Volume 19, Issue 3 (Autumn 2024)
Salmand: Iranian Journal of Ageing 2024, 19(3): 470-483 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Salehi N, Abasi F, Mahmoudi Bavandpouri S, Motevaseli S. Predictors of One-year Mortality in Older Patients With Myocardial Infarction: Results of a Cohort Study. Salmand: Iranian Journal of Ageing 2024; 19 (3) :470-483
URL: http://salmandj.uswr.ac.ir/article-1-2718-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2718-en.html
1- Cardiovascular Research Center, Health Research Institute, Imam Ali Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran.
2- Deputy of Research and Technology, Kermanshah University of Medical Sciences, Kermanshah, Iran.
3- Student Research Committee, Kermanshah University of Medical Sciences Kermanshah Iran. ,sayemotevaseli@gmail.com
2- Deputy of Research and Technology, Kermanshah University of Medical Sciences, Kermanshah, Iran.
3- Student Research Committee, Kermanshah University of Medical Sciences Kermanshah Iran. ,
Full-Text [PDF 5266 kb]
(1168 Downloads)
| Abstract (HTML) (2977 Views)
Full-Text: (1583 Views)
Introduction
Due to the improvement of health systems and increase in life expectancy, the population of older people is increasing [1]. These changes lead to an increase in the burden of cardiovascular diseases and their related costs [4]. In high-income countries, the burden of heart diseases has decreased mainly due to health improvements, while in low-income countries this burden has remained high [12]. ST-segment elevation myocardial infarction (STEMI) is a common and serious type of myocardial infarction with high morbidity and mortality [7]. There is little information about the management and risk factors of STEMI affecting the long-term mortality of older people in low- and middle-income countries [14]. The aim of this study is to evaluate the risk factors, clinical characteristics, and treatment patterns of STEMI and to examine the predictors of one-year mortality in older patients with STEMI in western Iran.
Methods
This retrospective cohort study was conducted on 421 older people (≥65 years) with STEMI admitted to Imam Ali Hospital in Kermanshah, Iran, from July 3, 2018, to December 21, 2019. After admission, patients’ contact information was recorded. Trained doctors and nurses collected the demographic and clinical information of the patients through standard questionnaires and medical records. The variables examined in this study included age, gender, body mass index (BMI), level of education, place of residence, low-density lipoprotein (LDL), high-density lipoprotein (HDL), glomerular filtration rate (GFR), diabetes, blood pressure, chronic kidney disease, history of smoking, history of coronary interventions, history of cardiovascular events, type of heart attack, type of treatment (PCI, thrombolytic treatment and no treatment) and left ventricular ejection fraction (LVEF). The primary outcome of the study was 1-year mortality after STEMI.
Patients were followed up for one year. Trained nurses called the patient’s family or companions and invited the patient for re-examination. In case of death, the date is recorded based on the death certificate or the statements of the family of the deceased patients. Survival time was considered from the date of admission to death, and if the patient survived 365 days after admission. To describe continuous variables with normal distribution, Mean±SD was used. For abnormal cases, median and interquartile range (IQR) were used. The classified variables were expressed by frequency and percentage. To identify predictors of one-year mortality, Cox proportional-hazards model was used in univariate and multivariate form. Variables with a significance level <0.2 were added to the multivariate model. Data analysis was done in Stata software, version 12.
Results
Participants were 421 older people with STEMI. The follow-up period was 350.62 person-years. In the one-year follow-up, it was not possible to contact 9 people (missing rate: 2.1%). The one-year mortality rate was (n=76[18.5%]), of which 9.3% patients (n=39) died in the hospital. The majority of patients were male (67.5%) and residents of Kermanshah City (74.9%). The mean age of patients was 73.51±6.73 years; (n=264[62.7%]) had a history of hypertension, (n=230[54.9%]) had chronic kidney disease, (n=103[24%]) had a history of diabetes, and (n=103[24.5%]) had a history of smoking. In terms of education, 239(60.8%) were illiterate, 136(34.6%) had elementary school up to high school education, and 18 (4.6%) had a high school diploma or higher. The LVEF for 130 patients (35%) was <35%, 35-50% for 55% of patients, and >50% for 50% of patients. Overall, 212 patients (50.4%) had received PCI, 128(30.4%) thrombolytic treatment, and 81(19.2%) did not receive reperfusion. Of 76 patients (18.5%) who died, 12.4% had undergone PCI, 16.1% had thrombolytic treatment and 0.38% had not received any reperfusion treatment.
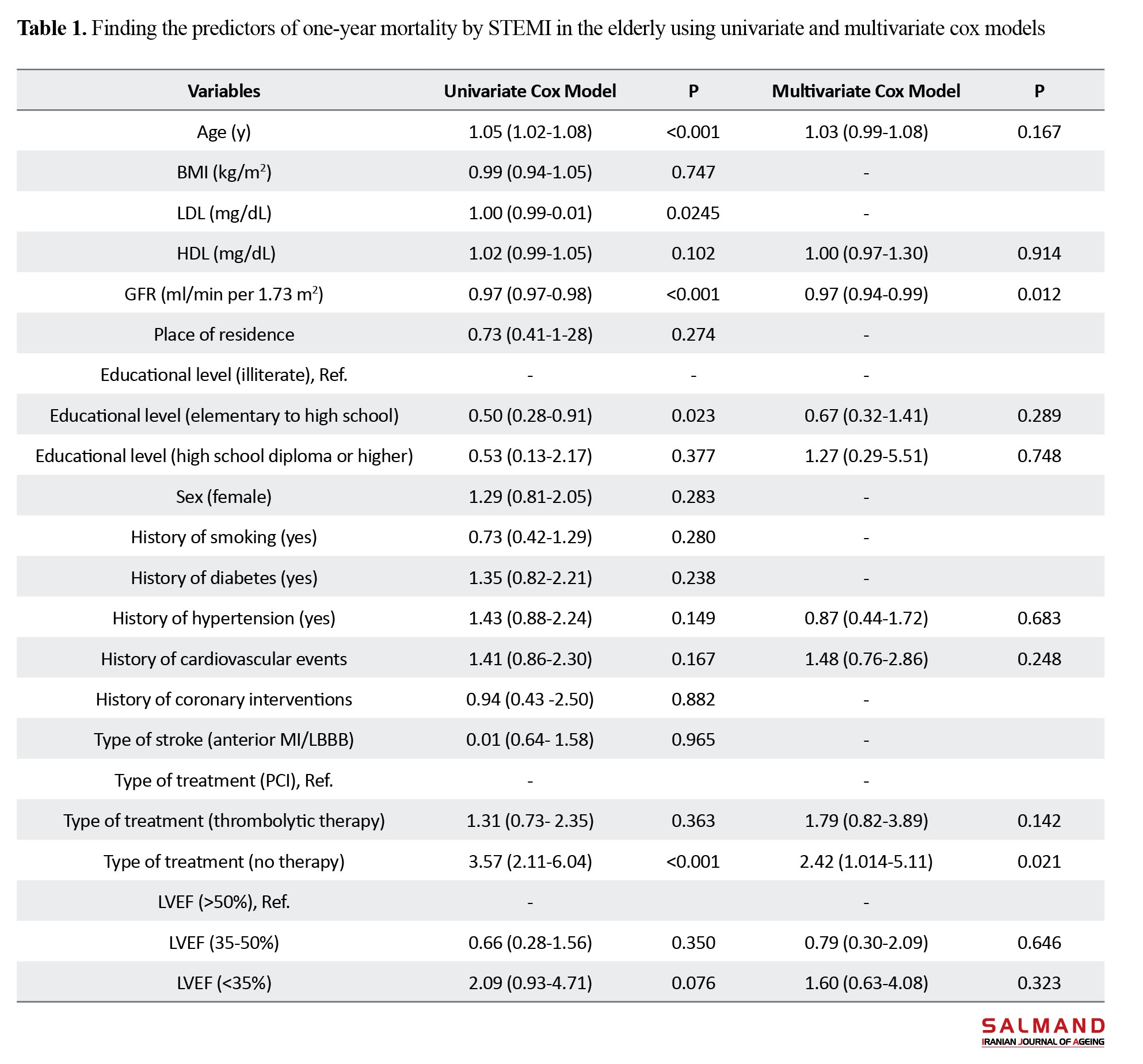
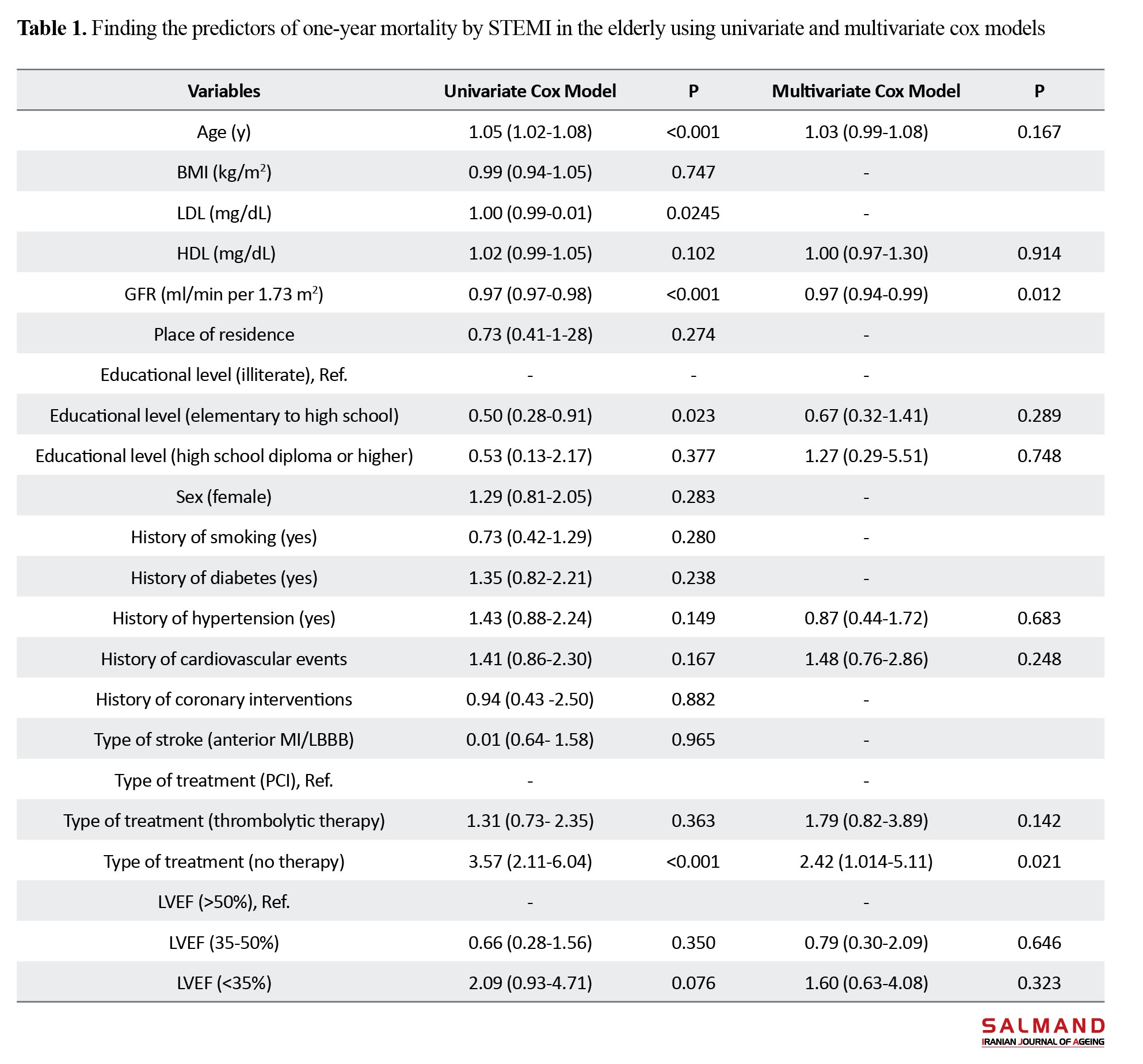
Based on the results of univariate Cox proportional-hazards model, lack of reperfusion treatment was one of the risk factors for one-year mortality in the elderly with STEMI (P<0.05). For every one year increase in the age, the risk of one-year mortality by STEMI increased by 1.05 times. Higher GFR and educational level were protective factors for death in the elderly. The results of multivariate Cox model showed that higher GFR and lack of reperfusion treatment had a statistically significant relationship with one-year mortality (P<0.05). For every one unit increase in GFR, the one-year mortality rate decreased by 3%. Also, the one-year mortality rate of the elderly who received reperfusion treatment decreased by 51% (P<0.05) (Table 1).
Conclusion
In this study, the majority of older patients with STEMI had been treated with PCI, and their one-year mortality rate was lower than those who received thrombolytic therapy. Older age, decreased GFR, lower literacy level, and lack of reperfusion therapy were associated with an increased risk of one-year mortality in the patients. Creating a management and treatment network for STEMI patients and planning to improve the health literacy of these patients through educational interventions about the symptoms of STEMI and the importance of timely treatment can be very effective in improving clinical outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Kermanshah University of Medical Sciences (Code: KUMS.REC.1395.252).
Funding
This study was funded by Kermanshah University of Medical Sciences (Grant No.: 1395.252).
Authors' contributions
The authors contributed equally to preparing this article.
Conflicts of interest
The authors declare no conflict of interest
Acknowledgements
The authors would like to thank all participants, the personnel of Imam Ali Hospital in Kermanshah, and the Vice-Chancellor for Research of Kermanshah University of Medical Sciences for their cooperation and support in this study.
References
Due to the improvement of health systems and increase in life expectancy, the population of older people is increasing [1]. These changes lead to an increase in the burden of cardiovascular diseases and their related costs [4]. In high-income countries, the burden of heart diseases has decreased mainly due to health improvements, while in low-income countries this burden has remained high [12]. ST-segment elevation myocardial infarction (STEMI) is a common and serious type of myocardial infarction with high morbidity and mortality [7]. There is little information about the management and risk factors of STEMI affecting the long-term mortality of older people in low- and middle-income countries [14]. The aim of this study is to evaluate the risk factors, clinical characteristics, and treatment patterns of STEMI and to examine the predictors of one-year mortality in older patients with STEMI in western Iran.
Methods
This retrospective cohort study was conducted on 421 older people (≥65 years) with STEMI admitted to Imam Ali Hospital in Kermanshah, Iran, from July 3, 2018, to December 21, 2019. After admission, patients’ contact information was recorded. Trained doctors and nurses collected the demographic and clinical information of the patients through standard questionnaires and medical records. The variables examined in this study included age, gender, body mass index (BMI), level of education, place of residence, low-density lipoprotein (LDL), high-density lipoprotein (HDL), glomerular filtration rate (GFR), diabetes, blood pressure, chronic kidney disease, history of smoking, history of coronary interventions, history of cardiovascular events, type of heart attack, type of treatment (PCI, thrombolytic treatment and no treatment) and left ventricular ejection fraction (LVEF). The primary outcome of the study was 1-year mortality after STEMI.
Patients were followed up for one year. Trained nurses called the patient’s family or companions and invited the patient for re-examination. In case of death, the date is recorded based on the death certificate or the statements of the family of the deceased patients. Survival time was considered from the date of admission to death, and if the patient survived 365 days after admission. To describe continuous variables with normal distribution, Mean±SD was used. For abnormal cases, median and interquartile range (IQR) were used. The classified variables were expressed by frequency and percentage. To identify predictors of one-year mortality, Cox proportional-hazards model was used in univariate and multivariate form. Variables with a significance level <0.2 were added to the multivariate model. Data analysis was done in Stata software, version 12.
Results
Participants were 421 older people with STEMI. The follow-up period was 350.62 person-years. In the one-year follow-up, it was not possible to contact 9 people (missing rate: 2.1%). The one-year mortality rate was (n=76[18.5%]), of which 9.3% patients (n=39) died in the hospital. The majority of patients were male (67.5%) and residents of Kermanshah City (74.9%). The mean age of patients was 73.51±6.73 years; (n=264[62.7%]) had a history of hypertension, (n=230[54.9%]) had chronic kidney disease, (n=103[24%]) had a history of diabetes, and (n=103[24.5%]) had a history of smoking. In terms of education, 239(60.8%) were illiterate, 136(34.6%) had elementary school up to high school education, and 18 (4.6%) had a high school diploma or higher. The LVEF for 130 patients (35%) was <35%, 35-50% for 55% of patients, and >50% for 50% of patients. Overall, 212 patients (50.4%) had received PCI, 128(30.4%) thrombolytic treatment, and 81(19.2%) did not receive reperfusion. Of 76 patients (18.5%) who died, 12.4% had undergone PCI, 16.1% had thrombolytic treatment and 0.38% had not received any reperfusion treatment.
Based on the results of univariate Cox proportional-hazards model, lack of reperfusion treatment was one of the risk factors for one-year mortality in the elderly with STEMI (P<0.05). For every one year increase in the age, the risk of one-year mortality by STEMI increased by 1.05 times. Higher GFR and educational level were protective factors for death in the elderly. The results of multivariate Cox model showed that higher GFR and lack of reperfusion treatment had a statistically significant relationship with one-year mortality (P<0.05). For every one unit increase in GFR, the one-year mortality rate decreased by 3%. Also, the one-year mortality rate of the elderly who received reperfusion treatment decreased by 51% (P<0.05) (Table 1).
Conclusion
In this study, the majority of older patients with STEMI had been treated with PCI, and their one-year mortality rate was lower than those who received thrombolytic therapy. Older age, decreased GFR, lower literacy level, and lack of reperfusion therapy were associated with an increased risk of one-year mortality in the patients. Creating a management and treatment network for STEMI patients and planning to improve the health literacy of these patients through educational interventions about the symptoms of STEMI and the importance of timely treatment can be very effective in improving clinical outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Kermanshah University of Medical Sciences (Code: KUMS.REC.1395.252).
Funding
This study was funded by Kermanshah University of Medical Sciences (Grant No.: 1395.252).
Authors' contributions
The authors contributed equally to preparing this article.
Conflicts of interest
The authors declare no conflict of interest
Acknowledgements
The authors would like to thank all participants, the personnel of Imam Ali Hospital in Kermanshah, and the Vice-Chancellor for Research of Kermanshah University of Medical Sciences for their cooperation and support in this study.
References
- Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020; 139:6-11. [DOI:10.1016/j.maturitas.2020.05.018] [PMID] [PMCID]
- United Nations. World social report 2023: Leaving no one behind in an ageing world. New York: United Nations; 2023. [Link]
- Bahador F, Mahfoozpour S, Masoudiasl I, Vahdat S. [A systematic review of the management of preventive health care for the elderly in the world (Persian)]. Salmand: Iranian Journal of Ageing. 2022; 16(4):592-607. [DOI:10.32598/sija.2021.3180.2]
- Carro A, Kaski JC. Myocardial infarction in the elderly. Aging and Disease. 2011; 2(2):116-37. [PMID]
- Heart Disease. Prevention CfDCa. About heart disease [Internet]. 2023 [Updated 18 July 2023]. Available ftom: [Link]
- Salari N, Morddarvanjoghi F, Abdolmaleki A, Rasoulpoor S, Khaleghi AA, Hezarkhani LA, et al. The global prevalence of myocardial infarction: A systematic review and meta-analysis. BMC Cardiovascular Disorders. 2023; 23(1):206. [DOI:10.1186/s12872-023-03231-w] [PMID] [PMCID]
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal. 2018; 39(2):119-77. [DOI:10.1093/eurheartj/ehx393] [PMID]
- Kala P, Kanovsky J, Rokyta R, Smid M, Pospisil J, Knot J, et al. Age-related treatment strategy and long-term outcome in acute myocardial infarction patients in the PCI era. BMC Cardiovascular Disorders. 2012; 12:31. [DOI:10.1186/1471-2261-12-31] [PMID] [PMCID]
- Beza L, Leslie SL, Alemayehu B, Gary R. Acute coronary syndrome treatment delay in low to middle-income countries: A systematic review. International Journal of Cardiology. Heart & vasculature. 2021; 35:100823. [PMID]
- Haller PM, Jäger B, Farhan S, Christ G, Schreiber W, Weidinger F, et al. Impact of age on short-and long-term mortality of patients with ST-elevation myocardial infarction in the VIENNA STEMI network. Wiener klinische Wochenschrift. 2018; 130(5-6):172-81.[DOI:10.1007/s00508-017-1250-7] [PMID]
- Forman DE, Chen AY, Wiviott SD, Wang TY, Magid DJ, Alexander KP. Comparison of outcomes in patients aged< 75, 75 to 84, and≥ 85 years with ST-elevation myocardial infarction (from the ACTION Registry-GWTG). The American Journal of Cardiology. 2010; 106(10):1382-8. [DOI:10.1016/j.amjcard.2010.07.008] [PMID]
- Dong C, Bu X, Liu J, Wei L, Ma A, Wang T. Cardiovascular disease burden attributable to dietary risk factors from 1990 to 2019: A systematic analysis of the Global Burden of Disease study. Nutrition, Metabolism & Cardiovascular Diseases. 2022; 32(4):897-907. [DOI:10.1016/j.numecd.2021.11.012] [PMID]
- Chandrashekhar Y, Alexander T, Mullasari A, Kumbhani DJ, Alam S, Alexanderson E, et al. Resource and infrastructure-appropriate management of ST-segment elevation myocardial infarction in low-and middle-income countries. Circulation. 2020; 141(24):2004-25. [DOI:10.1161/CIRCULATIONAHA.119.041297] [PMID]
- Kazemi MK, Alimohammadzadeh K, Maher A. Short-and long-term follow-up in the elderly patients with ST-elevation myocardial infarction receiving primary angioplasty or thrombolytic therapy. International Journal of Cardiovascular Practice. 2019; 4(1):10-5. [DOI:10.21859/ijcp-403]
- World Bank. GDP per capita (constant 2015 US$). World Bank Open Data. Washington: World Bank; 2023. [Link]
- Financial Tribune. 8 Provinces filed double-digit unemployment in FY 2022-23 [Internet]. 2023. [Updated 21 November 2023]. Available from: [Link]
- Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, et al. Socioeconomic status and cardiovascular outcomes: Challenges and interventions. Circulation. 2018; 137(20):2166-78. [DOI:10.1161/CIRCULATIONAHA.117.029652] [PMID] [PMCID]
- Davari M, Maracy MR, Khorasani E. Socioeconomic status, cardiac risk factors, and cardiovascular disease: A novel approach to determination of this association. ARYA atherosclerosis. 2019; 15(6):260-6. [PMID]
- Wang JY, Wang CY, Juang SY, Huang KY, Chou P, Chen CW, et al. Low socioeconomic status increases short-term mortality of acute myocardial infarction despite universal health coverage. International Journal of Cardiology. 2014; 172(1):82-7. [DOI:10.1016/j.ijcard.2013.12.082] [PMID]
- Statistical Centre of Iran. [Estimation of population in Iran by province and year (Persian)]. Tehran: Statistical Centre of Iran; 2016. [Link]
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018; 138(20):e618-51. [DOI:10.1161/CIR.0000000000000617] [PMID]
- Janjani P, Motevaseli S, Salimi Y, Bavandpouri SM, Ziapour A, Salehi N, et al. Clinical and epidemiological profile of ST‐segment elevation myocardial infarction patients in a megacity of west of Iran. Health Science Reports. 2023; 6(5):e1187. [DOI:10.1002/hsr2.1187] [PMID] [PMCID]
- Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Annals of Internal Medicine. 2009; 150(9):604-12. [DOI:10.7326/0003-4819-150-9-200905050-00006] [PMID] [PMCID]
- Wang Y, Wang W, Jia S, Gao M, Zheng S, Wang J, et al. Development of a nomogram for the prediction of in-hospital mortality in patients with acute ST-elevation myocardial infarction after primary percutaneous coronary intervention: A multicentre, retrospective, observational study in Hebei province, China. BMJ Open. 2022; 12(2):e056101. [DOI:10.1136/bmjopen-2021-056101] [PMID] [PMCID]
- De Luca G, van 't Hof AW, Ottervanger JP, Hoorntje JC, Gosselink AT, Dambrink JH, et al. Ageing, impaired myocardial perfusion, and mortality in patients with ST-segment elevation myocardial infarction treated by primary angioplasty. European Heart Journal. 2005; 26(7):662-6. [DOI:10.1093/eurheartj/ehi110] [PMID]
- de Boer MJ, Ottervanger JP, Van't Hof AWJ, Hoorntje JCA, Suryapranata H, Zijlstra F; et al. Final benefit of primary percutaneous coronary intervention for ST-elevation myocardial infarction in older patients: long-term results of a randomised trial. Netherlands Heart Journal. 2022; 30(12):567-71. [DOI:10.1007/s12471-022-01724-5] [PMID] [PMCID]
- Raja DC, Subban V, Victor SM, Joseph G, Thomson VS, Kannan K, et al. The impact of systems-of-care on pharmacoinvasive management with streptokinase: The subgroup analysis of the TN-STEMI programme. Indian Heart Journal. 2017; 69(5):573-9. [DOI:10.1016/j.ihj.2017.07.006] [PMID] [PMCID]
- Grams ME, Chow EK, Segev DL, Coresh J. Lifetime incidence of CKD stages 3-5 in the United States. American Journal of Kidney Diseases. 2013; 62(2):245-52. [DOI:10.1053/j.ajkd.2013.03.009] [PMID] [PMCID]
- Hoogeveen EK, Geleijnse JM, Kromhout D, Stijnen T, Gemen EF, Kusters R, et al. Effect of omega-3 fatty acids on kidney function after myocardial infarction: The Alpha Omega Trial. Clinical Journal of the American Society of Nephrology. 2014; 9(10):1676-83. [DOI:10.2215/CJN.10441013] [PMID] [PMCID]
- Rathod KS, Jones DA, Gallagher S, Rathod VS, Weerackody R, Jain AK, et al. Atypical risk factor profile and excellent long-term outcomes of young patients treated with primary percutaneous coronary intervention for ST-elevation myocardial infarction. European Heart Journal. Acute Cardiovascular Care. 2016; 5(1):23-32. [DOI:10.1177/2048872614567453] [PMID]
- Hoogeveen EK, Geleijnse JM, Giltay EJ, Soedamah-Muthu SS, de Goede J, Oude Griep LM, et al. Kidney function and specific mortality in 60-80 years old post-myocardial infarction patients: A 10-year follow-up study. Plos One. 2017; 12(2):e0171868. [DOI:10.1371/journal.pone.0171868] [PMID] [PMCID]
- Kochar A, Chen AY, Sharma PP, Pagidipati NJ, Fonarow GC, Cowper PA, et al. Long‐term mortality of older patients with acute myocardial infarction treated in US clinical practice. Journal of the American Heart Association. 2018; 7(13):e007230. [DOI:10.1161/JAHA.117.007230] [PMID] [PMCID]
- Kim JH, Jeong MH, Park IH, Choi JS, Rhee JA, Lee DH, et al. The association of socioeconomic status with three-year clinical outcomes in patients with acute myocardial infarction who underwent percutaneous coronary intervention. Journal of Korean Medical Science. 2014; 29(4):536-43. [DOI:10.3346/jkms.2014.29.4.536] [PMID] [PMCID]
- Poorhosseini H, Saadat M, Salarifar M, Mortazavi SH, Geraiely B. Pre-hospital delay and its contributing factors in patients with ST-elevation myocardial infarction; a cross sectional study. Archives of Academic Emergency Medicine. 2019; 7(1):e29. [PMID]
Type of Study: Research |
Subject:
Geriatric
Received: 2023/10/16 | Accepted: 2023/12/24 | Published: 2024/10/01
Received: 2023/10/16 | Accepted: 2023/12/24 | Published: 2024/10/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |