Volume 19, Issue 3 (Autumn 2024)
Salmand: Iranian Journal of Ageing 2024, 19(3): 328-361 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hajizadeh A, Albelbeisi A H, Tajvar M. Impacts of Population Ageing on the Functions of the Health System: A Systematic Review. Salmand: Iranian Journal of Ageing 2024; 19 (3) :328-361
URL: http://salmandj.uswr.ac.ir/article-1-2640-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2640-en.html
1- Department of Health Management, Policy and Economics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
2- Medical Services Direction, Gaza Strip, Palestine.
3- Department of Health Management, Policy and Economics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. ,mtajvar@sina.tums.ac.ir
2- Medical Services Direction, Gaza Strip, Palestine.
3- Department of Health Management, Policy and Economics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 29670 kb]
(3354 Downloads)
| Abstract (HTML) (4581 Views)
Full-Text: (2407 Views)
Introduction
The main goal of this study was to review the evidence related to the effect of population ageing on various functions of the health system, including stewardship, financing, resource generation, and service provision.
Methods
This study is a systematic review. The related articles were searched in PubMed, ProQuest, Web of Science, and Google Scholar from 2000 to 2022 using the related keywords. Original and review articles that had examined the effects of population aging on at least one of the functions of the health system were included in this study. Quality evaluation of selected articles was done with strengthening the reporting of observational studies in epidemiology (STROBE) checklist. To analyze the extracted data, the World Health Organization’s (WHO) health system performance assessment framework was used, which includes the four functions of stewardship, financing, resource generation, and service provision. All steps of this systematic review were done independently by two authors and disagreements were resolved with the discussion and participation of the third author. From the 1954 identified articles, 203 were removed due to being duplicates and 1751 remained for screening. After reviewing the title and abstract of the remaining articles, 94 articles were screened by full text. Finally, 23 articles met the entry criteria and selected for the review.
Results
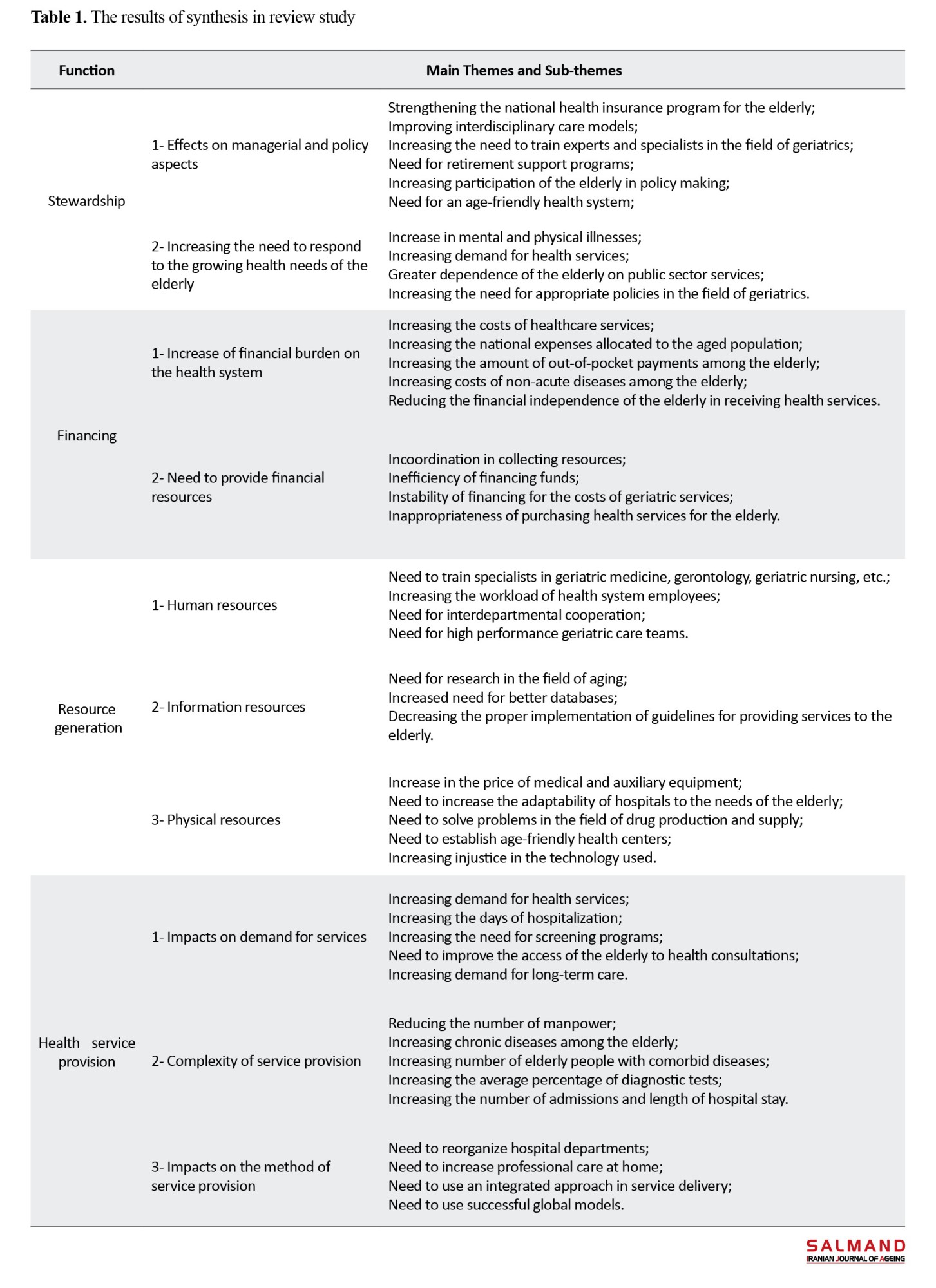
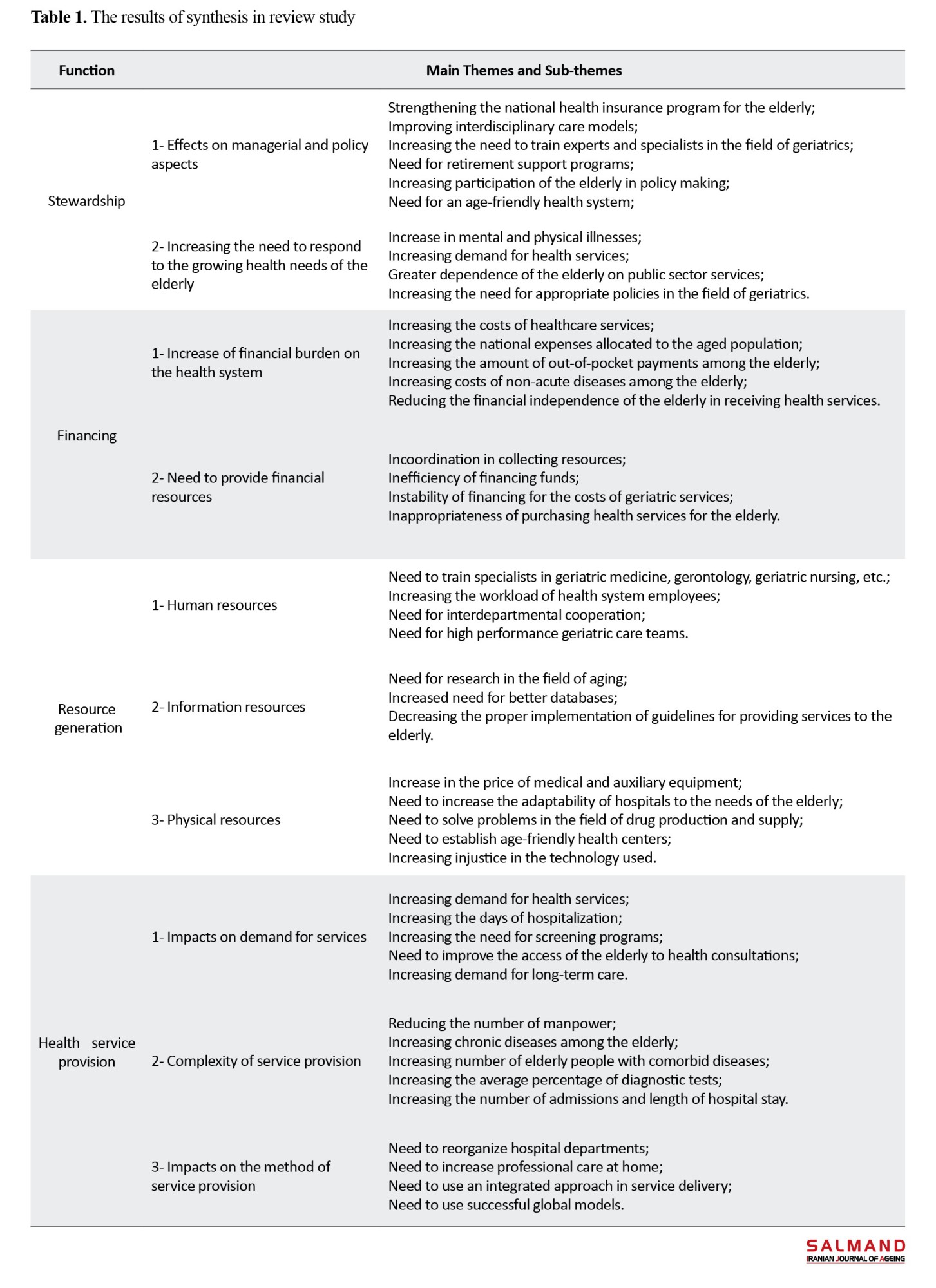
There was a upward growth trend in the studies from 2002 to 2021. Among the selected articles, four articles studied with the effects of population aging on stewardship function of the health system. Most of the studied was related to financing function (n=18). Three articles were related to the function of resource development, and nine articles were related to the function of health service provision. A summary of findings is provided in Table 1.
Conclusion
The effects of population aging on all the functions of the health system, especially the function of financing, are very noticeable. The findings of this study can provide appropriate information to health care providers so that, by proper and timely planning and management, they can improve the performance of the health system in the face of the negative consequences of population aging, which can ultimately improve the health of society and help meet expectations and fair financing in the health system.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.SPH.REC.1401.044).
Funding
This study was extracted from the PhD dissertation of Alireza Hajizadeh, approved by Department of Health Management, Policy and Economics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran (Code: 9921383004).
Authors' contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
References
The main goal of this study was to review the evidence related to the effect of population ageing on various functions of the health system, including stewardship, financing, resource generation, and service provision.
Methods
This study is a systematic review. The related articles were searched in PubMed, ProQuest, Web of Science, and Google Scholar from 2000 to 2022 using the related keywords. Original and review articles that had examined the effects of population aging on at least one of the functions of the health system were included in this study. Quality evaluation of selected articles was done with strengthening the reporting of observational studies in epidemiology (STROBE) checklist. To analyze the extracted data, the World Health Organization’s (WHO) health system performance assessment framework was used, which includes the four functions of stewardship, financing, resource generation, and service provision. All steps of this systematic review were done independently by two authors and disagreements were resolved with the discussion and participation of the third author. From the 1954 identified articles, 203 were removed due to being duplicates and 1751 remained for screening. After reviewing the title and abstract of the remaining articles, 94 articles were screened by full text. Finally, 23 articles met the entry criteria and selected for the review.
Results
There was a upward growth trend in the studies from 2002 to 2021. Among the selected articles, four articles studied with the effects of population aging on stewardship function of the health system. Most of the studied was related to financing function (n=18). Three articles were related to the function of resource development, and nine articles were related to the function of health service provision. A summary of findings is provided in Table 1.
Conclusion
The effects of population aging on all the functions of the health system, especially the function of financing, are very noticeable. The findings of this study can provide appropriate information to health care providers so that, by proper and timely planning and management, they can improve the performance of the health system in the face of the negative consequences of population aging, which can ultimately improve the health of society and help meet expectations and fair financing in the health system.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.SPH.REC.1401.044).
Funding
This study was extracted from the PhD dissertation of Alireza Hajizadeh, approved by Department of Health Management, Policy and Economics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran (Code: 9921383004).
Authors' contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
References
- Nikookar R, Ghaffari S, Akbari Kamrani A A, Sahaf R, Moghadam M, Ghadimi M R. [Assessing the duration of unnecessary hospitalization and expenses in older individuals suffering from cerebral vascular accident in the chronic care unit (Persian)]. Salmand: Iranian Journal of Ageing. 2015; 10(2):180-7. [Link]
- Tajvar M, Yaseri M, Karami B, Mohammadi M. [Pattern of outpatient health service utilization by older people in Iran (Persian)]. Iranian Journal of Ageing. 2021; 15(4):410-27. [DOI:10.32598/sija.15.4.2921.1]
- Zeinalhajlu A, Amini A, Tabrizi J. [Consequences of population aging in Iran with emphasis on its increasing challenges on the health system (literature review) (Persian)]. Depiction of Health. 2015; 6(1):54-64. [Link]
- Soltani MH, Sahaf R, Mohammadi Shahbolaghi F, Ghaffari S, Khosravi A, Gohari MR. [Elderly, duration of hospitalization and Hospital cost in Milad Hospital in Iran (Persian)]. Iranian Journal of Ageing. 2012; 6(S1):58-65. [Link]
- Shoaei F, Nejati V. [Elderly-caring service pattern in USA comparing with Iran (Persian)]. Iranian Journal of Ageing. 2008; 3(1):68-77. [Link]
- Colombier C. Healthcare expenditure and fiscal sustainability: Evidence from Switzerland. Public Sector Economics. 2018; 42(3):279-301. [DOI:10.3326/pse.42.3.3]
- Kalache A, Aboderin I, Hoskins I. Compression of morbidity and active ageing: Key priorities for public health policy in the 21st century. Bulletin of The World Health Organization. 2002; 80:243-4. [Link]
- Nooraiee Motlagh S, Saber Mahani A, Barooni M, Asadi Lari M, Vaez Mahdavi MR, Hadian M. [Determining factors related to health services utilization (Persian)]. Razi Journal of Medical Sciences. 2015; 21(127):61-72. [Link]
- World Health Organization. The world health report 2000: Health systems: Improving performance. Geneva: World Health Organization; 2000. [Link]
- Murray CJ, Frenk J. A framework for assessing the performance of health systems. Bulletin of the world Health Organization. 2000; 78(6):717-31. [PMID]
- Shahri S, Tabibi SJ, Nasiripour AA, Ghaffari F. [Effect functions on goals of health system in Iran (Persian)]. Payavard. 2017; 11(3):247-58. [Link]
- Pakdaman M, Geravandi S, Askari R, Askarishahi M, Afzali HR. The effect of macroeconomic indicators on health-care expenditure in Iran. Journal of Education and Health Promotion. 2019; 8:123. [DOI:10.4103/jehp.jehp_453_18] [PMID] [PMCID]
- Nasrollahpour Shirvani S, Moudi S. [Evidence-based policy-making in the health system and its achievements and challenges of publishing in Iran (Persian)]. Babol: Babol University of Medical Sciences and Health Services; 2013. [Link]
- Sapelli C. Chile: Effects of old age on health services utilization and consequences on system design. Documentos de Trabajo 255, Instituto de Economia. Pontificia Universidad Católica de Chile. 2003. [Link]
- Lin MH, Chou MY, Liang CK, Peng LN, Chen LK. Population aging and its impacts: Strategies of the health-care system in Taipei. Ageing Research Reviews. 2010; 9(Suppl 1):S23-7. [DOI:10.1016/j.arr.2010.07.004] [PMID]
- Lopreite M, Mauro M. The effects of population ageing on health care expenditure: A Bayesian VAR analysis using data from Italy. Health Policy. 2017; 121(6):663-74. [DOI:10.1016/j.healthpol.2017.03.015] [PMID]
- Shakoor U, Rashid M, Baloch AA, Husnain MIu, Saboor A. How aging population affects health care expenditures in Pakistan? A bayesian VAR analysis. Social Indicators Research. 2021; 153:585-607. [DOI:10.1007/s11205-020-02500-x]
- Seshamani M, Gray A. The impact of ageing on expenditures in the National Health Service. Age and Ageing. 2002; 31(4):287-94. [DOI:10.1093/ageing/31.4.287] [PMID]
- Martini EM, Garrett N, Lindquist T, Isham GJ. The boomers are coming: A total cost of care model of the impact of population aging on health care costs in the United States by Major Practice Category. Health Services Research. 2007; 42(1 Pt 1):201-18. [DOI:10.1111/j.1475-6773.2006.00607.x] [PMID] [PMCID]
- Gregersen FA. The impact of ageing on health care expenditures: A study of steepening. The European Journal of Health Economics: HEPAC: Health Economics In Prevention and Care. 2014; 15(9):979-89. [DOI:10.1007/s10198-013-0541-9] [PMID] [PMCID]
- Sarker AR, Mahumud RA, Sultana M, Ahmed S, Ahmed W, Khan JAM. The impact of age and sex on healthcare expenditure of households in Bangladesh. SpringerPlus. 2014; 3:435.[DOI:10.1186/2193-1801-3-435] [PMID] [PMCID]
- Kocot E. The impact of aging on different types of health care: The example of the Polish health insurance system. The International Journal of Health Planning and Management. 2018; 33(2):e557-68. [DOI:10.1002/hpm.2498] [PMID]
- Wang C, Li F, Wang L, Zhou W, Zhu B, Zhang X, et al. The impact of population aging on medical expenses: A big data study based on the life table. Bioscience Trends. 2018; 11(6):619-31. [DOI:10.5582/bst.2017.01243] [PMID]
- Agustin K, Shou-Yan C. Impact of an ageing society on healthcare expenditure of national health insurance in Taiwan. Jurnal Teknik Industri. 2019; 21(2):49-56. [DOI:10.9744/jti.21.2.49-56]
- Daviaud E, Kelly G, Cornell J, Geffen L, Solanki G. Population ageing in South Africa: Trends, impact, and challenges for the health sector. South African Health Review. 2019; 2019(1):175-82. [Link]
- Li L, Du T, Hu Y. The effect of population aging on healthcare expenditure from a healthcare demand perspective among different age groups: Evidence from Beijing City in the People's Republic of China. Risk Management and Healthcare Policy. 2020; 13:1403-12. [DOI:10.2147/RMHP.S271289] [PMID] [PMCID]
- Tang B, Li Z. A country-level empirical study on the fiscal effect of elderly population health: The mediating role of healthcare resources. Healthcare (Basel, Switzerland). 2021; 10(1):30. [DOI:10.3390/healthcare10010030] [PMID] [PMCID]
- Lorenz N, Ihle P, Breyer F. Aging and health care expenditures: A non-parametric approach. CESifo Working Paper No. 8216. 2020. [DOI:10.2139/ssrn.3576293]
- Bech M, Christiansen T, Khoman E, Lauridsen J, Weale M. Ageing and health care expenditure in EU-15. The European Journal of Health Economics. 2011; 12(5):469-78. [DOI:10.1007/s10198-010-0260-4] [PMID]
- Meng X, Yeo C. Ageing and health-care expenditure in urban China. Canberra: Australian National University; 2005. [Link]
- Costa-Font J, Vilaplana-Prieto C. 'More than one red herring'? Heterogeneous effects of ageing on health care utilisation. Health Economics. 2020; 29(Suppl 1):8-29. [DOI:10.1002/hec.4035] [PMID]
- Holecki T, Rogalska A, Sobczyk K, Wozniak-Holecka J, Romaniuk P. Global elderly migrations and their impact on health care systems. Frontiers in Public Health. 2020; 8:386. [DOI:10.3389/fpubh.2020.00386] [PMID] [PMCID]
- Atella V, Piano Mortari A, Kopinska J, Belotti F, Lapi F, Cricelli C, et al. Trends in age-related disease burden and healthcare utilization. Aging Cell. 2019; 18(1):e12861. [DOI:10.1111/acel.12861] [PMID] [PMCID]
- Dall TM, Gallo PD, Chakrabarti R, West T, Semilla AP, Storm MV. An aging population and growing disease burden will require alarge and specialized health care workforce by 2025. Health Affairs. 2013; 32(11):2013-20. [DOI:10.1377/hlthaff.2013.0714] [PMID]
- Schulz E, Leidl R, König HH. The impact of ageing on hospital care and long-term care-the example of Germany. Health Policy. 2004; 67(1):57-74. [DOI:10.1016/S0168-8510(03)00083-6] [PMID]
- Hajizadeh A, Babaei Aghbolagh M, Babaei G, Tajvar M, Heydari M. Strategies to enhance access and utilization of health services by older population: A comprehensive scoping review. Health & Social Care in the Community. 2024; 2024(1):3645115. [DOI:10.1155/2024/3645115]
- Karami B, Ostad-Taghizadeh A, Rashidian A, Tajvar M. Developing a conceptual framework for an age-friendly health system: A scoping review. International Journal of Health Policy and Management. 2023; 12:7342. [DOI:10.34172/ijhpm.2023.7342] [PMID] [PMCID]
- Tajvar M, Mosadeghrad A, Yaseri M, Mohammadi M. [Utilization of inpatient services by older people in Iran and its determinants (Persian)]. Journal of School of Public Health and Institute of Public Health Research. 2020; 17(4):337-50. [Link]
- Ghaemi Asl M, Mirzaei Abbasabadi H. Age effects on health expenditures: a global view. Journal of Population Ageing. 2021; 14(2):247-70. [Link]
Type of Study: Review paper |
Subject:
gerontology
Received: 2023/06/07 | Accepted: 2023/12/24 | Published: 2024/10/01
Received: 2023/06/07 | Accepted: 2023/12/24 | Published: 2024/10/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |