji Ali Beigloo R, Mohajer S. [Effect of an educational program based on health belief model on medication adherence in elderly patients with hypertension (Persian)]. Evidence Based Care. 2019; 9(1):52-62. [Link]
- Son KJ, Son HR, Park B, Kim HJ, Kim CB. A community-based intervention for improving medication adherence for elderly patients with hypertension in Korea. International Journal of Environmental Research and Public Health. 2019; 16(5):721. [DOI:10.3390/ijerph16050721] [PMID] [PMCID]
- Myoungsuk KI. Effects of customized long-message service and phone-based health-coaching on elderly people with hypertension. Iranian Journal of Public Health. 2019; 48(4):655. [PMCID] [PMID]
- Woodham N, Taneepanichskul S, Somrongthong R, Auamkul N. Medication adherence and associated factors among elderly hypertension patients with uncontrolled blood pressure in rural area, Northeast Thailand. Journal of Health Research. 2018; 32(6):449-58 . [DOI:10.1108/JHR-11-2018-085]
- Kurniawati ND, Wahyuni ED, Toulasik YA. Family support improves hypertensive patient drug compliance. Indian Journal of Public Health Research & Development. 2019; 10(8):2660-5. DOI:10.5958/0976-5506.2019.02270.8]
- Olowookere AJ, Olowookere SA, Talabi AO, Etonyeaku AC, Adeleke OE, Akinboboye OO. Perceived family support and factors influencing medication adherence among hypertensive patients attending a Nigerian tertiary hospital. Annals of Tropical Medicine & Public Health. 2015; 8(6):241-5. [DOI:10.4103/1755-6783.162668]
Type of Study: Research |
Subject:
Geriatric
Received: 2022/01/06 | Accepted: 2022/06/14 | Published: 2023/03/30
Received: 2022/01/06 | Accepted: 2022/06/14 | Published: 2023/03/30
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |