Volume 19, Issue 1 (Spring 2024)
Salmand: Iranian Journal of Ageing 2024, 19(1): 54-69 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Vasiee A, Mozafari M, Ghiasi N, Pakzad R, Masoumi M. Effect of Kegel’s Exercises on Urinary Incontinence, Frailty Syndrome, and Self-esteem After TURP: A RCT. Salmand: Iranian Journal of Ageing 2024; 19 (1) :54-69
URL: http://salmandj.uswr.ac.ir/article-1-2633-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2633-en.html
1- Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
2- Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran. ,rezawest10@gmail.com
3- Department of Health Education and Health Promotion, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran.
4- Department of Epidemiology, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran.
5- Department of Urology, Faculty of Medicine, Ilam University of Medical Sciences, Ilam, Iran.
2- Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran. ,
3- Department of Health Education and Health Promotion, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran.
4- Department of Epidemiology, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran.
5- Department of Urology, Faculty of Medicine, Ilam University of Medical Sciences, Ilam, Iran.
Full-Text [PDF 7131 kb]
(1579 Downloads)
| Abstract (HTML) (4726 Views)
Full-Text: (1813 Views)
Introduction
enign prostate hyperplasia (BPH) is common in the elderly, and its treatment options include medical and surgical methods, such as radical prostatectomy (RP) and transurethral resection of the prostate (TURP). The most important complication after prostate surgeries is urinary incontinence (UI), which causes a decrease in self-esteem and an increase in frailty syndrome [14]. One of the treatment methods for UI is Kegel’s exercises, which include voluntary and continuous contractions of the urethral sphincter muscle. According to studies, the Kegel exercises reduce UI after RP [27]. This study aims to investigate the effect of Kegel’s exercises on UI, frailty syndrome, and self-esteem in elderly people with BPH who underwent TURP.
Methods
This randomized clinical trial was conducted on 76 elderly people with BPH who underwent TURP surgery. They were randomly assigned to the control and intervention groups using the permuted block randomization method. Entry criteria were age ≥65 years, at least a primary school education, having a smart cell phone, not being diagnosed with prostate cancer after surgery, a score of 24 or higher in the mini-mental state examination (MMSE), a score of 4 or higher in items 1, 2 and 3 of the questionnaire for urinary incontinence diagnosis (QUID) and a score of 8 or higher in the Edmonton frailty scale (EFS). Exclusion criteria were not doing exercises for more than two days, re-hospitalization during the study, taking medication to control UI, and death. The tools used in this study included EFS, international consultation on incontinence questionnaire – UI short form (ICIQ-UI SF), rosenberg self-esteem scale (RSES), MMSE, QUID, and a demographic form, which were completed before the intervention, eight weeks after the start of the intervention, and four weeks after the end of the intervention. Descriptive statistics (Mean±SD) and inferential statistics (chi-square test, repeated measures ANOVA, Fisher’s test, and LSD post hoc test) were used for data analysis. Data were analyzed using SPSS software, version 26. The significance level was set at 0.05.
Results
The mean age of the participants was 71.78±4.85 years. Most of the participants were young elderly, married, retired, with primary school education, at least one child, a history of smoking, hypertension, diabetes, no history of stroke or heart attack, and less than one hour of mobility during the day. Using chi-square test, there was no significant difference in any demographic variables between the control and intervention groups. The scores of UI, fragility syndrome, and self-esteem in the control and intervention groups were not significantly different before the intervention, while eight weeks after the start of the intervention and four weeks after the end of the intervention, the differences were significant (P<0.05). The mean UI and fragility syndrome scores in the control group increased, indicating the worsening of these conditions, while they decreased in the intervention group, indicating an improvement in these conditions. Moreover, the mean score of self-esteem decreased in the control group, but increased in the intervention group (Table 1).
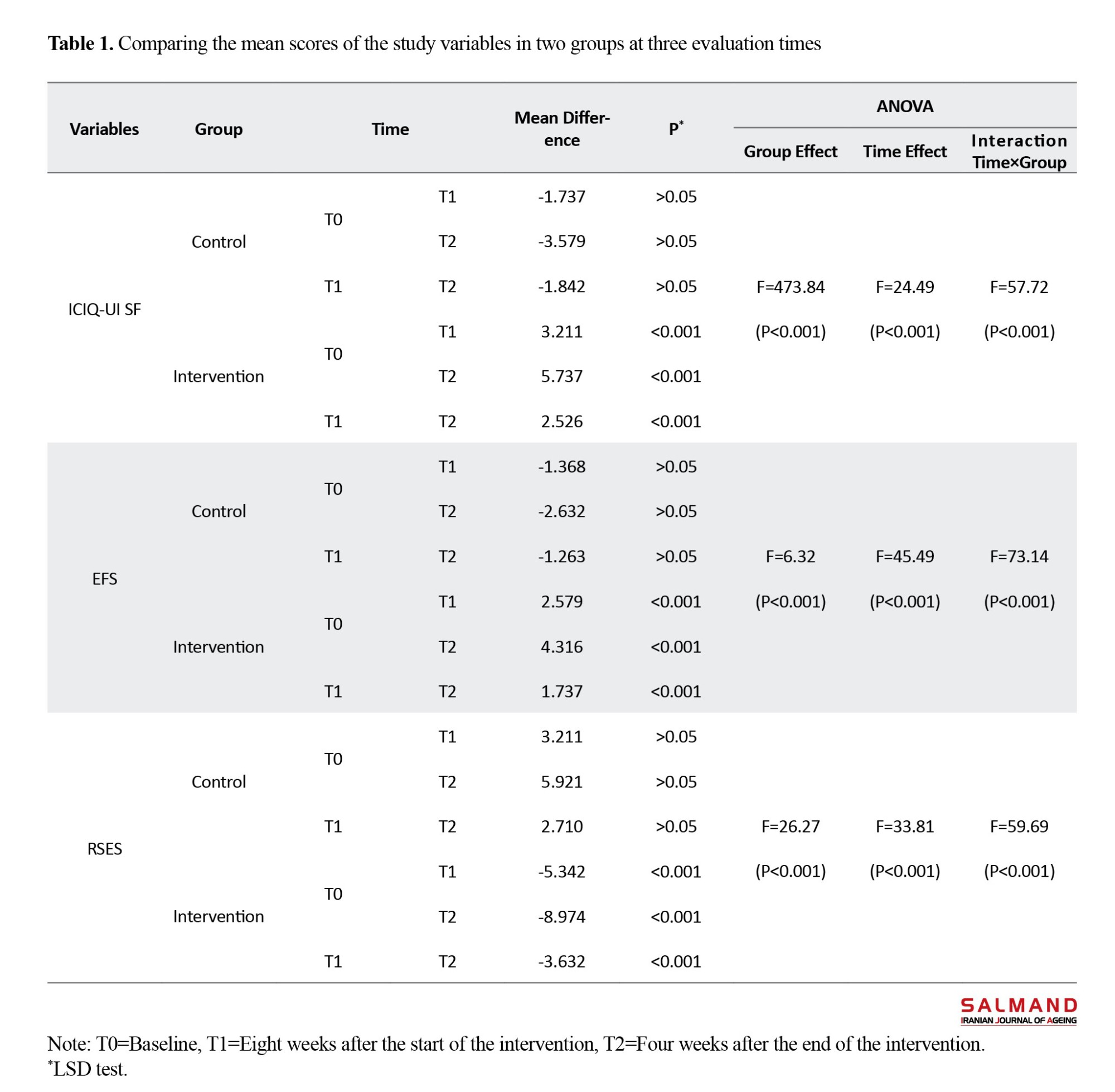
The comparison of the mean scores in each group in three time periods also showed that in the control group, the mean difference in scores of UI and fragility syndrome increased over time, but in the intervention group, the mean difference decreased. The mean difference in the score of self-esteem decreased in the control group over time, but increased in the intervention group. The LSD post hoc test showed that Kegel’s exercises in the intervention group had a significant effect on three variables over time, indicating the persistence of the treatment effect over time (P<0.001). However, there was no statistically significant difference over time in the control group (P>0.05) (Table 1).
Conclusion
The findings of the current study showed that Kegel’s exercises for 3 months improved UI, frailty syndrome, and self-esteem in elderly people with BPH following TURP. However, it was not proved whether the increase or decrease of UI, as a mediating variable, is effective in the relationship between self-esteem and frailty syndrome. Investigating this relationship requires more studies with more samples.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles, such as obtaining informed consent from the participants, protecting their confidentiality, and giving them the right to leave the study, were considered in this research. The present study was approved by the Ethics Committee of Ilam University of Medical Sciences (Code: IR.MEDILAM.REC.1400.167) and was registered by the Iranian Registry of Clinical Trials (IRCT) (ID: IRCT20211110053030N1).
Funding
This article was extracted from a master’s thesis of Alireza Vasiee, approved by Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences.
Authors' contributions
Conceptualization and data curation: Alireza Vasiee and Mosayeb Mozafari; Methodology, formal analysis and visualization: Alireza Vasiee and Reza Pakzad; Validation and resources: Nasrin Ghiasi; Investigation: Alireza Vasiee, Mosayeb Mozafari and Mansour Masoumi; The original draft preparation: Alireza Vasiee and Mansour Masoumi; Review and editing: Mosayeb Mozafari; Supervision: Mosayeb Mozafari, Nasrin Ghiasi and Mansour Masoumi; Project administration: Alireza Vasiee, Mansour Masoumi; Funding acquisition: Ilam University of Medical Sciences.
Conflicts of interest
The authors declared no conflict of interest
Acknowledgements
The authors would like to thank and the seniors and their families, as well as the Clinical Research Unit of Imam Khomeini Hospital in Ilam for their cooperation.
enign prostate hyperplasia (BPH) is common in the elderly, and its treatment options include medical and surgical methods, such as radical prostatectomy (RP) and transurethral resection of the prostate (TURP). The most important complication after prostate surgeries is urinary incontinence (UI), which causes a decrease in self-esteem and an increase in frailty syndrome [14]. One of the treatment methods for UI is Kegel’s exercises, which include voluntary and continuous contractions of the urethral sphincter muscle. According to studies, the Kegel exercises reduce UI after RP [27]. This study aims to investigate the effect of Kegel’s exercises on UI, frailty syndrome, and self-esteem in elderly people with BPH who underwent TURP.
Methods
This randomized clinical trial was conducted on 76 elderly people with BPH who underwent TURP surgery. They were randomly assigned to the control and intervention groups using the permuted block randomization method. Entry criteria were age ≥65 years, at least a primary school education, having a smart cell phone, not being diagnosed with prostate cancer after surgery, a score of 24 or higher in the mini-mental state examination (MMSE), a score of 4 or higher in items 1, 2 and 3 of the questionnaire for urinary incontinence diagnosis (QUID) and a score of 8 or higher in the Edmonton frailty scale (EFS). Exclusion criteria were not doing exercises for more than two days, re-hospitalization during the study, taking medication to control UI, and death. The tools used in this study included EFS, international consultation on incontinence questionnaire – UI short form (ICIQ-UI SF), rosenberg self-esteem scale (RSES), MMSE, QUID, and a demographic form, which were completed before the intervention, eight weeks after the start of the intervention, and four weeks after the end of the intervention. Descriptive statistics (Mean±SD) and inferential statistics (chi-square test, repeated measures ANOVA, Fisher’s test, and LSD post hoc test) were used for data analysis. Data were analyzed using SPSS software, version 26. The significance level was set at 0.05.
Results
The mean age of the participants was 71.78±4.85 years. Most of the participants were young elderly, married, retired, with primary school education, at least one child, a history of smoking, hypertension, diabetes, no history of stroke or heart attack, and less than one hour of mobility during the day. Using chi-square test, there was no significant difference in any demographic variables between the control and intervention groups. The scores of UI, fragility syndrome, and self-esteem in the control and intervention groups were not significantly different before the intervention, while eight weeks after the start of the intervention and four weeks after the end of the intervention, the differences were significant (P<0.05). The mean UI and fragility syndrome scores in the control group increased, indicating the worsening of these conditions, while they decreased in the intervention group, indicating an improvement in these conditions. Moreover, the mean score of self-esteem decreased in the control group, but increased in the intervention group (Table 1).
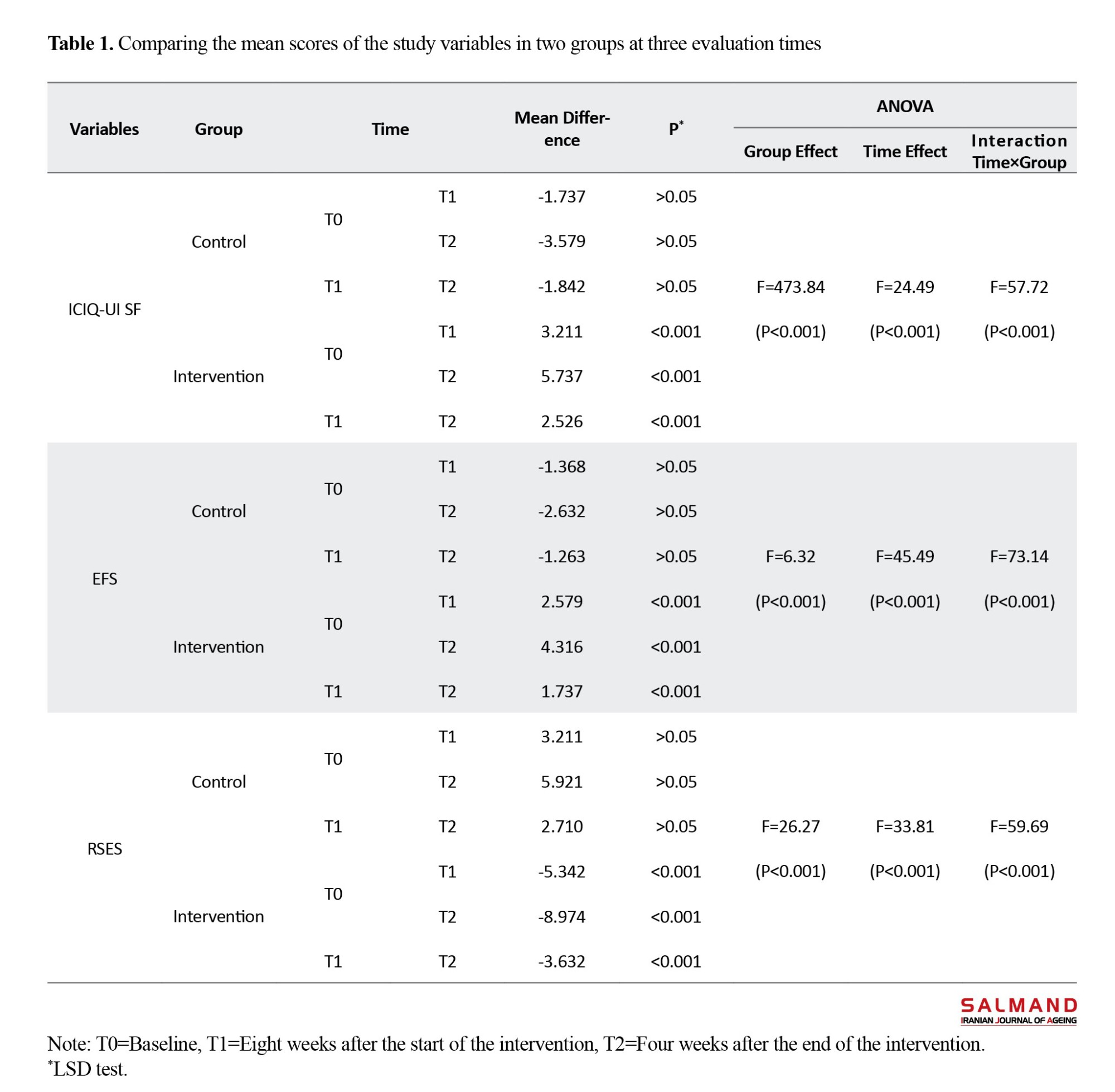
The comparison of the mean scores in each group in three time periods also showed that in the control group, the mean difference in scores of UI and fragility syndrome increased over time, but in the intervention group, the mean difference decreased. The mean difference in the score of self-esteem decreased in the control group over time, but increased in the intervention group. The LSD post hoc test showed that Kegel’s exercises in the intervention group had a significant effect on three variables over time, indicating the persistence of the treatment effect over time (P<0.001). However, there was no statistically significant difference over time in the control group (P>0.05) (Table 1).
Conclusion
The findings of the current study showed that Kegel’s exercises for 3 months improved UI, frailty syndrome, and self-esteem in elderly people with BPH following TURP. However, it was not proved whether the increase or decrease of UI, as a mediating variable, is effective in the relationship between self-esteem and frailty syndrome. Investigating this relationship requires more studies with more samples.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles, such as obtaining informed consent from the participants, protecting their confidentiality, and giving them the right to leave the study, were considered in this research. The present study was approved by the Ethics Committee of Ilam University of Medical Sciences (Code: IR.MEDILAM.REC.1400.167) and was registered by the Iranian Registry of Clinical Trials (IRCT) (ID: IRCT20211110053030N1).
Funding
This article was extracted from a master’s thesis of Alireza Vasiee, approved by Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences.
Authors' contributions
Conceptualization and data curation: Alireza Vasiee and Mosayeb Mozafari; Methodology, formal analysis and visualization: Alireza Vasiee and Reza Pakzad; Validation and resources: Nasrin Ghiasi; Investigation: Alireza Vasiee, Mosayeb Mozafari and Mansour Masoumi; The original draft preparation: Alireza Vasiee and Mansour Masoumi; Review and editing: Mosayeb Mozafari; Supervision: Mosayeb Mozafari, Nasrin Ghiasi and Mansour Masoumi; Project administration: Alireza Vasiee, Mansour Masoumi; Funding acquisition: Ilam University of Medical Sciences.
Conflicts of interest
The authors declared no conflict of interest
Acknowledgements
The authors would like to thank and the seniors and their families, as well as the Clinical Research Unit of Imam Khomeini Hospital in Ilam for their cooperation.
References
- Das K, Buchholz N. Benign prostate hyperplasia and nutrition. Clinical Nutrition ESPEN. 2019; 33:5-11. [DOI:10.1016/j.clnesp.2019.07.015] [PMID]
- Bravi F, Bosetti C, Dal Maso L, Talamini R, Montella M, Negri E, et al. Food groups and risk of benign prostatic hyperplasia. Urology. 2006; 67(1):73-9. [DOI:10.1016/j.urology.2005.07.030] [PMID]
- Safarinejad MR. Prevalence of benign prostatic hyperplasia in a population-based study in Iranian men 40 years old or older. International Urology and Nephrology. 2008; 40(4):921-31. [DOI:10.1007/s11255-008-9338-7] [PMID]
- Mahboub Ahari A, Sadeghi Ghyassi F, Yousefi M, Amjadi M, Mostafaie A. Green light photo selective vaporization of the prostate vs. transurethral resection of prostate for benign prostatic hyperplasia. Journal of Lasers in Medical Sciences. 2011; 2(4):152-8. [Link]
- Amirzargar M, ZerafatJou N, Biglarkhani M. [Comparison of the effect of pumpkin seed oil and tamsulosin on benign prostatic hyperplasia (Persian)]. Journal of Research in Urology. 2020; 4(1):24-32. [DOI:10.30699/jru.4.1.24]
- Becher E, Roehrborn CG, Siami P, Gagnier RP, Wilson TH, Montorsi F. The effects of dutasteride, tamsulosin, and the combination on storage and voiding in men with benign prostatic hyperplasia and prostatic enlargement: 2-year results from the combination of avodart and tamsulosin study. Prostate Cancer and Prostatic Diseases. 2009; 12(4):369-74. [DOI:10.1038/pcan.2009.37] [PMID]
- Pesonen JS, Vernooij RWM, Cartwright R, Aoki Y, Agarwal A, Mangera A, et al. The impact of nocturia on falls and fractures: A systematic review and meta-analysis. The Journal of Urology. 2020; 203(4):674-83. [DOI:10.1097/JU.0000000000000459] [PMID]
- DeAntoni EP, Crawford ED, Oesterling JE, Ross CA, Berger ER, McLeod DG, et al. Age- and race-specific reference ranges for prostate-specific antigen from a large community-based study. Urology. 1996; 48(2):234-9. [DOI:10.1016/S0090-4295(96)00091-X] [PMID]
- Taub DA, Wei JT. The economics of benign prostatic hyperplasia and lower urinary tract symptoms in the United States. Current Urology Reports. 2006; 7(4):272-81. [DOI:10.1007/s11934-996-0006-0] [PMID]
- Msezane LP, Reynolds WS, Gofrit ON, Shalhav AL, Zagaja GP, Zorn KC. Bladder neck contracture after robot-assisted laparoscopic radical prostatectomy: Evaluation of incidence and risk factors and impact on urinary function. Journal of Endourology. 2008; 22(1):97-104. [DOI:10.1089/end.2006.0460]
- Whitty JA, Crosland P, Hewson K, Narula R, Nathan TR, Campbell PA, et al. A cost-minimisation analysis comparing photoselective vaporisation (PVP) and transurethral resection of the prostate (TURP) for the management of symptomatic benign prostatic hyperplasia (BPH) in Queensland, Australia. BJU International. 2014; 113(Suppl 2):21-8. [DOI:10.1111/bju.12051] [PMID]
- Gonzalez-Sanchez B, Cendejas-Gomez J, Alejandro Rivera-Ramirez J, Herrera-Caceres JO, Olvera-Posada D, Villeda-Sandoval CI, et al. The correlation between lower urinary tract symptoms (LUTS) and erectile dysfunction (ED): Results from a survey in males from Mexico City (MexiLUTS). World Journal of Urology. 2016; 34(7):979-83. [DOI:10.1007/s00345-015-1703-4] [PMID]
- Biswas B, Bhattacharyya A, Dasgupta A, Karmakar A, Mallick N, Sembiah S. Urinary incontinence, its risk factors, and quality of life: A study among women aged 50 years and above in a rural health facility of West Bengal. Journal of Mid-Life Health. 2017; 8(3):130-6. [DOI:10.4103/jmh.JMH_62_17] [PMID] [PMCID]
- Lehto US, Tenhola H, Taari K, Aromaa A. Patients' perceptions of the negative effects following different prostate cancer treatments and the impact on psychological well-being: A nationwide survey. British Journal of Cancer. 2017; 116(7):864-73. [DOI:10.1038/bjc.2017.30] [PMID] [PMCID]
- Suskind AM. The aging overactive bladder: A review of aging-related changes from the brain to the bladder. Current Bladder Dysfunction Reports. 2017; 12(1):42-7. [DOI:10.1007/s11884-017-0406-7] [PMID] [PMCID]
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: Evidence for a phenotype. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2001; 56(3):M146-56. [DOI:10.1093/gerona/56.3.M146] [PMID]
- Bauer SR, Jin C, Kamal P, Suskind AM. Association between lower urinary tract symptoms and frailty in older men presenting for urologic care. Urology. 2021; 148:230-4. [DOI:10.1016/j.urology.2020.09.041] [PMID] [PMCID]
- Javadifar N, Komeilifar R, Afshary PD, Haghighy Zadeh MH. [Urinary incontinence and its predisposing factors in reproductive age women (Persian)]. Ilam-University-of-Medical-Sciences. 2018; 25(6):45-53. [DOI:10.29252/sjimu.25.6.45]
- Melotti IGR, Juliato CRT, Tanaka M, Riccetto CLZ. Severe depression and anxiety in women with overactive bladder. Neurourology and Urodynamics. 2018; 37(1):223-8. [DOI:10.1002/nau.23277] [PMID]
- Gibson W, Hunter KF, Camicioli R, Booth J, Skelton DA, Dumoulin C, et al. The association between lower urinary tract symptoms and falls: Forming a theoretical model for a research agenda. Neurourology and Urodynamics. 2018; 37(1):501-9. [DOI:10.1002/nau.23295] [PMID]
- Soliman Y, Meyer R, Baum N. Falls in the elderly secondary to urinary symptoms. Reviews in Urology. 2016; 18(1):28-32. [PMID] [PMCID]
- Lim YM, Lee SR, Choi EJ, Jeong K, Chung HW. Urinary incontinence is strongly associated with depression in middle-aged and older Korean women: Data from the Korean longitudinal study of ageing. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 2018; 220:69-73. [DOI:10.1016/j.ejogrb.2017.11.017] [PMID]
- Suen LKP, Cheng HL, Yeung SKW, Au-Yeung CH, Lee JCY, Ho KKY, et al. Qualitative insights into the experiences of living with moderate-to-severe lower urinary tract symptoms among community-dwelling ageing males. Plos One. 2017; 12(10):e0187085. [DOI:10.1371/journal.pone.0187085] [PMID] [PMCID]
- Elstad EA, Taubenberger SP, Botelho EM, Tennstedt SL. Beyond incontinence: The stigma of other urinary symptoms. Journal of Advanced Nursing. 2010; 66(11):2460-70. [DOI:10.1111/j.1365-2648.2010.05422.x] [PMID] [PMCID]
- MacDonald R, Fink HA, Huckabay C, Monga M, Wilt TJ. Pelvic floor muscle training to improve urinary incontinence after radical prostatectomy: A systematic review of effectiveness. BJU International. 2007; 100(1):76-81. [DOI:10.1111/j.1464-410X.2007.06913.x] [PMID]
- Chughtai B, Lee R, Sandhu J, Te A, Kaplan S. Conservative treatment for postprostatectomy incontinence. Reviews in Urology. 2013; 15(2):61-6. [PMID] [PMCID]
- Milios JE, Ackland TR, Green DJ. Pelvic floor muscle training in radical prostatectomy: A randomized controlled trial of the impacts on pelvic floor muscle function and urinary incontinence. BMC Urology. 2019; 19(1):116. [DOI:10.1186/s12894-019-0546-5] [PMID] [PMCID]
- Kargar Jahromi M, Talebizadeh M, Mirzaei M. The effect of pelvic muscle exercises on urinary incontinency and self-esteem of elderly females with stress urinary incontinency, 2013. Global Journal of Health Science. 2014; 7(2):71-9. [DOI:10.5539/gjhs.v7n2p71] [PMID] [PMCID]
- Hemmati Maslak Pak M, Mollazadeh F, Khalkhali H, Abkhiz S. [The impact of self-care education with teach-back method on self-esteem in kidney transplant recipients. A clinical trial (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2020; 28(3):154-62. [DOI:10.30699/ajnmc.28.3.154]
- Martín-Albo J, Núñiez JL, Navarro JG, Grijalvo F. The rosenberg self-esteem scale: Translation and validation in university students. The Spanish Journal of Psychology. 2007; 10(2):458-67. [DOI:10.1017/S1138741600006727] [PMID]
- Mäkikangas A, Kinnunen U, Feldt T. Self-esteem, dispositional optimism, and health: Evidence from cross-lagged data on employees. Journal of Research in Personality. 2004; 38(6):556-75. [DOI:10.1016/j.jrp.2004.02.001]
- Azizi M, Azadi A, Otaghi M. The effect of a self-care programme on urinary incontinence and self-esteem in elderly men dwelling in nursing homes in Iran. The Aging Male. 2020; 23(5):687-93. [DOI:10.1080/13685538.2019.1573891] [PMID]
- Karmakar D, Mostafa A, Abdel-Fattah M. A new validated score for detecting patient-reported success on postoperative ICIQ-SF: A novel two-stage analysis from two large RCT cohorts. International Urogynecology Journal. 2017; 28(1):95-100. [DOI:10.1007/s00192-016-3070-0] [PMID] [PMCID]
- Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourology and Urodynamics. 2004; 23(4):322-30. [DOI:10.1002/nau.20041] [PMID]
- Hajebrahimi S, Nourizadeh D, Hamedani R, Pezeshki MZ. Validity and reliability of the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form and its correlation with urodynamic findings. Urology Journal. 2012; 9(4):685-90. [PMID]
- Monroe T, Carter M. Using the folstein mini mental state exam (MMSE) to explore methodological issues in cognitive aging research. European Journal of Ageing. 2012; 9(3):265-74. [DOI:10.1007/s10433-012-0234-8] [PMID] [PMCID]
- Anthony JC, LeResche L, Niaz U, von Korff MR, Folstein MF. Limits of the 'mini-mental state' as a screening test for dementia and delirium among hospital patients. Psychological Medicine. 1982; 12(2):397-408. [DOI:10.1017/S0033291700046730] [PMID]
- Blesa R, Pujol M, Aguilar M, Santacruz P, Bertran-Serra I, Hernández G, et al. Clinical validity of the "mini-mental state" for Spanish-speaking communities. Neuropsychologia. 2001; 39(11):1150-7. [DOI:10.1016/S0028-3932(01)00055-0]
- Foroughan M, Jafari Z, Shirin Bayan P, Ghaem Magham Farahani Z, Rahgozar M. [Validation of mini- mental state examination (MMSE) in the elderly population of Tehran (Persian)]. Advances in Cognitive Sciences. 2008; 10(2):29-37. [Link]
- Bradley CS, Rahn DD, Nygaard IE, Barber MD, Nager CW, Kenton KS, et al. The questionnaire for urinary incontinence diagnosis (QUID): Validity and responsiveness to change in women undergoing non-surgical therapies for treatment of stress predominant urinary incontinence. Neurourology and Urodynamics. 2010; 29(5):727-34. [DOI:10.1002/nau.20818] [PMID] [PMCID]
- Ghodsbin F, Kargar M, Jahanbin I, Sagheb MM, Keshavarzi S. The effect of education on quality of life in elderly females with urinary incontinence, refereeing to jahandidegan center in Shiraz-Iran, 2011. Journal of Gerontology & Geriatric Research. 2012; 1(3):1000105. [DOI:10.4172/2167-7182.1000105]
- Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the edmonton frail scale. Age and Ageing. 2006; 35(5):526-9. [DOI:10.1093/ageing/afl041] [PMID] [PMCID]
- Patel MI, Yao J, Hirschhorn AD, Mungovan SF. Preoperative pelvic floor physiotherapy improves continence after radical retropubic prostatectomy. International Journal of Urology. 2013; 20(10):986-92. [DOI:10.1111/iju.12099] [PMID]
- Aydın Sayılan A, Özbaş A. The effect of pelvic floor muscle training on incontinence problems after radical prostatectomy. American Journal of Men's Health. 2018; 12(4):1007-15. [DOI:10.1177/1557988318757242] [PMID] [PMCID]
- Park SW, Kim TN, Nam JK, Ha HK, Shin DG, Lee W, et al. Recovery of overall exercise ability, quality of life, and continence after 12-week combined exercise intervention in elderly patients who underwent radical prostatectomy: A randomized controlled study. Urology. 2012; 80(2):299-305. [DOI:10.1016/j.urology.2011.12.060] [PMID]
- Sheikhalipour Z, Fathiazar E, Lotfi M, Pakpour V, Aghajari P, Ali Mokhtari Z. [Concept of evidence based nursing and nursing education (Persian)]. Iranian Journal of Medical Education. 2014; 14(6):507-16. [Link]
- Nilssen SR, Mørkved S, Overgård M, Lydersen S, Angelsen A. Does physiotherapist-guided pelvic floor muscle training increase the quality of life in patients after radical prostatectomy? A randomized clinical study. Scandinavian Journal of Urology and Nephrology. 2012; 46(6):397-404. [DOI:10.3109/00365599.2012.694117] [PMID]
- Nixon AC, Bampouras TM, Gooch HJ, Young HML, Finlayson KW, Pendleton N, et al. Home-based exercise for people living with frailty and chronic kidney disease: A mixed-methods pilot randomised controlled trial. Plos One. 2021; 16(7):e0251652. [DOI:10.1371/journal.pone.0251652] [PMID] [PMCID]
- Lai X, Bo L, Zhu H, Chen B, Wu Z, Du H, et al. Effects of lower limb resistance exercise on muscle strength, physical fitness, and metabolism in pre-frail elderly patients: A randomized controlled trial. BMC Geriatrics. 2021; 21(1):447. [DOI:10.1186/s12877-021-02386-5] [PMID] [PMCID]
Type of Study: Research |
Subject:
Clinical
Received: 2023/05/26 | Accepted: 2023/07/24 | Published: 2024/04/01
Received: 2023/05/26 | Accepted: 2023/07/24 | Published: 2024/04/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |