Volume 18, Issue 3 (Autumn 2023)
Salmand: Iranian Journal of Ageing 2023, 18(3): 304-325 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghaderian M, Ghasemi G A, Lenjannejadian S, Sadeghi Demneh E. Effect of Combined Exercises on Stair Negotiation Performance of Older Men: A Randomized Controlled Clinical Trial. Salmand: Iranian Journal of Ageing 2023; 18 (3) :304-325
URL: http://salmandj.uswr.ac.ir/article-1-2464-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2464-en.html
1- Department of Sport Injuries and Corrective Exercises, Faculty of Sport Sciences, University of Isfahan, Isfahan, Iran. , mehdighaderiyan67@gmail.com
2- Department of Sport Injuries and Corrective Exercises, Faculty of Sport Sciences, University of Isfahan, Isfahan, Iran.
3- Department of Orthotics and Prosthetics, Faculty of Rehabilitation Sciences, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Sport Injuries and Corrective Exercises, Faculty of Sport Sciences, University of Isfahan, Isfahan, Iran.
3- Department of Orthotics and Prosthetics, Faculty of Rehabilitation Sciences, Isfahan University of Medical Sciences, Isfahan, Iran.
Full-Text [PDF 9066 kb]
(2223 Downloads)
| Abstract (HTML) (4824 Views)
Full-Text: (2848 Views)
Introduction
Aging is a global concern that is associated with a decline in organ function and makes a person vulnerable to diseases. Falling is one of the causes of injuries in older adults [1]. Stair climbing is a problematic activity and one of the most common causes of falls in older adults [2, 3]. The elderly are three times more likely to fall when walking up the stairs than when walking on the ground [4]. Balance disorders make stair climbing difficult for the elderly [5]. Controlling balance while climbing stairs is more difficult than that when walking [6]. Most of studies have focused on improving the balance of the elderly while walking, and less attention has been paid to their stair-climbing performance. The mechanisms of balance improvement are different. Combined and multi-component training programs may cause better results in balance improvement [7]. The present study aims to investigate the effect of combined exercises on the stair negotiation performance of older men.
Methods
This is a randomized controlled clinical trial with a pre-test/post-test design. Thirty older men were selected and randomly allocated to two parallel groups of intervention and control. The intervention group performed 12 weeks of combined exercises, while the control group continued their usual activities during this period. Inclusion criteria were age at least 60 years, functional independence, obtaining the required scores in the general health questionnaire-28, mini-mental state examination, and physical activity readiness questionnaire; no any medical and ethical restrictions, ability to complete tests and exercises, and no participation in other regular exercise programs. Exclusion criteria included an unwillingness to participate in tests and absence from exercise sessions. The participants performed the stair negotiation tests and their kinetic and kinematic data were recorded using the Kistler force plate and the Qualisys motion capture system. The balance was measured with the center of pressure (COP) parameters [1]. The stair ascending and descending time was calculated with kinematic data. Stair negotiation performance was evaluated with the timed up and down stairs (TUDS) test [8], and the self-efficacy was evaluated with the stair self-efficacy (SSE) scale [9]. The exercise protocol consisted of warm-up (10 minutes), resistance training (20 minutes), balance, hopping, and jump training (40 minutes), and cooling down (5 minutes) for 12 weeks. The overload principle was observed with a gradual increase in the duration, number, and load amount. Statistical analysis was carried out using mixed ANOVA. Pairwise comparison was done with the Bonferroni test, and the effect size (partial eta squared) was calculated [10]. The significance level was set at 0.05.
Results
Descriptive information and the results of mixed ANOVA for the stair negotiation variable are reported in Table 1.
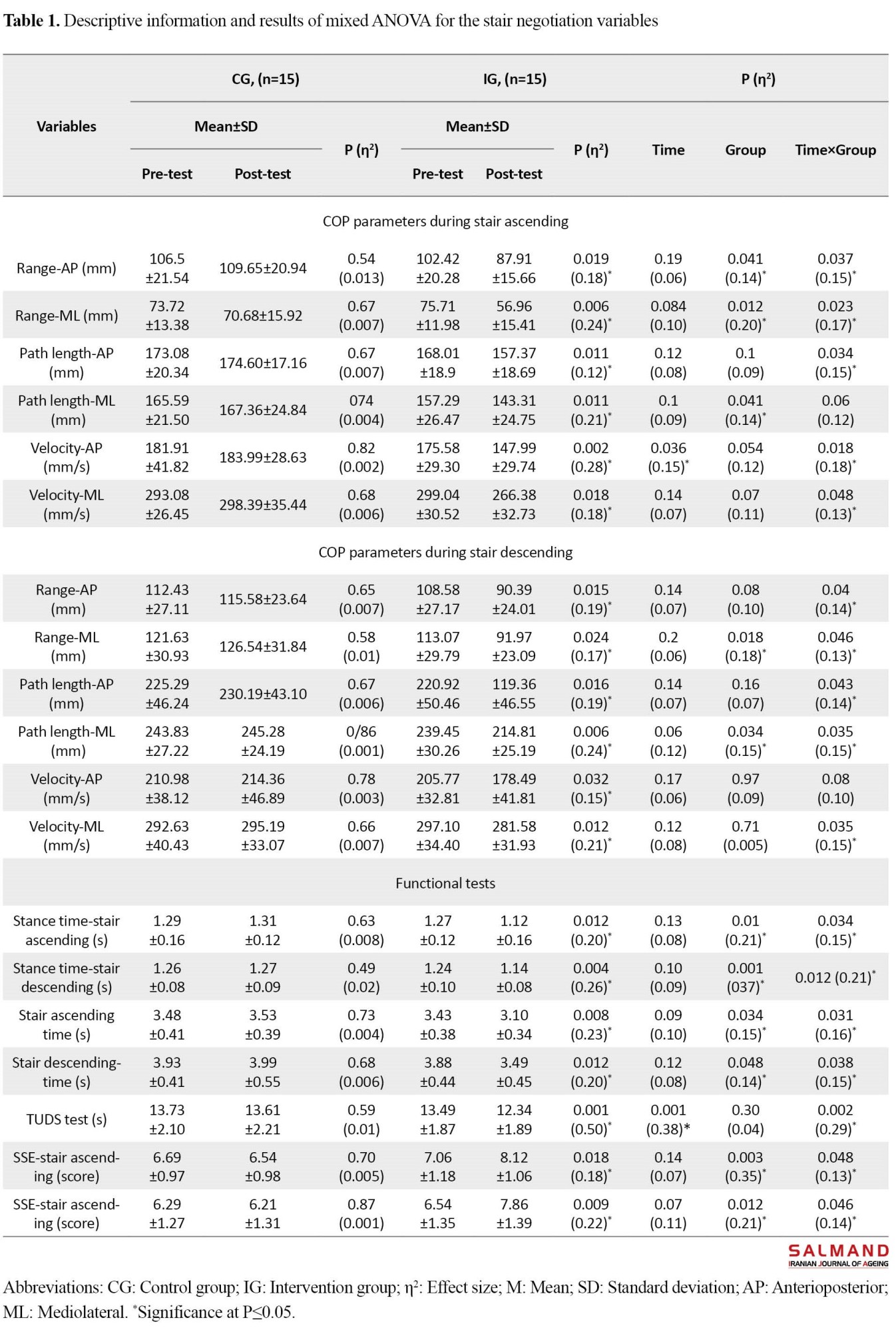
Interaction effects of the COP parameters, including range and velocity in anteroposterior and mediolateral directions, and path length in the anteroposterior direction were significant during stair ascending (P≤0.047, η2=0.12-0.18) as well as the range and path length in the anteroposterior and mediolateral directions and the velocity in the mediolateral direction during stair descending (P=0.046, η2=0.10-0.15), and in all functional tests variables (P=0.048, η2=0.13-0.29). The results of Bonferroni test showed a significant improvement in the variables in the post-test phase compared to the pre-test phase in the intervention group (P=0.032). No significant change was observed in any of the variables in the control group (P>0.05). The results showed a decrease in the COP parameters and an improvement in balance control during stair ascending and descending in the intervention group. Also, duration of stance phase, total time in stair ascending and descending, and the TUDS test time decreased and the stair self-efficacy was improved after exercises.
Conclusion
The results showed that the combined exersie program improved the stair negotiation performance of older men and enabled them to control the postural sways and have better balance during stair ascending and descending. It was also associated with reduced time and increased velocity during stair ascending and descending, and increased stair self-efficacy in older men, which means improvement in stair negotiation performance. In the present study, the combined exersie program included stretching, resistance, strength, and balance exersies. Each of these components can enhance the balance and functional performance [11-14], and their combined effect on improving stair negotiation performance of older mem was confirmed in this study. This program covered different abilities required for performing daily activities [15]. Therefore, it can be expected that the program can improve the stair negotiation performance of older adults by affecting stair ascending and descending functional demands, including lower limb range of motion, strength, power, and balance control. Gavin et al. (2019), Lee et al. (2021), Handsiker et al. (2016), and Holsgaard et al. (2011) also showed the effectiveness of exercises in improving stair descending performance [16-19], which is consistent with the results of the present study. Considering the prevalence of stair climbing activities and their potential danger for the elderly and given the effectiveness of combined exercise program, these exercises are recommended for older adults.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by the Ethics Committee of the University of Isfahan (Code: IR.UI.REC.1398.081) and was registered by the Iranian Registry of Clinical Trials (Code: IRCT20180101038168N1). All participants read and signed the informed consent form, and their rights were reserved during the study.
Funding
This article was extracted from Mehdi Ghaderian’s PhD dissertation, approved by the Faculty of Sports Sciences, University of Isfahan, and was funded by University of Isfahan.
Authors' contributions
The authors contributed equally to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all seniors participated in this study as well as the University of Isfahan and the Faculty of Rehabilitation Sciences, Isfahan University of Medical Sciences for their cooperation in this research.
References
Aging is a global concern that is associated with a decline in organ function and makes a person vulnerable to diseases. Falling is one of the causes of injuries in older adults [1]. Stair climbing is a problematic activity and one of the most common causes of falls in older adults [2, 3]. The elderly are three times more likely to fall when walking up the stairs than when walking on the ground [4]. Balance disorders make stair climbing difficult for the elderly [5]. Controlling balance while climbing stairs is more difficult than that when walking [6]. Most of studies have focused on improving the balance of the elderly while walking, and less attention has been paid to their stair-climbing performance. The mechanisms of balance improvement are different. Combined and multi-component training programs may cause better results in balance improvement [7]. The present study aims to investigate the effect of combined exercises on the stair negotiation performance of older men.
Methods
This is a randomized controlled clinical trial with a pre-test/post-test design. Thirty older men were selected and randomly allocated to two parallel groups of intervention and control. The intervention group performed 12 weeks of combined exercises, while the control group continued their usual activities during this period. Inclusion criteria were age at least 60 years, functional independence, obtaining the required scores in the general health questionnaire-28, mini-mental state examination, and physical activity readiness questionnaire; no any medical and ethical restrictions, ability to complete tests and exercises, and no participation in other regular exercise programs. Exclusion criteria included an unwillingness to participate in tests and absence from exercise sessions. The participants performed the stair negotiation tests and their kinetic and kinematic data were recorded using the Kistler force plate and the Qualisys motion capture system. The balance was measured with the center of pressure (COP) parameters [1]. The stair ascending and descending time was calculated with kinematic data. Stair negotiation performance was evaluated with the timed up and down stairs (TUDS) test [8], and the self-efficacy was evaluated with the stair self-efficacy (SSE) scale [9]. The exercise protocol consisted of warm-up (10 minutes), resistance training (20 minutes), balance, hopping, and jump training (40 minutes), and cooling down (5 minutes) for 12 weeks. The overload principle was observed with a gradual increase in the duration, number, and load amount. Statistical analysis was carried out using mixed ANOVA. Pairwise comparison was done with the Bonferroni test, and the effect size (partial eta squared) was calculated [10]. The significance level was set at 0.05.
Results
Descriptive information and the results of mixed ANOVA for the stair negotiation variable are reported in Table 1.
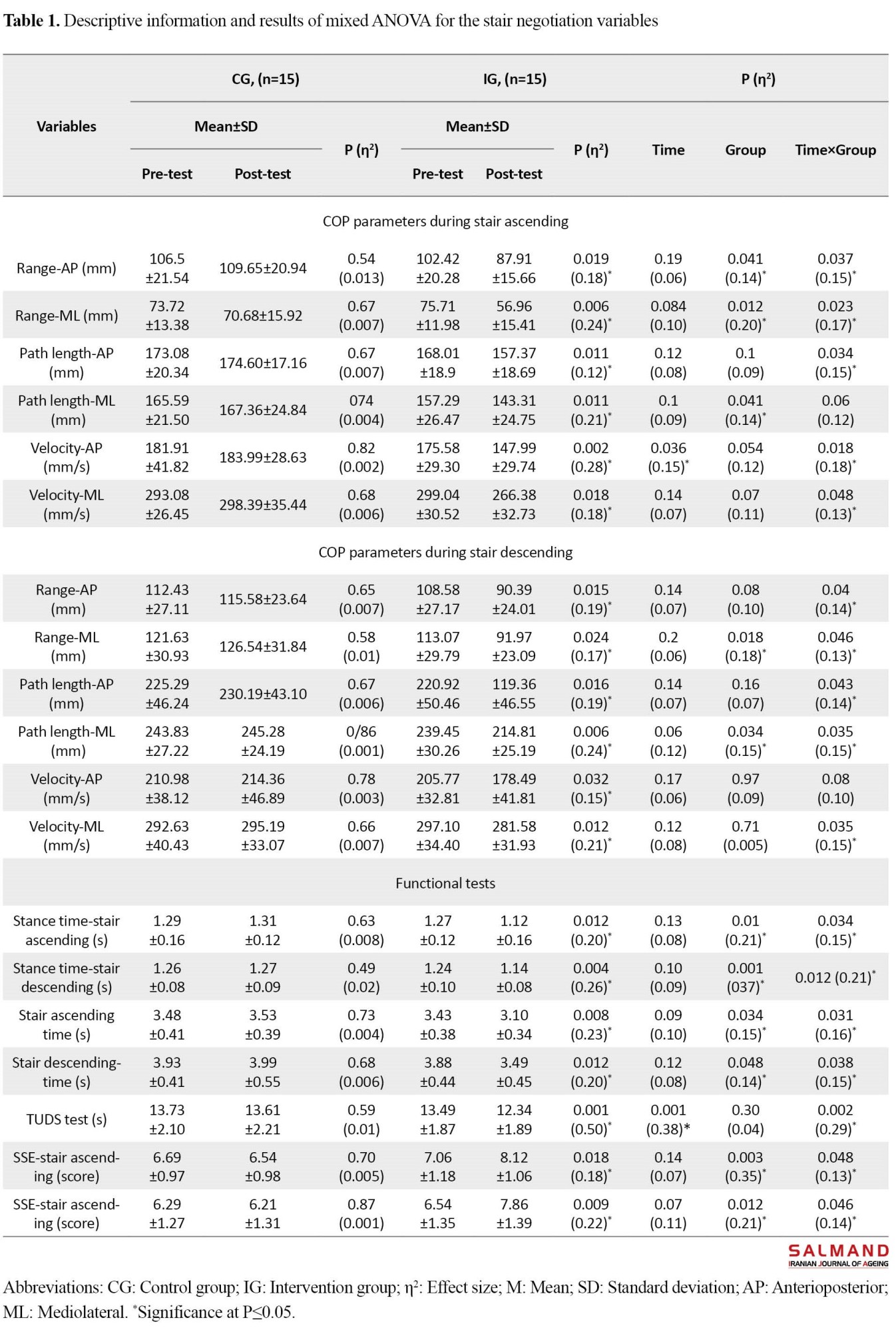
Interaction effects of the COP parameters, including range and velocity in anteroposterior and mediolateral directions, and path length in the anteroposterior direction were significant during stair ascending (P≤0.047, η2=0.12-0.18) as well as the range and path length in the anteroposterior and mediolateral directions and the velocity in the mediolateral direction during stair descending (P=0.046, η2=0.10-0.15), and in all functional tests variables (P=0.048, η2=0.13-0.29). The results of Bonferroni test showed a significant improvement in the variables in the post-test phase compared to the pre-test phase in the intervention group (P=0.032). No significant change was observed in any of the variables in the control group (P>0.05). The results showed a decrease in the COP parameters and an improvement in balance control during stair ascending and descending in the intervention group. Also, duration of stance phase, total time in stair ascending and descending, and the TUDS test time decreased and the stair self-efficacy was improved after exercises.
Conclusion
The results showed that the combined exersie program improved the stair negotiation performance of older men and enabled them to control the postural sways and have better balance during stair ascending and descending. It was also associated with reduced time and increased velocity during stair ascending and descending, and increased stair self-efficacy in older men, which means improvement in stair negotiation performance. In the present study, the combined exersie program included stretching, resistance, strength, and balance exersies. Each of these components can enhance the balance and functional performance [11-14], and their combined effect on improving stair negotiation performance of older mem was confirmed in this study. This program covered different abilities required for performing daily activities [15]. Therefore, it can be expected that the program can improve the stair negotiation performance of older adults by affecting stair ascending and descending functional demands, including lower limb range of motion, strength, power, and balance control. Gavin et al. (2019), Lee et al. (2021), Handsiker et al. (2016), and Holsgaard et al. (2011) also showed the effectiveness of exercises in improving stair descending performance [16-19], which is consistent with the results of the present study. Considering the prevalence of stair climbing activities and their potential danger for the elderly and given the effectiveness of combined exercise program, these exercises are recommended for older adults.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by the Ethics Committee of the University of Isfahan (Code: IR.UI.REC.1398.081) and was registered by the Iranian Registry of Clinical Trials (Code: IRCT20180101038168N1). All participants read and signed the informed consent form, and their rights were reserved during the study.
Funding
This article was extracted from Mehdi Ghaderian’s PhD dissertation, approved by the Faculty of Sports Sciences, University of Isfahan, and was funded by University of Isfahan.
Authors' contributions
The authors contributed equally to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all seniors participated in this study as well as the University of Isfahan and the Faculty of Rehabilitation Sciences, Isfahan University of Medical Sciences for their cooperation in this research.
References
- Shigematsu R, Chang M, Yabushita N, Sakai T, Nakagaichi M, Nho H, et al. Dance‐based aerobic exercise may improve indices of falling risk in older women. Age and Ageing. 2002; 31(4):261-6. [DOI:10.1093/ageing/31.4.261] [PMID]
- Mehdizadeh S, Van Ooteghem K, Gulka H, Nabavi H, Faieghi M, Taati B, et al. A systematic review of center of pressure measures to quantify gait changes in older adults. Experimental Gerontology. 2021; 143:111170. [DOI:10.1016/j.exger.2020.111170] [PMID]
- Stel VS, Smit JH, Pluijm SM, Lips P. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age and Ageing. 2004; 33(1):58-65. [DOI:10.1093/ageing/afh028] [PMID]
- Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, et al. Interventions for the prevention of falls in older adults: Systematic review and meta-analysis of randomised clinical trials. BMJ. 2004; 328(7441):680. [DOI:10.1136/bmj.328.7441.680] [PMID] [PMCID]
- Vaishya R, Vaish A. Falls in older adults are serious. Indian Journal of Orthopaedics. 2020; 54(1):69-74. [DOI:10.1007/s43465-019-00037-x] [PMID] [PMCID]
- Protopapadaki A, Drechsler WI, Cramp MC, Coutts FJ, Scott OM. Hip, knee, ankle kinematics and kinetics during stair ascent and descent in healthy young individuals. Clinical Biomechanics. 2007; 22(2):203-10. [DOI:10.1016/j.clinbiomech.2006.09.010] [PMID]
- Tiedemann AC, Sherrington C, Lord SR. Physical and psychological factors associated with stair negotiation performance in older people. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2007; 62(11):1259-65. [DOI:10.1093/gerona/62.11.1259] [PMID]
- Startzell JK, Owens DA, Mulfinger LM, Cavanagh PR. Stair negotiation in older people: A review. Journal of the American Geriatrics Society. 2000; 48(5):567-80. [DOI:10.1111/j.1532-5415.2000.tb05006.x] [PMID]
- Williamson JD, Fried LP. Characterization of older adults who attribute functional decrements to “old age”. Journal of the American Geriatrics Society. 1996; 44(12):1429-34. [DOI:10.1111/j.1532-5415.1996.tb04066.x] [PMID]
- Cohen HH, Templer J, Archea J. An analysis of occupational stair accident patterns. Journal of Safety Research. 1985; 16(4):171-81. [DOI:10.1016/0022-4375(85)90004-0]
- Roys MS. Serious stair injuries can be prevented by improved stair design. Applied Ergonomics. 2001; 32(2):135-9. [DOI:10.1016/S0003-6870(00)00049-1] [PMID]
- Buckley JG, Heasley K, Scally A, Elliott DB. The effects of blurring vision on medio-lateral balance during stepping up or down to a new level in the elderly. Gait & Posture. 2005; 22(2):146-53. [DOI:10.1016/j.gaitpost.2004.08.006] [PMID]
- Qu X. Effects of lower-limb muscular fatigue on stair gait. Journal of Biomechanics. 2015; 48(15):4059-64. [DOI:10.1016/j.jbiomech.2015.10.004] [PMID]
- Bosse I, Oberländer KD, Savelberg HH, Meijer K, Brüggemann G-P, Karamanidis K. Dynamic stability control in younger and older adults during stair descent. Human Movement Science. 2012; 31(6):1560-70. [DOI:10.1016/j.humov.2012.05.003] [PMID]
- Ojha HA, Kern RW, Lin CH, Winstein CJ. Age affects the attentional demands of stair ambulation: Evidence from a dual-task Approach. Physical Therapy. 2009; 89(10):1080-8. [DOI:10.2522/ptj.20080187] [PMID]
- Gavin JP, Reeves ND, Jones DA, Roys M, Buckley JG, Baltzopoulos V, et al. Combined resistance and stretching exercise training benefits stair descent biomechanics in older adults. Frontiers in Physiology. 2019; 10:873. [DOI:10.3389/fphys.2019.00873] [PMID] [PMCID]
- Silsupadol P, Siu KC, Shumway-Cook A, Woollacott MH. Training of balance under single-and dual-task conditions in older adults with balance impairment. Physical Therapy. 2006; 86(2):269-81. [DOI:10.1093/ptj/86.2.269] [PMID]
- Ren P, Huang S, Feng Y, Chen J, Wang Q, Guo Y, et al. Assessment of balance control subsystems by artificial intelligence. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2020; 28(3):658-68. [DOI:10.1109/TNSRE.2020.2966784] [PMID]
- Sibley KM, Beauchamp MK, Van Ooteghem K, Straus SE, Jaglal SB. Using the systems framework for postural control to analyze the components of balance evaluated in standardized balance measures: A scoping review. Archives of Physical Medicine and Rehabilitation. 2015; 96(1):122-32.e29. [DOI:10.1016/j.apmr.2014.06.021] [PMID]
- Westcott SL, Lowes LP, Richardson PK. Evaluation of postural stability in children: Current theories and assessment tools. Physical Therapy. 1997; 77(6):629-45. [DOI:10.1093/ptj/77.6.629] [PMID]
- Qu X, Hu X. Lower-extremity kinematics and postural stability during stair negotiation: Effects of two cognitive tasks. Clinical Biomechanics. 2014; 29(1):40-6. [DOI:10.1016/j.clinbiomech.2013.11.006] [PMID]
- Hwang HF, Cheng CH, Chien DK, Yu WY, Lin MR. Risk factors for traumatic brain injuries during falls in older persons. Journal of Head Trauma Rehabilitation. 2015; 30(6):E9-17. [DOI:10.1097/HTR.0000000000000093] [PMID]
- Alcock L, O’Brien TD, Vanicek N. Association between somatosensory, visual and vestibular contributions to postural control, reactive balance capacity and healthy ageing in older women. Health Care for Women International. 2018; 39(12):1366-80. [DOI:10.1080/07399332.2018.1499106] [PMID]
- Hortobágyi T, Mizelle C, Beam S, DeVita P. Old adults perform activities of daily living near their maximal capabilities. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2003; 58(5):M453-60. [DOI:10.1093/gerona/58.5.M453] [PMID]
- Sherrington C, Fairhall N, Wallbank G, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community: An abridged Cochrane systematic review. British Journal of Sports Medicine. 2020; 54(15):885-91. [DOI:10.1136/bjsports-2019-101512] [PMID]
- Thomas E, Battaglia G, Patti A, Brusa J, Leonardi V, Palma A, et al. Physical activity programs for balance and fall prevention in elderly: A systematic review. Medicine (Baltimore). 2019; 98(27):e16218. [DOI:10.1097/MD.0000000000016218] [PMID] [PMCID]
- Lesinski M, Hortobágyi T, Muehlbauer T, Gollhofer A, Granacher U. Effects of balance training on balance performance in healthy older adults: A systematic review and meta-analysis. Sports Medicine. 2015; 45(12):1721-38. [DOI:10.1007/s40279-015-0375-y] [PMID] [PMCID]
- Wang LC, Ye MZ, Xiong J, Wang XQ, Wu JW, Zheng GH. Optimal exercise parameters of tai chi for balance performance in older adults: A m eta‐analysis. Journal of the American Geriatrics Society. 2021; 69(7):2000-10. [DOI:10.1111/jgs.17094] [PMID]
- Li Y, Gao Y, Hu S, Chen H, Zhang M, Yang Y, et al. Effects of multicomponent exercise on the muscle strength, muscle endurance and balance of frail older adults: A meta‐analysis of randomised controlled trials. Journal of Clinical Nursing. 2023; 32(9-10):1795-805. [DOI:10.1111/jocn.16196]
- Zhang W, Low LF, Gwynn JD, Clemson L. Interventions to improve gait in older adults with cognitive impairment: A systematic review. Journal of the American Geriatrics Society. 2019; 67(2):381-91. [DOI:10.1111/jgs.15660] [PMID]
- Farahpour N, Shayeste M, Jafarnezhadgero A. [A comparison of squat and leg press training protocols on center of pressure alterations and ground reaction force during step descent (Persian)]. Journal of Applied Exercise Physiology. 2018; 13(26):213-24. [Link]
- Kim HD, Han JT, Cho YH. The effectiveness of community-based Tai Chi training on balance control during stair descent by older adults. Journal of Physical Therapy Science. 2009; 21(4):317-23. [DOI:10.1589/jpts.21.317]
- Jadczak AD, Makwana N, Luscombe-Marsh N, Visvanathan R, Schultz TJ. Effectiveness of exercise interventions on physical function in community-dwelling frail older people: An umbrella review of systematic reviews. JBI Database of Systematic Reviews and Implementation Reports. 2018; 16(3):752-75. [DOI:10.11124/JBISRIR-2017-003551] [PMID]
- Campani D, Caristia S, Amariglio A, Piscone S, Ferrara LI, Bortoluzzi S, et al. Effective, sustainable, and transferable physical exercise interventions for fall prevention among older people. Public Health Nursing. 2021; 38(6):1140-76. [DOI:10.1111/phn.12949] [PMID]
- Jacobs JV. A review of stairway falls and stair negotiation: Lessons learned and future needs to reduce injury. Gait & Posture. 2016; 49:159-67. [DOI:10.1016/j.gaitpost.2016.06.030] [PMID]
- Jofré-Saldía E, Villalobos-Gorigoitía Á, Gea-García G. Effects of multicomponent exercise program with progressive phases on functional capacity, fitness, quality of life, dual-task and physiological variables in older adults: Randomized controlled trial protocol. Revista Española de Geriatría y Gerontología. 2021; 56(5):272-8. [DOI:10.1016/j.regg.2021.04.006] [PMID]
- Jafarnezhadgero A, Madadi-Shad M, McCrum C, Karamanidis K. Effects of corrective training on drop landing ground reaction force characteristics and lower limb kinematics in older adults with genu valgus: A randomized controlled trial. Journal of Aging and Physical Activity. 2019; 27(1):9-17. [DOI:10.1123/japa.2017-0315] [PMID]
- Hamel KA, Okita N, Bus SA, Cavanagh PR. A comparison of foot/ground interaction during stair negotiation and level walking in young and older women. Ergonomics. 2005; 48(8):1047-56. [DOI:10.1080/00140130500193665] [PMID]
- Yu B. Effect of external marker sets on between-day reproducibility of knee kinematics and kinetics in stair climbing and level walking. Research in Sports Medicine. 2003; 11(4):209-18. [DOI:10.1080/714041037] [PMID]
- Li KW, Huang SY, Chiu WH. Ground reaction force and required friction during stair ascent and descent. Human Factors and Ergonomics in Manufacturing & Service Industries. 2017; 27(1):66-73. [DOI:10.1002/hfm.20691]
- Jafarnezhadgero A, Fatollahi A, Amirzadeh N, Siahkouhian M, Granacher U. Ground reaction forces and muscle activity while walking on sand versus stable ground in individuals with pronated feet compared with healthy controls. PloS One. 2019; 14(9):e0223219. [DOI:10.1371/journal.pone.0223219] [PMID] [PMCID]
- Oh-Park M, Perera S, Verghese J. Clinically meaningful change in stair negotiation performance in older adults. Gait & Posture. 2012; 36(3):532-6. [DOI:10.1016/j.gaitpost.2012.05.015] [PMID] [PMCID]
- Del Corral T, Vivas-Mateos J, Castillo-Pelaz M, Aguilar-Zafra S, López-de-Uralde-Villanueva I. Development of stratified normative data and reference equations for the timed up and down stairs test for healthy children 6-14 years of age. Physiotherapy. 2021; 112:31-40. [DOI:10.1016/j.physio.2021.03.002] [PMID]
- Altmeier D, Kempe M, Memmert D. Stair self-efficacy questionnaire to test the ability of stair negotiation for older people. German Journal of Exercise and Sport Research. 2018; 48(1):40-7. [DOI:10.1007/s12662-017-0483-y]
- Hamel KA, Cavanagh PR. Stair performance in people aged 75 and older. Journal of the American Geriatrics Society. 2004; 52(4):563-7. [DOI:10.1111/j.1532-5415.2004.52162.x] [PMID]
- Best-Martini E, Jones-DiGenova KA. Exercise for frail elders. Champaign: Human kinetics; 2014. [DOI:10.5040/9781492597353]
- Cutler K. Home exercise guide for adults and seniors: Fitness and nutrition. Lost temple fitness: Strength, balance, flexibility, myofascial release, nutrition. California: CreateSpace; 2018. [Link]
- Baechle TR, Westcott WL. Fitness professionals guide to strength training older adults. Champaign: Human Kinetics Publishers; 2010. [Link]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007; 116(9):1094-105. [DOI:10.1161/CIRCULATIONAHA.107.185650] [PMID]
- Richardson JT. Eta squared and partial eta squared as measures of effect size in educational research. Educational Research Review. 2011; 6(2):135-47. [DOI:10.1016/j.edurev.2010.12.001]
- Dutil M, Handrigan GA, Corbeil P, Cantin V, Simoneau M, Teasdale N, et al. The impact of obesity on balance control in community-dwelling older women. Age (Dordr). 2013; 35(3):883-90. [DOI:10.1007/s11357-012-9386-x] [PMID] [PMCID]
- Raymakers JA, Samson MM, Verhaar HJ. The assessment of body sway and the choice of the stability parameter (s). Gait & Posture. 2005; 21(1):48-58. [DOI:10.1016/j.gaitpost.2003.11.006] [PMID]
- Wu R, De Vito G, Delahunt E, Ditroilo M. Age-related changes in motor function (I). Mechanical and neuromuscular factors. International Journal of Sports Medicine. 2020; 41(11):709-19. [DOI:10.1055/a-1144-3408]
- Wang SJ, Xu DQ, Su LN, Li JX. Effect of long-term exercise training on static postural control in older adults: A cross-sectional study. Research in Sports Medicine. 2020; 28(4):553-62. [DOI:10.1080/15438627.2020.1795661] [PMID]
- Low DC, Walsh GS, Arkesteijn M. Effectiveness of exercise interventions to improve postural control in older adults: A systematic review and meta-analyses of centre of pressure measurements. Sports Medicine. 2017; 47(1):101-12. [DOI:10.1007/s40279-016-0559-0] [PMID] [PMCID]
- Lemos ECWM, Guadagnin EC, Mota CB. Influence of strength training and multicomponent training on the functionality of older adults: Systematic review and meta-analysis. Revista Brasileira de Cineantropometria & Desempenho Humano. 2020; 22. [DOI:10.1590/1980-0037.2020v22e6070]
- Zouita S, Zouhal H, Ferchichi H, Paillard T, Dziri C, Hackney AC, et al. Effects of combined balance and strength training on measures of balance and muscle strength in older women with a history of falls. Frontiers in Physiology. 2020; 11:619016.[DOI:10.3389/fphys.2020.619016] [PMID] [PMCID]
- Li Y, Song Q, Li L, Sun W, Zhang C. Tai Chi practitioners have lower fall risks under dual-task conditions during stair descending. Plos One. 2021; 16(2):e0246292. [DOI:10.1371/journal.pone.0246292] [PMID] [PMCID]
- Handsaker JC, Brown SJ, Bowling FL, Maganaris CN, Boulton AJ, Reeves ND. Resistance exercise training increases lower limb speed of strength generation during stair ascent and descent in people with diabetic peripheral neuropathy. Diabetic Medicine. 2016; 33(1):97-104. [DOI:10.1111/dme.12841] [PMID]
- Holsgaard-Larsen A, Caserotti P, Puggaard L, Aagaard P. Stair-ascent performance in elderly women: Effect of explosive strength training. Journal of Aging and Physical Activity. 2011; 19(2):117-36. [DOI:10.1123/japa.19.2.117] [PMID]
- Vittala G, Sundari LPR, Basuki N, Kuswardhani RAT, Purnawati S, Muliarta IM. The addition of active stretching to balance strategy exercise is the most effective as a home-based exercise program in improving the balance of the elderly. Journal of Mid-Life Health. 2021; 12(4):294-8. [DOI:10.4103/jmh.jmh_184_21] [PMID] [PMCID]
- Drozdova-Statkevičienė M, Česnaitienė VJ, Levin O, Pauwels L, Pukėnas K, Helsen WF, et al. The beneficial effects of acute strength training on sway activity and sway regularity in healthy older men: Evidence from a posturography study. Neuroscience Letters. 2021; 749:135718. [DOI:10.1016/j.neulet.2021.135718] [PMID]
- Piirainen JM, Cronin NJ, Avela J, Linnamo V. Effects of plyometric and pneumatic explosive strength training on neuromuscular function and dynamic balance control in 60-70 year old males. Journal of Electromyography and Kinesiology. 2014; 24(2):246-52. [DOI:10.1016/j.jelekin.2014.01.010] [PMID]
- Behm DG, Kay AD, Trajano GS, Alizadeh S, Blazevich AJ. Effects of stretching on injury risk reduction and balance. Journal of Clinical Exercise Physiology. 2021; 10(3):106-16. [DOI:10.31189/2165-6193-10.3.106]
- Vetrovsky T, Steffl M, Stastny P, Tufano JJ. The efficacy and safety of lower-limb plyometric training in older adults: A systematic review. Sports Medicine. 2019; 49(1):113-31. [DOI:10.1007/s40279-018-1018-x] [PMID] [PMCID]
- Moran J, Ramirez-Campillo R, Granacher U. Effects of jumping exercise on muscular power in older adults: A meta-analysis. Sports Medicine. 2018; 48(12):2843-57. [DOI:10.1007/s40279-018-1002-5] [PMID]
- Lee HJ, Chou LS. Balance control during stair negotiation in older adults. Journal of Biomechanics. 2007; 40(11):2530-6. [DOI:10.1016/j.jbiomech.2006.11.001] [PMID]
- Rogers ME, Page P, Takeshima N. Balance training for the older athlete. International Journal of Sports Physical Therapy. 2013; 8(4):517-30. [PMID]
- Wolf R, Locks RR, Lopes PB, Bento PCB, Rodacki ALF, Carraro AN, et al. Multicomponent exercise training improves gait ability of older women rather than strength training: A randomized controlled trial. Journal of Aging Research. 2020; 2020:6345753. [DOI:10.1155/2020/6345753] [PMID] [PMCID]
- Brustio PR, Magistro D, Liubicich ME. Changes in temporal parameters during performance of the Step Test in older adults. Gait & Posture. 2015; 41(1):217-21. [DOI:10.1016/j.gaitpost.2014.10.006] [PMID]
- Zietz D, Johannsen L, Hollands M. Stepping characteristics and centre of mass control during stair descent: Effects of age, fall risk and visual factors. Gait & Posture. 2011; 34(2):279-84. [DOI:10.1016/j.gaitpost.2011.05.017] [PMID]
- Nightingale EJ, Pourkazemi F, Hiller CE. Systematic review of timed stair tests. Journal of Rehabilitation Research and Development. 2014; 51(3):335-50. [DOI:10.1682/JRRD.2013.06.0148] [PMID]
- Oh-Park M, Wang C, Verghese J. Stair negotiation time in community-dwelling older adults: Normative values and association with functional decline. Archives of Physical Medicine and Rehabilitation. 2011; 92(12):2006-11. [DOI:10.1016/j.apmr.2011.07.193] [PMID] [PMCID]
- Yang TH, Huang CF. Stepping characteristics before stair walking transitons in taichi elderly. ISBS-Conference Proceedings Archive. 2013; 1-3. [Link]
- Novak AC, Brouwer B. Sagittal and frontal lower limb joint moments during stair ascent and descent in young and older adults. Gait & Posture. 2011; 33(1):54-60. [DOI:10.1016/j.gaitpost.2010.09.024] [PMID]
- Hortobágyi T, Lesinski M, Gäbler M, VanSwearingen JM, Malatesta D, Granacher U. Effects of three types of exercise interventions on healthy old adults’ gait speed: A systematic review and meta-analysis. Sports Medicine. 2015; 45(12):1627-43. [DOI:10.1007/s40279-015-0371-2] [PMID] [PMCID]
- Lopopolo RB, Greco M, Sullivan D, Craik RL, Mangione KK. Effect of therapeutic exercise on gait speed in community-dwelling elderly people: A meta-analysis. Physical Therapy. 2006; 86(4):520-40. [DOI:10.1093/ptj/86.4.520] [PMID]
- LaRoche DP, Millett ED, Kralian RJ. Low strength is related to diminished ground reaction forces and walking performance in older women. Gait & Posture. 2011; 33(4):668-72. [DOI:10.1016/j.gaitpost.2011.02.022] [PMID] [PMCID]
- LaStayo PC, Ewy GA, Pierotti DD, Johns RK, Lindstedt S. The positive effects of negative work: Increased muscle strength and decreased fall risk in a frail elderly population. The Journals of Gerontology: Series A. 2003; 58(5):M419-24. [DOI:10.1093/gerona/58.5.M419] [PMID]
- Fiatarone MA, O’Neill EF, Ryan ND, Clements KM, Solares GR, Nelson ME, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. New England Journal of Medicine. 1994; 330(25):1769-75. [DOI:10.1056/NEJM199406233302501] [PMID]
- Mian OS, Thom JM, Narici MV, Baltzopoulos V. Kinematics of stair descent in young and older adults and the impact of exercise training. Gait & Posture. 2007; 25(1):9-17. [DOI:10.1016/j.gaitpost.2005.12.014] [PMID]
- Allen MD, Dalton BH, Gilmore KJ, McNeil CJ, Doherty TJ, Rice CL, et al. Neuroprotective effects of exercise on the aging human neuromuscular system. Experimental Gerontology. 2021; 152:111465. [DOI:10.1016/j.exger.2021.111465] [PMID]
- Halvarsson A, Franzén E, Ståhle A. Balance training with multi-task exercises improves fall-related self-efficacy, gait, balance performance and physical function in older adults with osteoporosis: A randomized controlled trial. Clinical Rehabilitation. 2015; 29(4):365-75. [DOI:10.1177/0269215514544983] [PMID]
Type of Study: Research |
Subject:
Geriatric
Received: 2022/06/09 | Accepted: 2022/08/30 | Published: 2023/10/01
Received: 2022/06/09 | Accepted: 2022/08/30 | Published: 2023/10/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








