Volume 19, Issue 4 (Winter 2025)
Salmand: Iranian Journal of Ageing 2025, 19(4): 642-663 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hamedanchi A, Rezaie F, Nafei A, Hamzezadeh H. Causes and Trends of Mortality Among Iranian Older Adults From 2000 to 2019. Salmand: Iranian Journal of Ageing 2025; 19 (4) :642-663
URL: http://salmandj.uswr.ac.ir/article-1-2737-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2737-en.html
1- Research Department of Gerontology, Academic Center for Education, Culture and Research (ACECR), Shahid Beheshti University of Medical Sciences Branch, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Research Department of Gerontology, Academic Center for Education, Culture and Research (ACECR), Shahid Beheshti University of Medical Sciences Branch, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,fereshte.rezaie318@gmail.com
2- Research Department of Gerontology, Academic Center for Education, Culture and Research (ACECR), Shahid Beheshti University of Medical Sciences Branch, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 8817 kb]
(1604 Downloads)
| Abstract (HTML) (3412 Views)
Full-Text: (1366 Views)
Introduction
Mortality is considered one of the primary indicators for assessing population health. Metrics such as mortality rates, the number of deaths, locations, ages, and primary causes of death are pivotal in policymaking, planning, interventions, research prioritization, and the development of new technologies [8]. In this context, identifying the conditions associated with mortality in the elderly is essential to develop and implement strategies aimed at enhancing the quality of additional years gained through increased life expectancy [9]. Additionally, the significant growth in the population aged 70 years and above may create new societal demands. By 2030, it is estimated that this age group, comprising less than 8% of the global population, will account for over 50% of cancer cases, 58% of diabetes cases, 95% of Alzheimer disease and dementia cases, 62% of deaths due to non-communicable diseases, 25% of deaths caused by accidents, and 30% of deaths from infectious diseases [13]. Accordingly, this study examines the common causes of mortality among Iranian elderly aged 60–69 and 70 years and older in the 21st century and compares these findings with global statistics.
Methods
This study analyzes mortality statistics of Iranian elderly individuals as detailed in the global health estimates tables published by the World Health Organization (WHO) for the years 2000, 2010, 2015, and 2019 [15–18]. These tables provide the latest international data on mortality and disability, categorized by region, country, age, gender, and income. They offer key insights into mortality and morbidity trends to aid in health policy formulation and resource allocation.
To estimate these values, data from multiple sources, such as vital statistics recorded by countries, recent WHO technical program estimates, United Nations members and related agencies, and international burden of disease studies, were utilized. Before the publication, global health estimates data are reviewed by WHO members through consultations with national focal points and country and regional offices [19].
Global mortality statistics, based on the number of deaths by country, age group, gender, and cause for the years 2000, 2010, 2015, and 2019, were analyzed [15–18]. The analysis focused on determining disease-specific mortality rates and the proportion of deaths attributable to specific causes [20, 21]. Based on calculations and rankings of these rates and proportions, the 20 most common causes of death and the five leading causes of mortality were identified for elderly men and women in the age groups of 60–69 years and 70 years and older. These findings were compared with global data.
Results
An analysis of mortality statistics for both genders in 2019 in Iran revealed that among those aged 60–69 years, cardiovascular diseases (47.75%), malignancies (22.56%), diabetes (5.98%), unintentional injuries (4.86%), and respiratory diseases (4.53%) were the leading causes of death. In contrast, for those aged 70 years and older, the primary causes were cardiovascular diseases (54.09%), malignancies (15.71%), neurological disorders (6.80%), respiratory diseases (5.42%), and diabetes (4.15%).
From 2000 to 2019, ischemic heart disease and stroke were the top two causes of mortality among Iranian elderly aged 60–69 years. Depending on gender and time period, hypertension-related heart disease and diabetes mellitus were the third leading causes. In 2000, road traffic accidents were also reported as the third leading cause of death among elderly men in this age group. Overall, diabetes, which ranked seventh in 2000, rose to third place in 2019. The Alzheimer disease and other dementias were not common causes of death in this age group during the mentioned periods, ranking between 12th and 18th across genders. Other geriatric syndromes, such as falls, were not among the top 20 causes of mortality in this age group (Table 1).
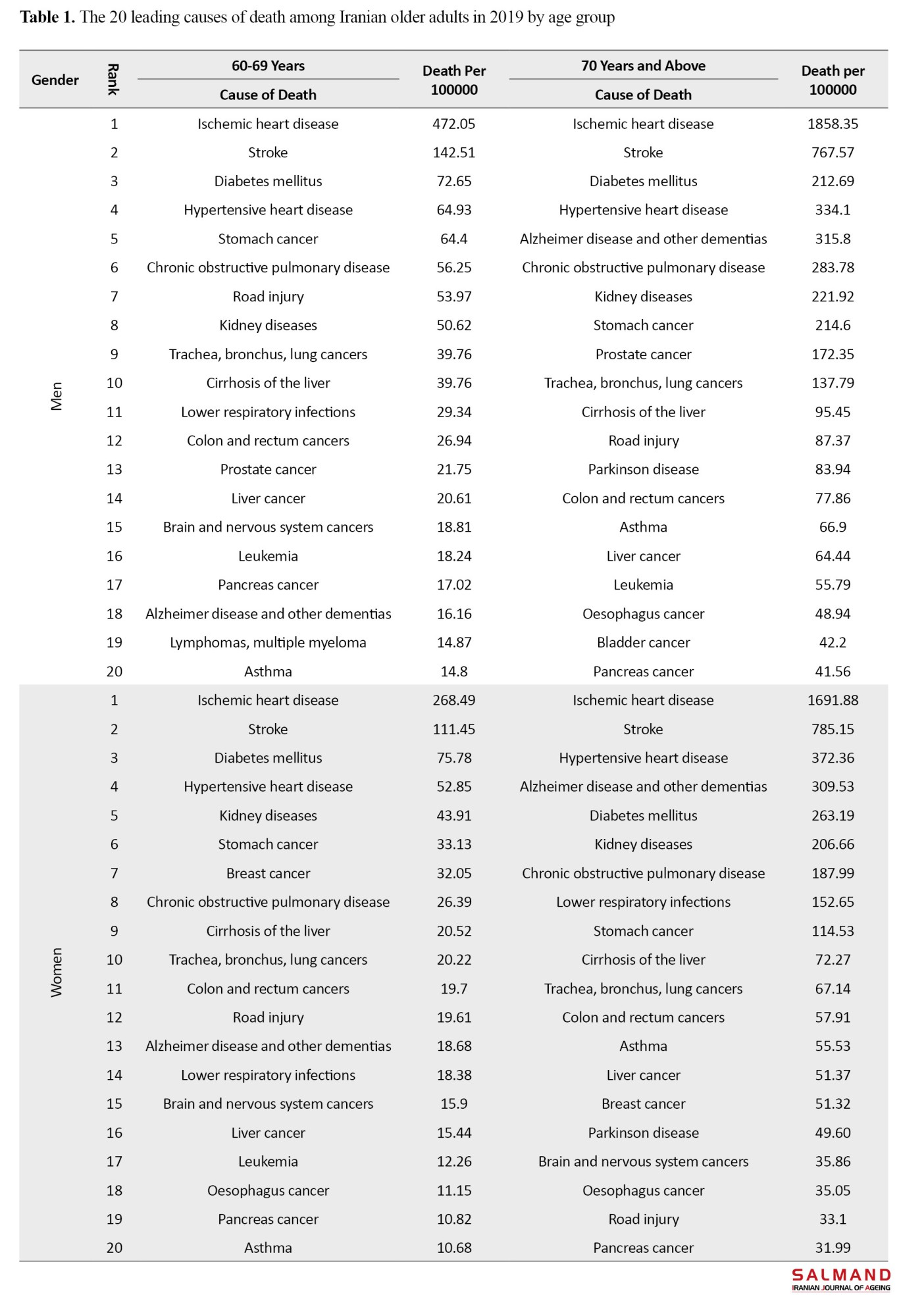
Among those aged 70 and older, ischemic heart disease and stroke were consistently the first and second leading causes of mortality across genders in all four periods. Hypertension was the third leading cause (except for men in 2019). Among men, diabetes was the third leading cause of death in 2019. Deaths due to the Alzheimer disease and other dementias were significantly higher in this age group compared to those under 70, ranking as the fourth leading cause of death among women across all periods. Among men, chronic obstructive pulmonary disease was the fourth leading cause (except in 2019), with the Alzheimer disease and other dementias ranking fifth from 2000 to 2019. Falls were not among the top 20 causes of death for this age group in the 2015 and 2019 studies.
Conclusion
An analysis of the top 20 causes of mortality among Iranian elderly reveals significant differences in the patterns and rates of death between the two age groups, 60–69 years and 70 years and older. For instance, the disease-specific mortality rate for various dementias in the higher than 70 years of age group is approximately 20 times higher than in those under 70, for both genders. These differences should be carefully considered in the study of disease-specific mortality rates, as well as in planning and implementing health strategies for the elderly population.
Given the limitations in data collection and potential methodological changes in preparing these statistics, the WHO-estimated tables may differ from the actual national figures. Therefore, caution is advised when using these results for policymaking and interpreting them in comparisons.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Avicenna Research Institute (ARI), Tehran, Iran (Code: IR.ACECR.AVICENNA.REC.1402.011).
Funding
This study was financially supported by the Shahid Beheshti University of Medical Sciences Branch of ACECR Tehran, Iran.
Authors' contributions
Conceptualization, and study design: Arya Hamedanchi; Writing the initial draft: Arya Hamedanchi and Fereshteh Rezaie; Data analysis and final approval: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors extend their sincere gratitude to the esteemed faculty and staff of the Avicenna Research Institute (ARI) and the Shahid Beheshti University of Medical Sciences Branch of ACECR for their invaluable support and cooperation.
References
Mortality is considered one of the primary indicators for assessing population health. Metrics such as mortality rates, the number of deaths, locations, ages, and primary causes of death are pivotal in policymaking, planning, interventions, research prioritization, and the development of new technologies [8]. In this context, identifying the conditions associated with mortality in the elderly is essential to develop and implement strategies aimed at enhancing the quality of additional years gained through increased life expectancy [9]. Additionally, the significant growth in the population aged 70 years and above may create new societal demands. By 2030, it is estimated that this age group, comprising less than 8% of the global population, will account for over 50% of cancer cases, 58% of diabetes cases, 95% of Alzheimer disease and dementia cases, 62% of deaths due to non-communicable diseases, 25% of deaths caused by accidents, and 30% of deaths from infectious diseases [13]. Accordingly, this study examines the common causes of mortality among Iranian elderly aged 60–69 and 70 years and older in the 21st century and compares these findings with global statistics.
Methods
This study analyzes mortality statistics of Iranian elderly individuals as detailed in the global health estimates tables published by the World Health Organization (WHO) for the years 2000, 2010, 2015, and 2019 [15–18]. These tables provide the latest international data on mortality and disability, categorized by region, country, age, gender, and income. They offer key insights into mortality and morbidity trends to aid in health policy formulation and resource allocation.
To estimate these values, data from multiple sources, such as vital statistics recorded by countries, recent WHO technical program estimates, United Nations members and related agencies, and international burden of disease studies, were utilized. Before the publication, global health estimates data are reviewed by WHO members through consultations with national focal points and country and regional offices [19].
Global mortality statistics, based on the number of deaths by country, age group, gender, and cause for the years 2000, 2010, 2015, and 2019, were analyzed [15–18]. The analysis focused on determining disease-specific mortality rates and the proportion of deaths attributable to specific causes [20, 21]. Based on calculations and rankings of these rates and proportions, the 20 most common causes of death and the five leading causes of mortality were identified for elderly men and women in the age groups of 60–69 years and 70 years and older. These findings were compared with global data.
Results
An analysis of mortality statistics for both genders in 2019 in Iran revealed that among those aged 60–69 years, cardiovascular diseases (47.75%), malignancies (22.56%), diabetes (5.98%), unintentional injuries (4.86%), and respiratory diseases (4.53%) were the leading causes of death. In contrast, for those aged 70 years and older, the primary causes were cardiovascular diseases (54.09%), malignancies (15.71%), neurological disorders (6.80%), respiratory diseases (5.42%), and diabetes (4.15%).
From 2000 to 2019, ischemic heart disease and stroke were the top two causes of mortality among Iranian elderly aged 60–69 years. Depending on gender and time period, hypertension-related heart disease and diabetes mellitus were the third leading causes. In 2000, road traffic accidents were also reported as the third leading cause of death among elderly men in this age group. Overall, diabetes, which ranked seventh in 2000, rose to third place in 2019. The Alzheimer disease and other dementias were not common causes of death in this age group during the mentioned periods, ranking between 12th and 18th across genders. Other geriatric syndromes, such as falls, were not among the top 20 causes of mortality in this age group (Table 1).
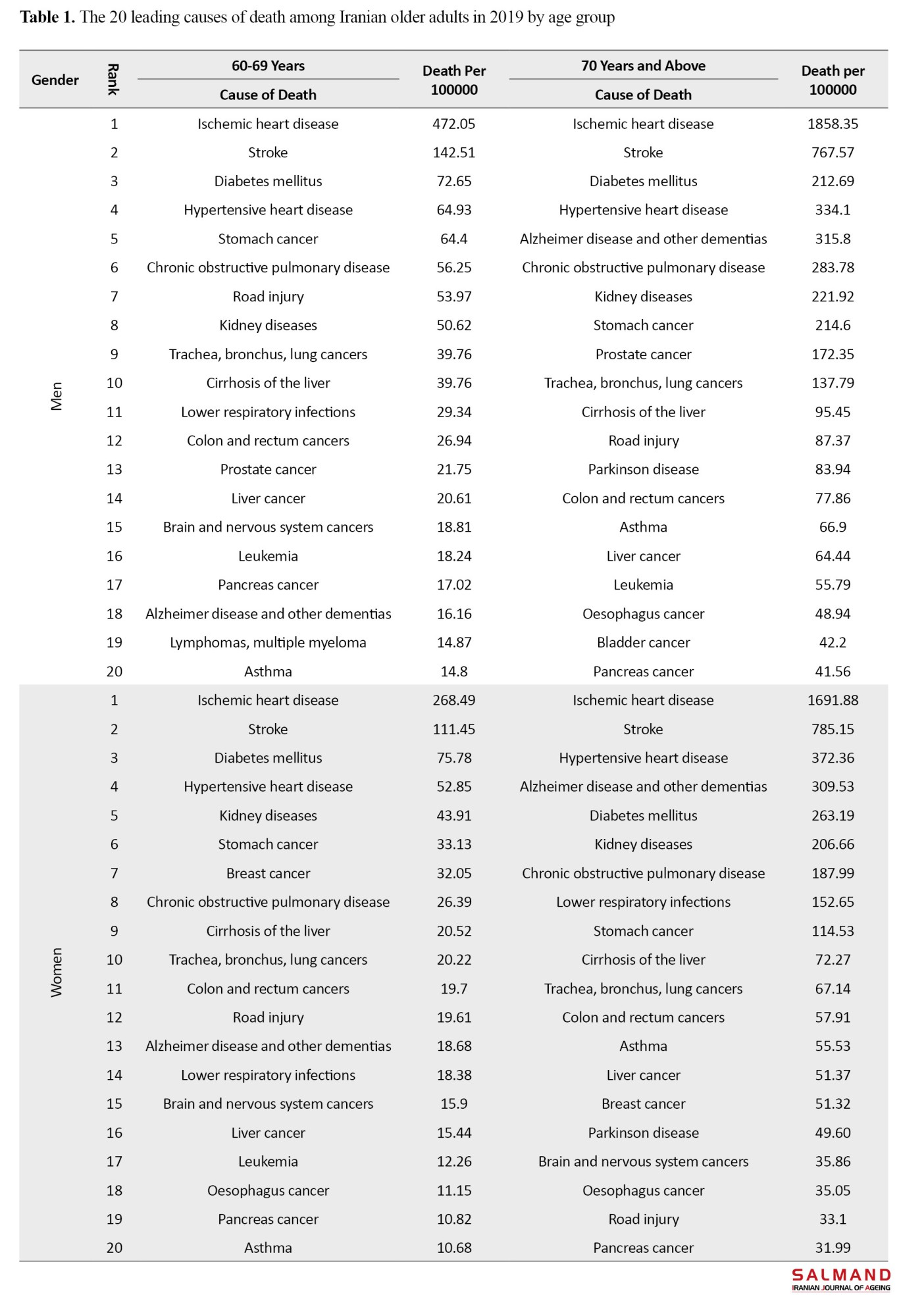
Among those aged 70 and older, ischemic heart disease and stroke were consistently the first and second leading causes of mortality across genders in all four periods. Hypertension was the third leading cause (except for men in 2019). Among men, diabetes was the third leading cause of death in 2019. Deaths due to the Alzheimer disease and other dementias were significantly higher in this age group compared to those under 70, ranking as the fourth leading cause of death among women across all periods. Among men, chronic obstructive pulmonary disease was the fourth leading cause (except in 2019), with the Alzheimer disease and other dementias ranking fifth from 2000 to 2019. Falls were not among the top 20 causes of death for this age group in the 2015 and 2019 studies.
Conclusion
An analysis of the top 20 causes of mortality among Iranian elderly reveals significant differences in the patterns and rates of death between the two age groups, 60–69 years and 70 years and older. For instance, the disease-specific mortality rate for various dementias in the higher than 70 years of age group is approximately 20 times higher than in those under 70, for both genders. These differences should be carefully considered in the study of disease-specific mortality rates, as well as in planning and implementing health strategies for the elderly population.
Given the limitations in data collection and potential methodological changes in preparing these statistics, the WHO-estimated tables may differ from the actual national figures. Therefore, caution is advised when using these results for policymaking and interpreting them in comparisons.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Avicenna Research Institute (ARI), Tehran, Iran (Code: IR.ACECR.AVICENNA.REC.1402.011).
Funding
This study was financially supported by the Shahid Beheshti University of Medical Sciences Branch of ACECR Tehran, Iran.
Authors' contributions
Conceptualization, and study design: Arya Hamedanchi; Writing the initial draft: Arya Hamedanchi and Fereshteh Rezaie; Data analysis and final approval: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors extend their sincere gratitude to the esteemed faculty and staff of the Avicenna Research Institute (ARI) and the Shahid Beheshti University of Medical Sciences Branch of ACECR for their invaluable support and cooperation.
References
- Kyriazis M. Aging as "time-related dysfunction": A perspective. Frontiers in Medicine. 2020; 7:371. [DOI:10.3389/fmed.2020.00371] [PMID]
- World Health Organization (WHO). Ageing and health [Internet]. 2022 [Updated 2024 October 1]. Available from: [Link]
- Hägg S, Jylhävä J, Wang Y, Xu H, Metzner C, Annetorp M, et al. Age, frailty, and comorbidity as prognostic factors for short-term outcomes in patients with coronavirus disease 2019 in geriatric care. Journal of the American Medical Directors Association. 2020; 21(11):1555-9.e2. [DOI:10.1016/j.jamda.2020.08.014]
- Mahmoud M, Carmisciano L, Tagliafico L, Muzyka M, Rosa G, Signori A, et al. Patterns of comorbidity and in-hospital mortality in older patients with COVID-19 infection. Frontiers in Medicine. 2021; 8:726837. [DOI:10.3389/fmed.2021.726837]
- Çinar F, Parlak G, Eti Aslan F. The effect of comorbidity on mortality in elderly patients undergoing emergency abdominal surgery: A systematic review and metaanalysis. Turkish Journal of Medical Sciences. 2021; 51(1):61-7. [DOI:10.3906/sag-2001-27]
- Caughey GE, Ramsay EN, Vitry AI, Gilbert AL, Luszcz MA, Ryan P, et al. Comorbid chronic diseases, discordant impact on mortality in older people: A 14-year longitudinal population study. Journal of Epidemiology and Community Health. 2010; 64(12):1036-42. [DOI:10.1136/jech.2009.088260]
- Bezerra PCdL, Monteiro GTR. Trends in overall mortality and from diseases of the circulatory system in elderly individuals in Rio Branco, Acre, 1980-2012. Revista Brasileira de Geriatria e Gerontologia. 2018; 21(2):143-54. [DOI:10.1590/1981-22562018021.170128]
- Boitrago S, Souza ASO, Cunha PO, Vieira MA, Caldeira AP, Carneiro JA, et al. Mortality in community-dwelling elderly: Coefficient and associated factors. Revista Brasileira de Enfermagem. 2021; 74(suppl 2):e20200612. [DOI:10.1590/0034-7167-2020-0612]
- Fan ZY, Yang Y, Zhang CH, Yin RY, Tang L, Zhang F. Prevalence and patterns of comorbidity among middle-aged and elderly people in China: A cross-sectional study based on Charls data. International Journal of General Medicine. 2021; 14:1449-55. [DOI:10.2147/IJGM.S309783]
- Fathi E, Sharifi M, Ebrahimpour M, Zanjani H. [Major causes of mortality in Iran in 2016 using multiple decrease life tables (Persian)]. Journal of Population Association of Iran. 2019; 13(26):155-85. [Link]
- Zanjari N, Sasanipour M. [Changes in cause of death among the older adults and its effect on increasing life expectancy in Iran (Persian)]. Iranian Journal of Epidemiology. 2022; 18(1):33-44. [Link]
- Imani A, Dastgari S, Azizi Zain al-Hajlo A. [Aging population and burden of diseases (review study) (Persian)]. Depiction of Health. 2015; 6(2):54-61. [Link]
- The World Bank. Life expectancy at birth, total (years)-Iran, Islamic Rep [Internet]. 2022 [Updated 2022 May 1]. Available from: [Link]
- World Health Organization. Estimated deaths (‘000) by cause, sex and WHO Member State. Geneva: WHO; 2000.
- World Health Organization. Estimated deaths (‘000) by cause, sex and WHO Member State (1). Geneva: WHO; 2010.
- World Health Organization. Estimated deaths (‘000) by cause, sex and WHO Member State (1). Geneva: WHO; 2015.
- World Health Organization. Estimated deaths (‘000) by cause, sex and WHO Member State (1).Geneva: WHO; 2019.
- World Health Organization. Global health estimates: Leading causes of death [Internet]. 2019 [Update 2023 October 1]. Available from: [Link]
- Celentano DD, Szklo M. Gordis epidemiology. Philadelphia Elsevier; 2018. [Link]
- Park K. Park’s textbook of preventive and social medicine. New Delhi: Bhanot Publishers India; 2017. [Link]
- United Nations. World Population Prospects 2024 [Internet]. 2024 [Updated 2024 November 3]. Available from: [Link]
- Kim EJ, Jung SW, Kim YE, Go DS, Yoon SJ. Assessing the impact of aging on burden of disease. Iranian Journal of Public Health. 2018; 47(Suppl 1):33-8. [PMID] [PMCID]
- Duncan BB, Schmidt MI, GBD 2019 Collaborators. Global, regional, and national burden of diseases and injuries for adults 70 years and older: Systematic analysis for the global burden of disease 2019 study. BMJ. 2022; 376:e068208. [DOI:10.1136/bmj-2021-068208 ]
- Torkashvand Moradabadi M, Abbasi M. [An epidemiological study of mortality among elderly in iran using years of life lost (YLL) index during 2011 to 2017 (Persian)]. Payesh. 2020; 19(1):85-97. [DOI:10.29252/payesh.19.1.85]
- Najafi B, Bakhtiyari F, Manavi A, Soufinejad MR, Fakhrzadeh H, Arzaghi M, et al. [Elderly death cause and death registry accuracy in kahrizak charity foundation (Persian)]. Iranian Journal of Diabetes and Lipid Disorders. 2014; 13(6):455-61. [Link]
- Karimi A, Sahaf R, Taghavi N, Rasafiani M, Aliakbari Kamrani A, Khosravi A, et al. [Mortality causes in adult and elderly Iranian male veterans (Persian)]. Iranian Journal of War and Public Health. 2015; 7(3):157-65. [Link]
- Torkashvand Moradabadi M, Torkashvand Z. [Epidemiological transition and the importance of social policy: Mortality statistic in Ilam, Iran during 2011-2017 (Persian)]. Payesh. 2019; 18(4):321-31. [Link]
- Tubi K, Gholamreza S. [Investigating the causes of death in the population covered by Birjand University of Medical Sciences (Persian)]. Birjand University of Medical Sciences. 2003; 10(2):17-25. [Link]
- World Health Organization. Cardiovascular diseases (CVDs) [Internet]. 2021 [Updated 2021 June 11]. Available from: [Link]
- World Health Organization. WHo mortality database: Interactive platform visualizing mortality data [Internet]. 2023 [Updated 2023 June 11]. Available from: [Link]
- Coll PP, Korc-Grodzicki B, Ristau BT, Shahrokni A, Koshy A, Filippova OT, et al. Cancer prevention and screening for older adults: Part 2. Interventions to prevent and screen for breast, prostate, cervical, ovarian, and endometrial cancer. Journal of the American Geriatrics Society. 2020; 68(11):2684-91. [DOI:10.1111/jgs.16794]
- Soerjomataram I, Bray F. Planning for tomorrow: Global cancer incidence and the role of prevention 2020-2070. Nature Reviews Clinical Oncology. 2021; 18(10):663-72. [DOI:10.1038/s41571-021-00514-z]
- Pilleron S, Sarfati D, Janssen-Heijnen M, Vignat J, Ferlay J, Bray F, et al. Global cancer incidence in older adults, 2012 and 2035: A population-based study. International Journal of Cancer. 2019; 144(1):49-58. [DOI:10.1002/ijc.31664]
- Pourqanbari I, Rezai Sharif F, Mokhtari Z, Ahmadzadeh M, Jamali Motlagh E. Comparison of the prevalence of chronic diseases in the elderly in urban and rural areas. Paper presented in: The 10th International Conference on Health, Treatment and Health Promotion. 7 July 2022; Tbilisi, Georgia. [Link]
- Khamseh ME, Sepanlou SG, Hashemi-Madani N, Joukar F, Mehrparvar AH, Faramarzi E, et al. Nationwide prevalence of diabetes and prediabetes and associated risk factors among Iranian Adults: Analysis of data from Persian cohort study. Diabetes Therapy. 2021; 12(11):2921-38. [DOI:10.1007/s13300-021-01152-5]
- Sinclair A, Robert I, Croxson S. Mortality in older people with diabetes mellitus. Diabetic Medicine. 1997; 14(8):639-47. [DOI:10.1002/(SICI)1096-9136(199708)14:83.0.CO;2-C]
- Su B, Wang Y, Dong Y, Hu G, Xu Y, Peng X, et al. Trends in diabetes mortality in urban and rural China, 1987-2019: A joinpoint regression analysis. Frontiers in Endocrinology. 2022; 12:777654. [DOI:10.3389/fendo.2021.777654]
- Jafarvand E, Ataey A, Edalati S. Epidemiology and death trends due to diabetes in Iran. Internal Medicine Today. 2021; 27(2):198-213. [DOI:10.32598/hms.27.2.2764.1]
- Pan American Health Organization. Panorama of Diabetes in the Americas. Washington, D.C.: PAHO; 2022. [Link]
- Forbes A, Murrells T, Sinclair A. Examining factors associated with excess mortality in older people (age≥ 70 years) with diabetes-A 10-year cohort study of older people with and without diabetes. Diabetic Medicine. 2017; 34(3):387-95. [DOI:10.1111/dme.13132]
- Aziz Z, Absetz P, Oldroyd J, Pronk NP, Oldenburg B. A systematic review of real-world diabetes prevention programs: Learnings from the last 15 years. Implementation Science 2015; 10:172. [DOI:10.1186/s13012-015-0354-6]
- World Health Organization (WHO). Hypertension [Internet]. 2023 [Updated 2023 March 16]. Available from: [Link]
- Rigaud AS, Forette B. Hypertension in older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2001; 56(4):M217-25. [DOI:10.1093/gerona/56.4.M217]
- Motlagh M, Yazdani S, Taheri Tanjani P. [Elderly health profile in Islamic Republic of Iran (Persian)]. Tehran: Foujhangraphic. 2014. [Link]
- Oori MJ, Mohammadi F, Norozi K, Fallahi-Khoshknab M, Ebadi A, Gheshlagh RG. Prevalence of HTN in Iran: Meta-analysis of published studies in 2004-2018. Current Hypertension Reviews. 2019; 15(2):113-22. [DOI:10.2174/1573402115666190118142818]
- Simpson O, Camorlinga SG. A framework to study the emergence of non-communicable diseases. Procedia Computer Science. 2017; 114:116-25. [DOI:10.1016/j.procs.2017.09.026]
- Khademi N, Gooya MM, Izade B, Mansory F, Laghai Z. [Decreasing risk factors of non-communicable diseases among health workers of Kermanshah University of Medical Sciences (2008-2010) (Persian)]. Hakim. 2013; 15(4):330-8. [Link]
- Hamidi Parsa H, Elahi N, Rezaei M, Jafari M. [Economic analysis of Iran’s health system transformation plan using the structural break tests (Persian)]. Qom University of Medical Sciences Journal. 2023; 16(11):890-901. [DOI:10.32598/qums.16.11.2077.1]
- Goli S, Mahjub H, Goli M, Sadeghi FM. [Risk factors ranking of non-communicable disease in different provinces of Iran using multivariate factor analysis methods (Persian)]. Journal of Knowledge & Health. 2018; 12(4):7-15. [Link]
- Helali Sotoudeh M, Hashemianfar SA, Javaheri F. [How the health policy happens in the framework of the power system: Discourse analysis of the health reform plan in the 11th and 12th governments (Persian)]. Sociological Review. 2022; 1-25. [Link]
- Damari B, Heidari A. [Implementation of integrated management of non-communicable disease prevention and control in Iran: A proposal (Persian)]. Payesh. 2020; 19(1):7-17. [DOI:10.29252/payesh.19.1.7]
Type of Study: Research |
Subject:
Geriatric
Received: 2023/11/17 | Accepted: 2024/02/06 | Published: 2025/01/01
Received: 2023/11/17 | Accepted: 2024/02/06 | Published: 2025/01/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |