Volume 20, Issue 3 (Autumn 2025)
Salmand: Iranian Journal of Ageing 2025, 20(3): 356-371 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hosseini S R, Zabihi A, Hosseinnejad Roshan S M, Ghadimi R, Sefidchian A, Ahmadi Ahangar A et al . Factors Associated With Chronic Pain in Older Adults: Second Phase of the Amirkola Health and Ageing Project (AHAP) Cohort Study in North of Iran. Salmand: Iranian Journal of Ageing 2025; 20 (3) :356-371
URL: http://salmandj.uswr.ac.ir/article-1-2881-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2881-en.html
Seyed Reza Hosseini *1 

 , Ali Zabihi2
, Ali Zabihi2 

 , Seyedeh Mahdieh Hosseinnejad Roshan3
, Seyedeh Mahdieh Hosseinnejad Roshan3 

 , Reza Ghadimi2
, Reza Ghadimi2 

 , Alireza Sefidchian4
, Alireza Sefidchian4 

 , Alijan Ahmadi Ahangar5
, Alijan Ahmadi Ahangar5 

 , Ali Bijani2
, Ali Bijani2 




 , Ali Zabihi2
, Ali Zabihi2 

 , Seyedeh Mahdieh Hosseinnejad Roshan3
, Seyedeh Mahdieh Hosseinnejad Roshan3 

 , Reza Ghadimi2
, Reza Ghadimi2 

 , Alireza Sefidchian4
, Alireza Sefidchian4 

 , Alijan Ahmadi Ahangar5
, Alijan Ahmadi Ahangar5 

 , Ali Bijani2
, Ali Bijani2 


1- Social Determinants of Health Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran. , hossenirezaseyed@gmail.com
2- Social Determinants of Health Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
3- Student Research Committee, Babol University of Medical Sciences, Babol, Iran.
4- Department of Psychiatry, Faculty of Medicine, Shahid Yahyanejad Hospital, Babol University of Medical Sciences, Babol, Iran.
5- Movement Disorders Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
2- Social Determinants of Health Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
3- Student Research Committee, Babol University of Medical Sciences, Babol, Iran.
4- Department of Psychiatry, Faculty of Medicine, Shahid Yahyanejad Hospital, Babol University of Medical Sciences, Babol, Iran.
5- Movement Disorders Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
Full-Text [PDF 5825 kb]
(1089 Downloads)
| Abstract (HTML) (2372 Views)
Conclusion
In Amirkola City, 67.6% of older adults suffer from chronic pain, most of whom are women and those higher with higher age. The chronic pain in older adults is strongly associated with sleep quality disorders, depressive symptoms, and the number of chronic diseases.
The development of appropriate interventions based on these factors to reduce the chronic pain of older adults is recommended.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Babol University of Medical Sciences, Babol, Iran (Code: IR.MUBABOL.HRI.REC.1398.352). After providing initial explanations, informed consent was obtained from all participants or their legal guardians. All procedures were performed in accordance with relevant guidelines.
Funding
This study was funded by Babol University of Medical Sciences, Babol, Iran (Grant Number: 724132234).
Authors' contributions
Design, writing and investigation: Seyed Reza Hosseini, Ali Zabihi and Mahdieh Hosseininejad Roshan; editing and review: Seyed Reza Hosseini, Reza Ghadimi, Alireza Sefidchian, Alijan Ahmadi Ahangar, and Ali Zabihi; data analysis: Ali Bijani; preparation of the initial draft: Ali Zabihi and Mahdieh Hosseininejad; Final approval: all authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the Vice-Chancellor for Research and Technology of Babol University of Medical Sciences, Babol, Iran, for financial support, the staff of the health centers in Amirkola for their cooperation in this study, and all seniors for participating in this study.
References
Full-Text: (655 Views)
Introduction
Chronic pain is common in older people. There is limited evidence for the predictors of chronic pain in old age. It is important to identify risk factors for chronic pain because they can guide preventive interventions and improve clinical management. In the general population, the predictors of chronic pain are constant. They are: Age, female gender, low social class, socioeconomic status, properties of pain (severity and number of pain points), psychological disorders (anxiety, depression), comorbidities, and genetic factors [7]. Therefore, given that chronic pain in older people is common, the need to find out factors linked to chronic pain in the older population to develop treatment strategies and prevention for chronic pain is imperative. This study aims to investigate the factors related to chronic pain in older adults living in Amirkola City, Mazandaran, north of Iran.
Methods
This is a descriptive-analytical study with a cross-sectional design, as a second phase of the Amirkla health and ageing project (AHAP) cohort study. Participants were 1675 older adults living in Amirkola City. They were divided into two groups depending on whether they had chronic pain or not. Their demographic factors, cognitive status using the mini-mental state examination (MMSE), depressive symptoms using the geriatric depression scale (GDS), sleep quality using the Pittsburgh sleep quality index (PSQI), frailty using the FRAIL scale, and physical activity using the physical activity scale for the elderly (PASE), were measured.
Demographic information included age, sex, educational level, marital status, occupation, level of satisfaction with income, and use of sleeping pills, which were surveyed using a demographic form.
Chronic musculoskeletal pain and its location were surveyed using a questionnaire. Older people were asked if they had experienced pain in any of the following areas in the last six months, lasting for 3 months or longer: Hands, wrists, elbows, shoulders, face, jaw, neck, hip joints, knees, ankles, feet, and back.
The collected data were analyzed in SPSS software, version 24 using chi-square, t-test, and multiple logistic regression analysis. P<0.05 was considered statistically significant.
Results
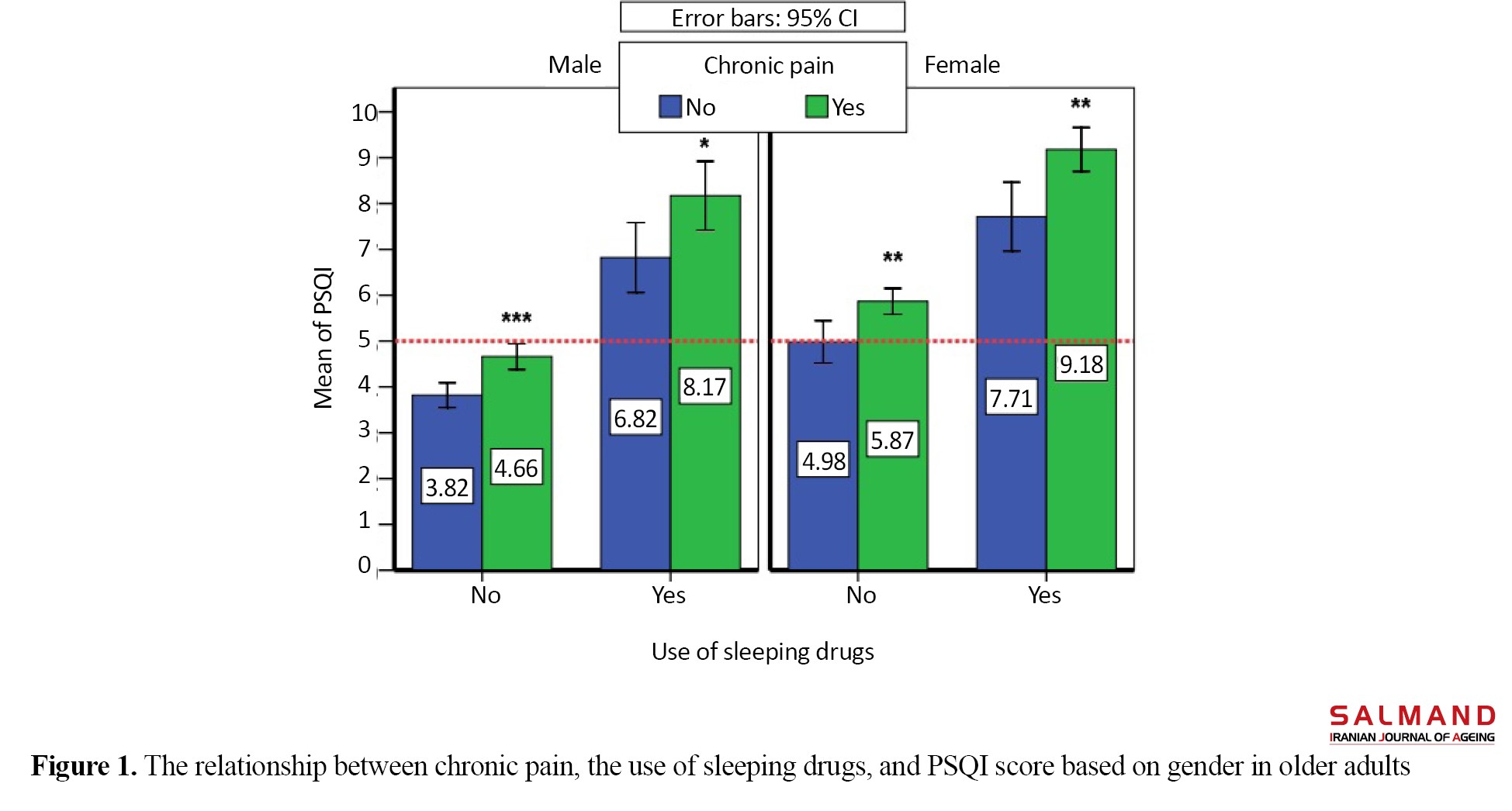
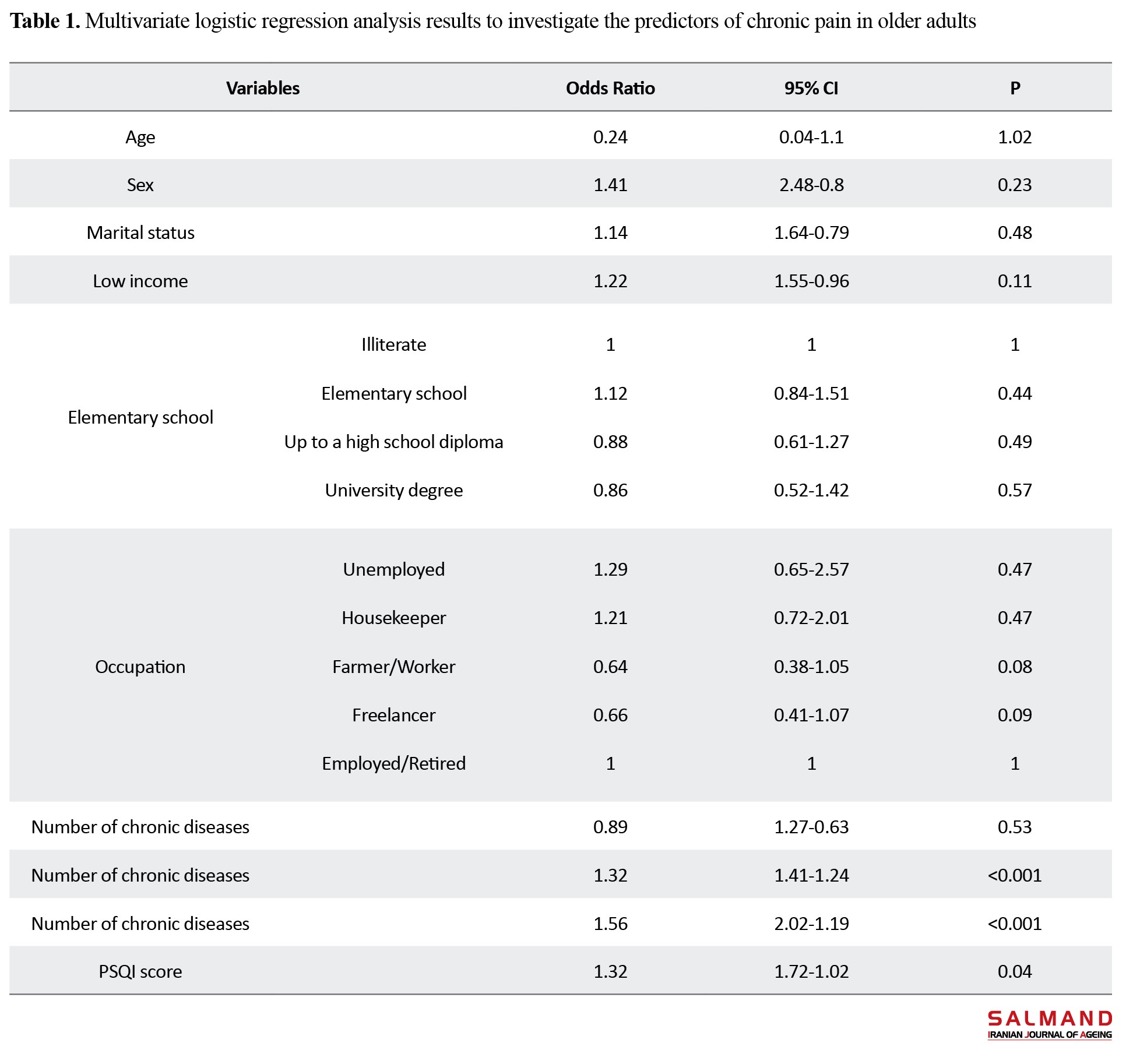
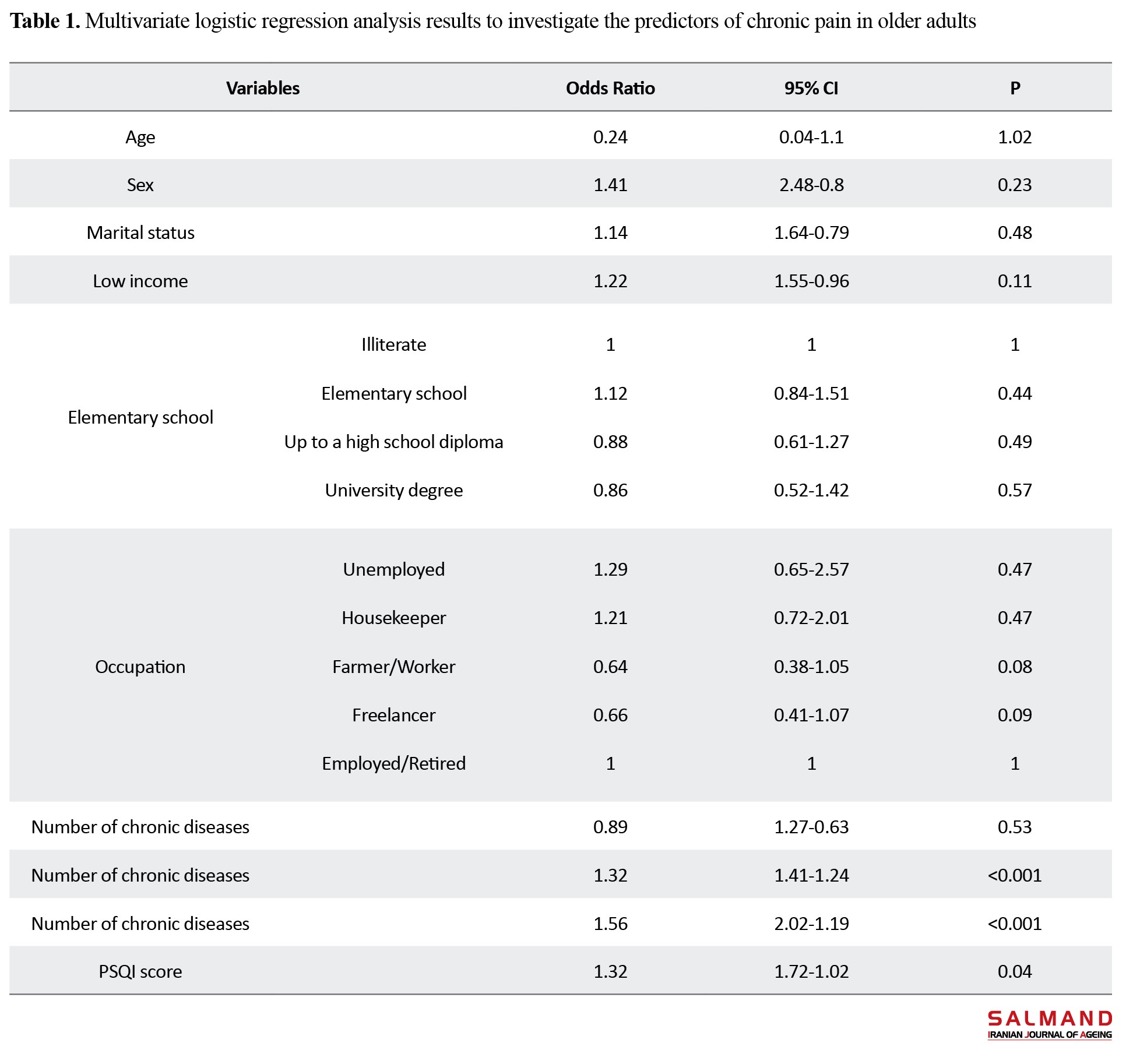
The participants were mostly male, married, illiterate, and housekeepers. The majority of the elderly (76.52%) were pre-frail or frail. Chronic pain was significantly more common among unmarried women, those with a low level of education, those living alone, housewives, those unsatisfied with their income, disabled people, users of sleeping pills, those with poor sleep quality, and those with depressive symptoms. The mean age, GDS score, PSQI score, and the number of chronic diseases were significantly higher and the PASE and MMSE scores were significantly lower in the group with chronic pain than those without chronic pain. The results of multivariate logistic regression analysis with Enter method showed that number of chronic diseases, depressive symptoms and sleep disorder had the highest association with chronic pain (Table 1).
The mean PSQI score was higher in older women and men with chronic pain using sleeping pills (Figure 1).
Chronic pain is common in older people. There is limited evidence for the predictors of chronic pain in old age. It is important to identify risk factors for chronic pain because they can guide preventive interventions and improve clinical management. In the general population, the predictors of chronic pain are constant. They are: Age, female gender, low social class, socioeconomic status, properties of pain (severity and number of pain points), psychological disorders (anxiety, depression), comorbidities, and genetic factors [7]. Therefore, given that chronic pain in older people is common, the need to find out factors linked to chronic pain in the older population to develop treatment strategies and prevention for chronic pain is imperative. This study aims to investigate the factors related to chronic pain in older adults living in Amirkola City, Mazandaran, north of Iran.
Methods
This is a descriptive-analytical study with a cross-sectional design, as a second phase of the Amirkla health and ageing project (AHAP) cohort study. Participants were 1675 older adults living in Amirkola City. They were divided into two groups depending on whether they had chronic pain or not. Their demographic factors, cognitive status using the mini-mental state examination (MMSE), depressive symptoms using the geriatric depression scale (GDS), sleep quality using the Pittsburgh sleep quality index (PSQI), frailty using the FRAIL scale, and physical activity using the physical activity scale for the elderly (PASE), were measured.
Demographic information included age, sex, educational level, marital status, occupation, level of satisfaction with income, and use of sleeping pills, which were surveyed using a demographic form.
Chronic musculoskeletal pain and its location were surveyed using a questionnaire. Older people were asked if they had experienced pain in any of the following areas in the last six months, lasting for 3 months or longer: Hands, wrists, elbows, shoulders, face, jaw, neck, hip joints, knees, ankles, feet, and back.
The collected data were analyzed in SPSS software, version 24 using chi-square, t-test, and multiple logistic regression analysis. P<0.05 was considered statistically significant.
Results
The participants were mostly male, married, illiterate, and housekeepers. The majority of the elderly (76.52%) were pre-frail or frail. Chronic pain was significantly more common among unmarried women, those with a low level of education, those living alone, housewives, those unsatisfied with their income, disabled people, users of sleeping pills, those with poor sleep quality, and those with depressive symptoms. The mean age, GDS score, PSQI score, and the number of chronic diseases were significantly higher and the PASE and MMSE scores were significantly lower in the group with chronic pain than those without chronic pain. The results of multivariate logistic regression analysis with Enter method showed that number of chronic diseases, depressive symptoms and sleep disorder had the highest association with chronic pain (Table 1).
The mean PSQI score was higher in older women and men with chronic pain using sleeping pills (Figure 1).
Conclusion
In Amirkola City, 67.6% of older adults suffer from chronic pain, most of whom are women and those higher with higher age. The chronic pain in older adults is strongly associated with sleep quality disorders, depressive symptoms, and the number of chronic diseases.
The development of appropriate interventions based on these factors to reduce the chronic pain of older adults is recommended.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Babol University of Medical Sciences, Babol, Iran (Code: IR.MUBABOL.HRI.REC.1398.352). After providing initial explanations, informed consent was obtained from all participants or their legal guardians. All procedures were performed in accordance with relevant guidelines.
Funding
This study was funded by Babol University of Medical Sciences, Babol, Iran (Grant Number: 724132234).
Authors' contributions
Design, writing and investigation: Seyed Reza Hosseini, Ali Zabihi and Mahdieh Hosseininejad Roshan; editing and review: Seyed Reza Hosseini, Reza Ghadimi, Alireza Sefidchian, Alijan Ahmadi Ahangar, and Ali Zabihi; data analysis: Ali Bijani; preparation of the initial draft: Ali Zabihi and Mahdieh Hosseininejad; Final approval: all authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the Vice-Chancellor for Research and Technology of Babol University of Medical Sciences, Babol, Iran, for financial support, the staff of the health centers in Amirkola for their cooperation in this study, and all seniors for participating in this study.
References
- Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges, and compromises. Pain. 2020; 161(9):1976-82. [DOI:10.1097/j.pain.0000000000001939] [PMID]
- Kuner R, Flor H. Structural plasticity and reorganisation in chronic pain. Nature Reviews. Neuroscience. 2016;1 8(1):20-30. [DOI:10.1038/nrn.2016.162] [PMID]
- Dagnino APA, Campos MM. Chronic pain in the elderly: Mechanisms and perspectives. Frontiers in Human Neuroscience. 2022; 16:736688. [DOI:10.3389/fnhum.2022.736688] [PMID]
- Janbazi L, Kazemian A, Mansouri K, Madani SP, Yousefi N, Vahedifard F, et al. The incidence and characteristics of chronic pain and fatigue after 12 months later admitting with COVID-19; The Post-COVID 19 syndrome. American Journal of Physical Medicine & Rehabilitation. 2022; 10.1097/PHM.0000000000002030. Advance online publication. [DOI:10.1097/PHM.0000000000002030] [PMID]
- Liberman O, Freud T, Peleg R, Keren A, Press Y. Chronic pain and geriatric syndromes in community-dwelling patients aged≥ 65 years. Journal of Pain Research. 2018; 11:1171-80. [DOI:10.2147/JPR.S160847] [PMID]
- Majedi H, Amini MH, Yousefshahi F, Khazaeipour Z, Majedi M, Rahimi M, et al. Predicting factors of pain duration in patients with chronic pain: A large population-based study. Anesthesiology and Pain Medicine. 2020; 10(1):e95776. [DOI:10.5812/aapm.95776]
- van Hecke O, Torrance N, Smith BH. Chronic pain epidemiology and its clinical relevance. British Journal of Anaesthesia. 2013; 111(1):13-8. [DOI:10.1093/bja/aet123] [PMID]
- Mills SE, Nicolson KP, Smith BH. Chronic pain: A review of its epidemiology and associated factors in population-based studies. British Journal of Anaesthesia. 2019; 123(2):e273-83. [DOI:10.1016/j.bja.2019.03.023] [PMID]
- Larsson C, Hansson EE, Sundquist K, Jakobsson U. Chronic pain in older adults: Prevalence, incidence, and risk factors. Scandinavian Journal of Rheumatology. 2017; 46(4):317-25. [DOI:10.1080/03009742.2016.1218543] [PMID]
- Ferretti F, Silva MRd, Pegoraro F, Baldo JE, Sá CAD. Chronic pain in the elderly, associated factors and relation with the level and volume of physical activity. BrJP. 2019; 2:3-7. [DOI:10.5935/2595-0118.20190002]
- Dev MK, Paudel N, Joshi ND, Shah DN, Subba S. Psycho-social impact of visual impairment on health-related quality of life among nursing home residents. BMC Health Services Research. 2014; 14:345. [DOI:10.1186/1472-6963-14-345] [PMID]
- Bastami F, Salahshoori A, Shirani F, Mohtashami A, Sharafkhani N. [Risk factors of depression on the elderly: A review study (Persian)]. Journal of Gerontology. 2016; 1(2):54-65. [DOI:10.18869/acadpub.joge.1.2.54]
- Hosseini S, Zabihi A, Jafarian Amiri S, Bijani A. The relationship between chronic diseases and disability in daily activities and instrumental activities of daily living in the elderly. Journal of Babol University of Medical Sciences. 2018; 20(5):23-9. [Link]
- Khodadadi S, Pourhadi S, Hosseini SR, Sum S, Kheirkhah F, Mohammadi Z. [Investigating the relationship between social support, cognitive status, and depression with daily life activities of the elderly in Amirkola City (Persian)]. Iranian Journal of Ageing. 2022; 17(1):2-15. [DOI:10.32598/sija.2021.593.4]
- Giebel CM, Sutcliffe C, Challis D. Activities of daily living and quality of life across different stages of dementia: A UK study. Aging & Mental Health. 2015; 19(1):63-71. [DOI:10.1080/13607863.2014.915920] [PMID]
- Saeidimehr S, Geravandi S, Izadmehr A, Mohammadi MJ. [Relationship between the “Quality of Life” and symptoms of depression among older adults (Persian)]. Iranian Journal of Ageing. 2016; 11(1):90-9. [DOI:10.21859/sija-110190]
- Sadock BJ, Sadock VA, Kaplan HI. Kaplan and Sadock’s concise textbook of child and adolescent psychiatry. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2009. [Link]
- Nourhashémi F, Andrieu S, Gillette-Guyonnet S, Vellas B, Albarède JL, Grandjean H. Instrumental activities of daily living as a potential marker of frailty: A study of 7364 community-dwelling elderly women (the EPIDOS study). The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2001; 56(7):M448-53. [DOI:10.1093/gerona/56.7.M448] [PMID]
- Ahmadi S, Khankeh H, Mohammadi F, Fallahi M, Reza Soltani P. [The effect of sleep restriction treatment on quality of sleep in the elders (Persian)]. Iranian Journal of Ageing. 2010; 5(16):7-15. [Link]
- Gulia KK, Kumar VM. Sleep disorders in the elderly: A growing challenge. Psychogeriatrics. 2018; 18(3):155-65. [DOI:10.1111/psyg.12319] [PMID]
- Foroughan M, Shahboulaghi FM, Jafari Z, Rashedi V, Biglarian A. Pain characteristics of older residents in Iranian nursing homes. Eastern Mediterranean Health Journal. 2019; 25(3):205-12.[DOI:10.26719/emhj.18.045] [PMID]
- Heidari GA, Tavafian SS. The relationship between anxiety and chronic pain: A cross-sectional study from Yazd, Iran. International Journal of Musculoskeletal Pain Prevention. 2016; 1(2):87-92. [Link]
- Bijani A, Ghadimi R, Mikaniki E, Kheirkhah F, Mozaffarpur SA, Motallebnejad M, et al. Cohort profile update: The Amirkola health and ageing project (AHAP). Caspian Journal of Internal Medicine. 2017; 8(3):205-12. [PMID]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research,. 1989; 28(2):193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Farrahi Moghaddam J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P). Sleep & Breathing. 2012; 16(1):79-82. [DOI:10.1007/s11325-010-0478-5] [PMID]
- Yesavage JA, Sheikh JI. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontologist. 1986; 5(1-2):165-73. [DOI:10.1300/J018v05n01_09]
- Malakouti SK, Fatollahi P, Mirabzadeh A, Salavati M, Zandi T. Reliability, validity and factor structure of the GDS‐15 in Iranian elderly. International Journal of Geriatric Psychiatry: A Journal of the Psychiatry of Late Life and Allied Sciences. 2006; 21(6):588-93. [DOI:10.1002/gps.1533] [PMID]
- Gleason LJ, Benton EA, Alvarez-Nebreda ML, Weaver MJ, Harris MB, Javedan H. FRAIL questionnaire screening tool and short-term outcomes in geriatric fracture patients. Journal of the American Medical Directors Association. 2017; 18(12):1082-6. [DOI:10.1016/j.jamda.2017.07.005] [PMID]
- Alqahtani BA, Nasser TA. Assessment of frailty in Saudi community-dwelling older adults: Validation of measurements. Annals of Saudi Medicine. 2019; 39(3):197-204. [DOI:10.5144/0256-4947.2019.197] [PMID]
- Tavan F, Asadollahi A. Psychometric properties of frailty syndrome checklist 5-items in frail older adults in Iran. Journal of Health Sciences & Surveillance System. 2021; 9(3):162-8. [DOI:10.30476/jhsss.2021.88650.1152]
- Keikavoosi-Arani L, Salehi L. Cultural adaptation and psychometric adequacy of the Persian version of the physical activity scale for the elderly (P-PASE). BMC Research Notes. 2019; 12(1):555. [DOI:10.1186/s13104-019-4591-7] [PMID]
- Foroughan M, Jafari Z, Shirin Bayan P, Ghaem Magham Farahani Z, Rahgozar M. [Validation of Mini- Mental State Examination (MMSE) in the elderly population of Tehran (Persian)]. Advances in Cognitive Sciences. 2008; 10(2):29-37. [Link]
- Seyedian M, Fallah M, Norouzian M, Nejat S, Delavar A, Ghasemzadeh H. Validity of the Farsi version of mini-mental state examination. Journal of Medical Council of Islamic Republic of Iran. 2007; 25(4): Pe408-14. [Link]
- Barbosa MH, Bolina AF, Tavares JL, Cordeiro AL, Luiz RB, de Oliveira KF. Sociodemographic and health factors associated with chronic pain in institutionalized elderly. Revista Latino-Americana de Enfermagem. 2014; 22(6):1009-16. [DOI:10.1590/0104-1169.3552.2510] [PMID]
- Mallon T, Eisele M, König HH, Brettschneider C, Röhr S, Pabst A, et al. Lifestyle aspects as a predictor of pain among oldest-old primary care patients - A longitudinal cohort study. Clinical Interventions in Aging. 2019; 14:1881-8. [DOI:10.2147/CIA.S217431] [PMID]
- Gallant NL, Hadjistavropoulos T. Experiencing pain in the presence of others: A structured experimental investigation of older adults. The Journal of Pain. 2017; 18(4):456-67. [DOI:10.1016/j.jpain.2016.12.009] [PMID]
- Wei X, Dong Z, Cheng L, Guo Z, Lv Z. Identifing the gender-specific genes and pathways in osteoarthritis by bioinfromatics. Osteoarthritis and Cartilage. 2020; 28(Supplement 1):S207-8. [DOI:10.1016/j.joca.2020.02.338]
- Malon J, Shah P, Koh WY, Cattabriga G, Li E, Cao L. Characterizing the demographics of chronic pain patients in the state of Maine using the Maine all payer claims database. BMC Public Health. 2018; 18(1):810. [DOI:10.1186/s12889-018-5673-5] [PMID]
- Mailis-Gagnon A, Yegneswaran B, Lakha SF, Nicholson K, Steiman AJ, Ng D, et al. Pain characteristics and demographics of patients attending a university-affiliated pain clinic in Toronto, Ontario. Pain Research & Management. 2007; 12(2):93-9. [PMID]
- Maly A, Vallerand AH. Neighborhood, socioeconomic, and racial influence on chronic pain. Pain Management Nursing. 2018; 19(1):14-22. [DOI:10.1016/j.pmn.2017.11.004] [PMID]
- LaRowe LR, Miaskowski C, Miller A, Mayfield A, Keefe FJ, Smith AK, et al. Prevalence and sociodemographic correlates of chronic pain among a nationally representative sample of older adults in the United States. The Journal of Pain. 2024; 25(10):104614. [DOI:10.1016/j.jpain.2024.104614] [PMID]
- Ho A, Nair S. Global chronic pain: Public and population health responses. Developments in Neuroethics and Bioethics. Amsterdam: Elsevier; 2018. [DOI:10.1016/bs.dnb.2018.08.009]
- Shaw WS, Linton SJ, Pransky G. Reducing sickness absence from work due to low back pain: How well do intervention strategies match modifiable risk factors? Journal of Occupational Rehabilitation. 2006; 16(4):591-605. [DOI:10.1007/s10926-006-9061-0] [PMID]
- Hassan H, Alsherbieny E, Fahmy M. Effect of elderly women’s socio-demographic characteristics on knee osteoarthritis pain. American Journal of Medical Sciences and Medicine. 2023; 11(2):39-46. [Link]
- Fahmy MR, Hassan HE, El-sherbieny EM. Coping strategies among elderly women suffering from knee osteoarthritis pain at Beni-Suef city. NILES Journal for Geriatric and Gerontology. 2023; 6(1):148-66. [DOI:10.21608/niles.2023.279733]
- Parreira PC, Maher CG, Ferreira ML, Machado GC, Blyth FM, Naganathan V, et al. A longitudinal study of the influence of comorbidities and lifestyle factors on low back pain in older men. Pain. 2017; 158(8):1571-6. [DOI:10.1097/j.pain.0000000000000952] [PMID]
- Mookerjee N, Schmalbach N, Antinori G, Thampi S, Windle-Puente D, Gilligan A, et al. Association of risk factors and comorbidities with chronic pain in the elderly population. Journal of Primary Care & Community Health. 2024; 15:21501319241233463. [DOI:10.1177/21501319241233463] [PMID]
- Rouch I, Edjolo A, Laurent B, Pongan E, Dartigues JF, Amieva H. Association between chronic pain and long-term cognitive decline in a population-based cohort of elderly participants. Pain. 2021; 162(2):552-60. [DOI:10.1097/j.pain.0000000000002047] [PMID]
- Zhang Q, Yu M, Tang R, Wang H, Xiao M, Geng G, et al. A pathway model of chronic pain and frailty in older Chinese cancer patients: The mediating effect of sleep. Geriatric Nursing. 2023; 50:215-21. [DOI:10.1016/j.gerinurse.2023.01.015] [PMID]
- Suzuki K, Miyamoto M, Hirata K. Sleep disorders in the elderly: Diagnosis and management. Journal of General and Family Medicine. 2017; 18(2):61-71. [DOI:10.1002/jgf2.27] [PMID]
- Jank R, Gallee A, Boeckle M, Fiegl S, Pieh C. Chronic pain and sleep disorders in primary care. Pain Research and Treatment. 2017; 2017(1):9081802. [DOI:10.1155/2017/9081802] [PMID]
- Axén I. Pain-related sleep disturbance: A prospective study with repeated measures. The Clinical Journal of Pain. 2016; 32(3):254-9. [DOI:10.1097/AJP.0000000000000249] [PMID]
- Nijs J, Mairesse O, Neu D, Leysen L, Danneels L, Cagnie B, et al. Sleep disturbances in chronic pain: Neurobiology, assessment, and treatment in physical therapist practice. Physical Therapy. 2018; 98(5):325-35. [DOI:10.1093/ptj/pzy020] [PMID]
- Zis P, Daskalaki A, Bountouni I, Sykioti P, Varrassi G, Paladini A. Depression and chronic pain in the elderly: Links and management challenges. Clinical Interventions in Aging. 2017; 12:709-20.[DOI:10.2147/CIA.S113576] [PMID]
- Denkinger MD, Lukas A, Nikolaus T, Peter R, Franke S, Group AS. Multisite pain, pain frequency and pain severity are associated with depression in older adults: Results from the ActiFE Ulm study. Age and Ageing. 2014; 43(4):510-4. [DOI:10.1093/ageing/afu013] [PMID]
Type of Study: Research |
Subject:
Geriatric
Received: 2024/06/25 | Accepted: 2024/10/27 | Published: 2025/10/01
Received: 2024/06/25 | Accepted: 2024/10/27 | Published: 2025/10/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |