Volume 18, Issue 3 (Autumn 2023)
Salmand: Iranian Journal of Ageing 2023, 18(3): 424-437 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Amani A, Akbari Kamrani A A, Fadayevatan R, Eshrati B, Rafiee M. Burden of Important Risk Factors for Common Cancers Among Older Adults in Markazi Province, Iran in 2016. Salmand: Iranian Journal of Ageing 2023; 18 (3) :424-437
URL: http://salmandj.uswr.ac.ir/article-1-2492-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2492-en.html
1- Department of Geriatrics, School of Social Welfare, University of Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Geriatrics, School of Social Welfare, University of Welfare and Rehabilitation Sciences, Tehran, Iran. ,akbarikamrani@uswr.ac.ir
3- Preventive Medicine and Public Health Research Center, Social Injury Prevention Research Institute, Iran University of Medical Sciences.
4- Department of Biostatistics, School of Medicine, Arak University of Medical Sciences, Arak, Iran.
2- Department of Geriatrics, School of Social Welfare, University of Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Preventive Medicine and Public Health Research Center, Social Injury Prevention Research Institute, Iran University of Medical Sciences.
4- Department of Biostatistics, School of Medicine, Arak University of Medical Sciences, Arak, Iran.
Full-Text [PDF 5497 kb]
(1195 Downloads)
| Abstract (HTML) (3218 Views)
Full-Text: (1686 Views)
Introduction
The burden of disease analysis is a method that can integrate the fetal and non-fetal data and provide a summary measure named the disability-adjusted life years, which indicates the total number of years lost as a result of premature death or disability [2]. Considering the high prevalence of cancers in the elderly group and that awareness of the risk factors attributed to cancer can help in macro-level planning in prevention, the present study was designed to calculate the burden of risk factors attributed to common cancers in the elderly living in Markazi Province of Iran in 2016. The results can help the officials and policymakers in the field of health to develop healthy lifestyle programs and cancer screening programs in this region.
Methods
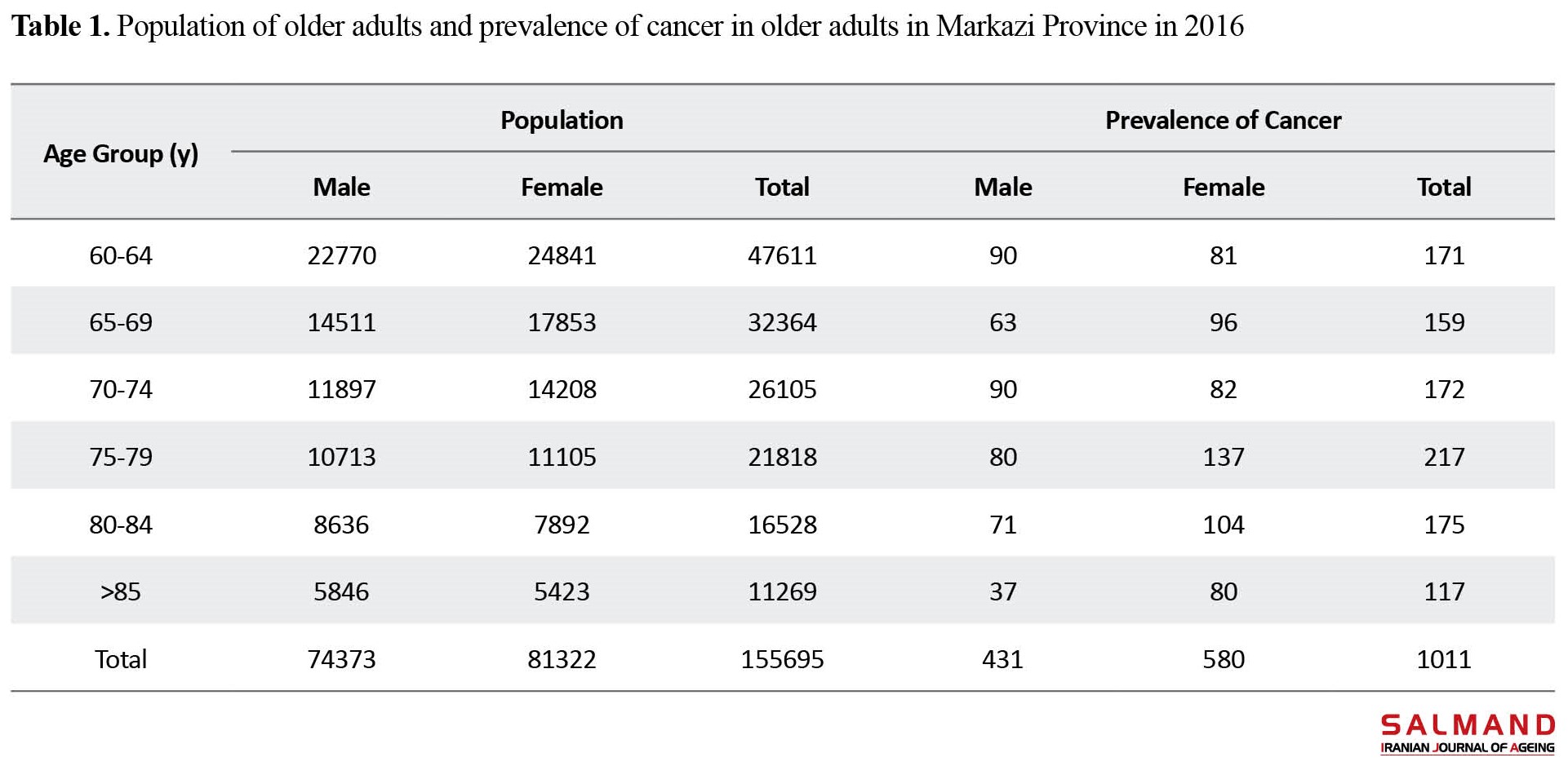
This is a retrospective descriptive-analytical study. The data of older people with cancer or those who died from cancer aged >60 years and lived in Markazi Province for more than 6 months were selected using a census method over one year. These data included: Cancer incidence rate by age group, cancer death rate by age group, average age of cancer death, average age of onset of cancer and average duration of the disease by age and sex groups, standard life expectancy, average age of onset of cancer using patient data available in death registration system, duration of the disease from the time of infection to the time of death or (in rare cases) recovery and the data of the risk factors for cancer using the death registration system and the last national cancer survey report in 2017. The data were first processed in Excel software and were then entered into DisMod II software and the necessary calculations were performed. Cancer diagnosis criteria in this study were based on the 10th version of the international statistical classification of diseases. Demographic information was obtained from the website of the Iranian Statistics Center, and risk factors were extracted from the cancer registration system. The Equation 1 was used to measure the effect of each risk factor on each type of cancers in the elderly [3]:
In this equation, PIF is the potential impact fraction, Pi is the observed prevalence of the risk factor i, pi is the counter factual prevalence of the risk factor i, and RRi is the relative risk of i.
Results
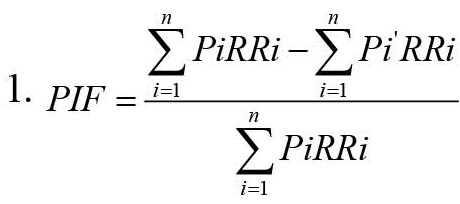
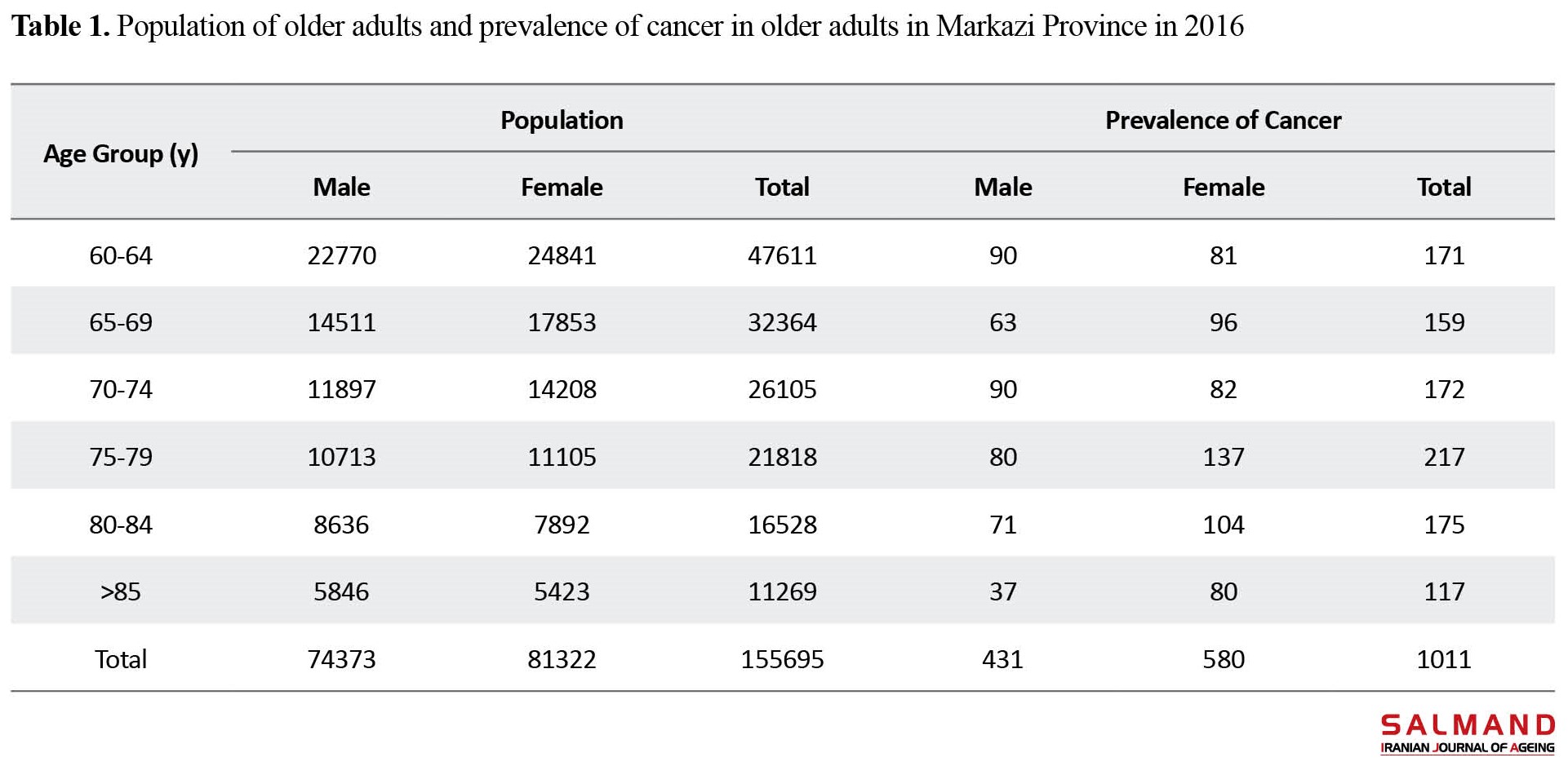
Based on the census report of 2016 in Iran, the population of Markazi Province was estimated at 1429475 people, of whom 155695(10.9%) had 60 years old or higher. There were 1769 new cases of cancer in the province in 2016, of which 1011(57.15%) occurred in the elderly group (Table 1).
In calculating the burden of different risk factors for different types of cancer, the results showed that:
For skin cancer, the highest burden was related to exposure to sunlight (526.71), while the lowest burden was attributed to alcohol consumption (95.22).
For gastric cancer, the highest burden was related to family history (79305.88), while the lowest burden was related to alcohol consumption (2676.23).
For colon cancer, the highest burden was related to not consuming fruits (4063.18), while the lowest burden was related to obesity (408.87).
For breast cancer, the highest burden was related to not being married (6488.58), while the lowest burden was related to the age of menstruation (49.91).
For lung cancer, the highest burden was related to smoking (2646.53), while the lowest burden was related to not consuming fruits (37.14).
For bladder cancer, the highest burden was related to family history (10194.71), while the lowest burden was related to having a high-risk job (109.91).
For ovarian cancer, the highest burden was related to obesity (13129.21), while the lowest burden was related to alcohol use (81.88).
For prostate cancer, the highest burden was related to a history of previous diseases (7244.08), while the lowest burden was related to lack of physical activity (1656.59).
Conclusion
The findings of the present study showed that exposure to sunlight, family history, lack of fruit consumption, lack of marriage, smoking, obesity, and history of previous diseases are the most common risk factors for skin, gastric, colon, breast, lung, ovarian, and prostate cancers. In the present study, the burden of skin cancer was lower compared to other cancers, which can be due to its proper treatment, as well as its better response to treatment and longer life expectancy of patients. Оshyvalova also showed that the non-use of sunscreen and family history were the greatest risk factors for skin cancer [4]. In our study, the highest burden for gastric cancer was family history, while the lowest burden was related to alcohol consumption. In a systematic review study in 2018, Yousefi et al concluded that several factors, including diet, lifestyle, and level of education and awareness of patients, have a role in the risk of gastric cancer [5]. The findings of Lewandowska et al. in 2022 showed that obesity, low physical activity, active and passive smoking, and high consumption of salt and red meat were associated with an increased risk of colon cancer [6]. This is consistent with our results. In the present study, the highest burden of breast cancer was attributed to not being married, family history, and infection, while the age of menstruation had the lowest burden for breast cancer. The findings of a study in 2021 showed that factors such as body mass index, age, and number of births were among the most important factors affecting breast cancer [7].
Ethical Considerations
Compliance with ethical guidelines
To consider the ethical principles, the personal information of the patients was kept confidential. This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1396.326).
Funding
This study was extracted from the PhD dissertation of Ahmad Amani, approved by Department of Geriatrics, School of Social Welfare, University of Social Welfare and Rehabilitation Sciences, and was funded by the University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
Methodology, investigation, funding acquisition, resources and writing the original draft: All authors; Conceptualization, supervision, review & editing: Ahmad Ali Akbari Kamrani.
Conflicts of interest
The authors declared no conflict of interest.
References
The burden of disease analysis is a method that can integrate the fetal and non-fetal data and provide a summary measure named the disability-adjusted life years, which indicates the total number of years lost as a result of premature death or disability [2]. Considering the high prevalence of cancers in the elderly group and that awareness of the risk factors attributed to cancer can help in macro-level planning in prevention, the present study was designed to calculate the burden of risk factors attributed to common cancers in the elderly living in Markazi Province of Iran in 2016. The results can help the officials and policymakers in the field of health to develop healthy lifestyle programs and cancer screening programs in this region.
Methods
This is a retrospective descriptive-analytical study. The data of older people with cancer or those who died from cancer aged >60 years and lived in Markazi Province for more than 6 months were selected using a census method over one year. These data included: Cancer incidence rate by age group, cancer death rate by age group, average age of cancer death, average age of onset of cancer and average duration of the disease by age and sex groups, standard life expectancy, average age of onset of cancer using patient data available in death registration system, duration of the disease from the time of infection to the time of death or (in rare cases) recovery and the data of the risk factors for cancer using the death registration system and the last national cancer survey report in 2017. The data were first processed in Excel software and were then entered into DisMod II software and the necessary calculations were performed. Cancer diagnosis criteria in this study were based on the 10th version of the international statistical classification of diseases. Demographic information was obtained from the website of the Iranian Statistics Center, and risk factors were extracted from the cancer registration system. The Equation 1 was used to measure the effect of each risk factor on each type of cancers in the elderly [3]:
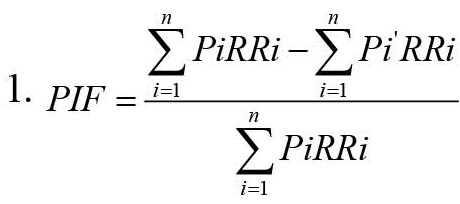
In this equation, PIF is the potential impact fraction, Pi is the observed prevalence of the risk factor i, pi is the counter factual prevalence of the risk factor i, and RRi is the relative risk of i.
Results
Based on the census report of 2016 in Iran, the population of Markazi Province was estimated at 1429475 people, of whom 155695(10.9%) had 60 years old or higher. There were 1769 new cases of cancer in the province in 2016, of which 1011(57.15%) occurred in the elderly group (Table 1).
In calculating the burden of different risk factors for different types of cancer, the results showed that:
For skin cancer, the highest burden was related to exposure to sunlight (526.71), while the lowest burden was attributed to alcohol consumption (95.22).
For gastric cancer, the highest burden was related to family history (79305.88), while the lowest burden was related to alcohol consumption (2676.23).
For colon cancer, the highest burden was related to not consuming fruits (4063.18), while the lowest burden was related to obesity (408.87).
For breast cancer, the highest burden was related to not being married (6488.58), while the lowest burden was related to the age of menstruation (49.91).
For lung cancer, the highest burden was related to smoking (2646.53), while the lowest burden was related to not consuming fruits (37.14).
For bladder cancer, the highest burden was related to family history (10194.71), while the lowest burden was related to having a high-risk job (109.91).
For ovarian cancer, the highest burden was related to obesity (13129.21), while the lowest burden was related to alcohol use (81.88).
For prostate cancer, the highest burden was related to a history of previous diseases (7244.08), while the lowest burden was related to lack of physical activity (1656.59).
Conclusion
The findings of the present study showed that exposure to sunlight, family history, lack of fruit consumption, lack of marriage, smoking, obesity, and history of previous diseases are the most common risk factors for skin, gastric, colon, breast, lung, ovarian, and prostate cancers. In the present study, the burden of skin cancer was lower compared to other cancers, which can be due to its proper treatment, as well as its better response to treatment and longer life expectancy of patients. Оshyvalova also showed that the non-use of sunscreen and family history were the greatest risk factors for skin cancer [4]. In our study, the highest burden for gastric cancer was family history, while the lowest burden was related to alcohol consumption. In a systematic review study in 2018, Yousefi et al concluded that several factors, including diet, lifestyle, and level of education and awareness of patients, have a role in the risk of gastric cancer [5]. The findings of Lewandowska et al. in 2022 showed that obesity, low physical activity, active and passive smoking, and high consumption of salt and red meat were associated with an increased risk of colon cancer [6]. This is consistent with our results. In the present study, the highest burden of breast cancer was attributed to not being married, family history, and infection, while the age of menstruation had the lowest burden for breast cancer. The findings of a study in 2021 showed that factors such as body mass index, age, and number of births were among the most important factors affecting breast cancer [7].
Ethical Considerations
Compliance with ethical guidelines
To consider the ethical principles, the personal information of the patients was kept confidential. This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1396.326).
Funding
This study was extracted from the PhD dissertation of Ahmad Amani, approved by Department of Geriatrics, School of Social Welfare, University of Social Welfare and Rehabilitation Sciences, and was funded by the University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
Methodology, investigation, funding acquisition, resources and writing the original draft: All authors; Conceptualization, supervision, review & editing: Ahmad Ali Akbari Kamrani.
Conflicts of interest
The authors declared no conflict of interest.
References
- Lopez AD. The evolution of the Global Burden of Disease framework for disease, injury and risk factor quantification: Developing the evidence base for national, regional and global public health action. Globalization and Health. 2005; 1(1):5. [DOI:10.1186/1744-8603-1-5] [PMID] [PMCID]
- Lincoln D, Muscatello D. Burden of disease New South Wales-Feasibility Report. New South Wales Public Health Bulletin Supplementary Series. 2002; 13(5):1-37. [DOI:10.1071/NB02S50]
- Global Burden of Disease Cancer Collaboration. The global burden of cancer 2013. JAMA Oncology. 2015; 1(4):505-27. [Link]
- World Health Organization. The world heath report 2002: Reducing risks, promoting healthy life. Geneva: World Health Organization; 2002. [Link]
- O’Donovan MR, Sezgin D, Liew A, O’Caoimh R. Burden of disease, disability-adjusted life years and frailty prevalence. QJM : Monthly Journal of the Association of Physicians. 2019; 112(4):261-7. [DOI:10.1093/qjmed/hcy291] [PMID]
- Rezagholi T, Yavari P, Abolhasani F, Etemad K, Khosravi A, Hashemi Nazari S, et al. [Estimating the burden of breast cancer in Iranian Women in 2009 (Persian)]. Iranian Journal of Epidemiology. 2015; 10(4):32-40. [Link]
- Tsilidis KK, Papadimitriou N, Capothanassi D, Bamia C, Benetou V, Jenab M, et al. Burden of cancer in a large consortium of prospective cohorts in Europe. Journal of The National Cancer Institute. 2016; 108(10):djw127. [DOI:10.1093/jnci/djw127]
- Mathers CD, Vos ET, Stevenson CE, Begg SJ. The Australian burden of disease study: Measuring the loss of health from diseases, injuries and risk factors. The Medical Journal of Australia. 2000; 172(12):592-6. [DOI:10.5694/j.1326-5377.2000.tb124125.x] [PMID]
- Naghavi M, Abolhassani F, Pourmalek F, Lakeh M, Jafari N, Vaseghi S, et al. The burden of disease and injury in Iran 2003. Popul Health Metr. 2009; 7:9. [PMID]
- Gordon R. Skin cancer: An overview of epidemiology and risk factors. Seminars in Oncology Nursing. 2013; 29(3):160-9. [DOI:10.1016/j.soncn.2013.06.002] [PMID]
- Оshyvalova ОО. Studying risk factors for skin cancer development. Wiadomosci Lekarskie. 2017; 70(3 pt 1):503-7. [PMID]
- Shih ST, Carter R, Sinclair C, Mihalopoulos C, Vos T. Economic evaluation of skin cancer prevention in Australia. Preventive Medicine. 2009; 49(5):449-53. [DOI:10.1016/j.ypmed.2009.09.008] [PMID]
- Yusefi AR, Bagheri Lankarani K, Bastani P, Radinmanesh M, Kavosi Z. Risk factors for gastric cancer: A systematic review. Asian Pacific Journal of Cancer Prevention. 2018; 19(3):591-603. [PMID]
- Poorolajal J, Moradi L, Mohammadi Y, Cheraghi Z, Gohari-Ensaf F. Risk factors for stomach cancer: A systematic review and meta-analysis. Epidemiology and Health. 2020; 42:e2020004. [DOI:10.4178/epih.e2020004] [PMID] [PMCID]
- Center MM, Jemal A, Ward E. International trends in colorectal cancer incidence rates. Cancer Epidemiology and Prevention Biomarkers. 2009; 18(6):1688-94. [DOI:10.1158/1055-9965.EPI-09-0090] [PMID]
- Lewandowska A, Rudzki G, Lewandowski T, Stryjkowska-Góra A, Rudzki S. Title: Risk factors for the diagnosis of colorectal cancer. Cancer Control. 2022; 29:10732748211056692. [DOI:10.1177/10732748211056692] [PMID] [PMCID]
- Johnson CM, Wei C, Ensor JE, Smolenski DJ, Amos CI, Levin B, et al. Meta-analyses of colorectal cancer risk factors. Cancer Causes Control. 2013; 24(6):1207-22. [DOI:10.1007/s10552-013-0201-5] [PMID] [PMCID]
- Shih ST, Carter R, Heward S, Sinclair C. Economic evaluation of future skin cancer prevention in Australia. Preventive Medicine. 2017; 99:7-12. [DOI:10.1016/j.ypmed.2017.01.013] [PMID]
- Mbeje NP, Ginindza T, Jafta N. Epidemiological study of risk factors for lung cancer in KwaZulu-Natal, South Africa. International Journal of Environmental Research and Public Health. 2022; 19(11):6752. [DOI:10.3390/ijerph19116752] [PMID] [PMCID]
- Mohaghegh F, Hamta A, Shariatzade MA. [The study of cancer incidence and cancer registration in Markazi province between 2001-2006 and comparison with national statistics, Iran (Persian)]. Journal of Arak University of Medical Sciences. 2008; 11(2):84-93. [Link]
- Cumberbatch MGK, Jubber I, Black PC, Esperto F, Figueroa JD, Kamat AM, et al. Epidemiology of bladder cancer: A systematic review and contemporary update of risk factors in 2018. European Urology. 2018; 74(6):784-95. [DOI:10.1016/j.eururo.2018.09.001] [PMID]
- Salehi A, Khezri AA, Malekmakan L, Aminsharifi A. Epidemiologic status of bladder cancer in Shiraz, southern Iran. Asian Pacific Journal of Cancer Prevention. 2011; 12(5):1323-7. [PMID]
- Łukasiewicz S, Czeczelewski M, Forma A, Baj J, Sitarz R, Stanisławek A. Breast cancer-epidemiology, risk factors, classification, prognostic markers, and current treatment strategies-An updated review. Cancers. 2021; 13(17):4287. [DOI:10.3390/cancers13174287] [PMID] [PMCID]
- Mousavi SM, Montazeri A, Mohagheghi MA, Jarrahi AM, Harirchi I, Najafi M, et al. Breast cancer in Iran: An epidemiological review. The Breast Journal. 2007; 13(4):383-91. [DOI:10.1111/j.1524-4741.2007.00446.x] [PMID]
- Collaborative Group On Epidemiological Studies Of Ovarian Cancer; Beral V, Gaitskell K, Hermon C, Moser K, Reeves G, et al. Menopausal hormone use and ovarian cancer risk: Individual participant meta-analysis of 52 epidemiological studies. The Lancet. 2015; 385(9980):1835-42. [DOI:10.1016/S0140-6736(14)61687-1] [PMID]
- Elshami M, Tuffaha A, Yaseen A, Alser M, Al-Slaibi I, Jabr H, et al. Awareness of ovarian cancer risk and protective factors: A national cross-sectional study from Palestine. PLoS One. 2022; 17(3):e0265452. [DOI:10.1371/journal.pone.0265452] [PMID] [PMCID]
- Abad M, Gangy R, Sharifian E, Nikdel R, Jafarzadeh M, Jafarzadeh F. [Epidemiologic distribution of cancer in a 10-yearstudy: Retrospective review of hospital records and pathology centers of North Khorasan Province from 2003 to 2012 (Persian)]. Journal of North Khorasan University of Medical Sciences. 2015; 6(4):689-96. [DOI:10.29252/jnkums.6.4.689]
- Sim HG, Cheng CW. Changing demography of prostate cancer in Asia. European Journal of Cancer. 2005; 41(6):834-45. [DOI:10.1016/j.ejca.2004.12.033] [PMID]
- Pourmand G, Salem S, Mehrsai A, Lotfi M, Amirzargar MA, Mazdak H, et al. The risk factors of prostate cancer: A multicentric case-control study in Iran. Asian Pacific Journal of Cancer Prevention. 2007; 8(3):422-8. [PMID]
- Sadjadi A, Nooraie M, Ghorbani A, Alimohammadian M, Zahedi MJ, Darvish-Moghadam S, et al. The incidence of prostate cancer in Iran: Results of a population-based cancer registry. Archives of Iranian Medicine. 2007; 10(4):481-5. [PMID]
- Gandaglia G, Leni R, Bray F, Fleshner N, Freedland SJ, Kibel A, et al. Epidemiology and prevention of prostate cancer. European Urology Oncology. 2021; 4(6):877-92. [DOI:10.1016/j.euo.2021.09.006] [PMID]
Type of Study: Research |
Subject:
gerontology
Received: 2022/08/13 | Accepted: 2022/11/02 | Published: 2023/10/01
Received: 2022/08/13 | Accepted: 2022/11/02 | Published: 2023/10/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |