Volume 20, Issue 3 (Autumn 2025)
Salmand: Iranian Journal of Ageing 2025, 20(3): 438-453 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nazaripanah N S, Nadrian H, Gilani N, Hahsemiparast M. Evaluating the Integrated Geriatric Care Program in a Health Center in Yazd, Iran, Based on the RE-AIM Framework. Salmand: Iranian Journal of Ageing 2025; 20 (3) :438-453
URL: http://salmandj.uswr.ac.ir/article-1-2884-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2884-en.html
1- Psychiatry and Behavioral Medicine Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
2- Department of Health Education and Promotion, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran. & Social Determinants of Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran. ,haidarnadrian@gmail.com
3- Medical Education Research Center, Tabriz University of Medical Sciences, Tabriz, Iran. & Department of Biostatistics and Epidemiology, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran.
4- Social Determinants of Health Research Center, Zanjan University of Medical Sciences, Tabriz, Iran. & Department of Health Education and Promotion, Faculty of Health,Zanjan University of Medical Sciences, Zanjan, Iran.
2- Department of Health Education and Promotion, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran. & Social Determinants of Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran. ,
3- Medical Education Research Center, Tabriz University of Medical Sciences, Tabriz, Iran. & Department of Biostatistics and Epidemiology, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran.
4- Social Determinants of Health Research Center, Zanjan University of Medical Sciences, Tabriz, Iran. & Department of Health Education and Promotion, Faculty of Health,Zanjan University of Medical Sciences, Zanjan, Iran.
Keywords: Geriatric health care, Reach, effectiveness, adoption, implementation, and maintenance (RE-AIM), Older adults, Evaluation
Full-Text [PDF 8108 kb]
(1034 Downloads)
| Abstract (HTML) (2586 Views)
References
Full-Text: (461 Views)
Introduction
The aging population poses a global challenge. Recently, there has been a rising concern about the increasing prevalence of older people suffering from several chronic diseases at the same time. Such concerns have led to the enhancement of national programs aimed at improving the health, function, and quality of life of older people in Iran. In this regard, a national plan titled “integrated geriatric care program” (IGCP) is currently being implemented by the Iranian Ministry of Health and Medical Education in healthcare centers across Iran. In this plan, the risk factors and key clinical symptoms have been used for early diagnosis, appropriate treatment, and timely referral.
Although healthcare services are being provided to older adults in Iran, there are still many challenges in terms of structure, specialized organizational resources, and service delivery. The evaluation of these service delivery program can help assess the current status, identify service delivery gaps and the areas for improvement. On of the theoretical framework for this purpose is called the reach, effectiveness, adoption, implementation, and maintenance (RE-AIM) model. The use of this model is reported to be suitable for those in the fields of geriatric care, public health, and related disciplines. This study aims to evaluate the IGCP in Yazd City, Iran, based on the RE-AIM model.
Methods & Materials
This is a cross-sectional study conducted at Imamshahr Health Center in Yazd in 2023. Data collection was conducted in two phases. In the first phase, all program indicators from 2016 to 2022 were extracted from the electronic health records of 1,672 older adults covered by the mentioned health center. Then, the obtained data were categorized according to the five dimensions of the RE-AIM model. In the second phase, supplementary information was collected using a researcher-made questionnaire from all healthcare providers at the mentioned health center (n=9). The researcher-made questionnaire was developed by the research team based on the IGCP booklet. It had five sections based on the five dimensions of the RE-AIM model. The results of the expert panel assessments affirmed the adequate validity and reliability of this questionnaire (CVR=0.98, CVI=0.97, Cronbach’s α=0.878).
Data analyses were performed in SPSS software, version 26. Data preprocessing was done to identify outliers and missing values and the normality of data distribution was tested. Friedman test was used to determine the difference between standardized scores of the five evaluation dimensions. The significance level was set at 0.05. The trend of changes in indicators was analyzed using time-series models from 2016 to 2022, followed by forecasting these indicators for 2023. The time-series analysis and forecasting were conducted using the auto regressive integrated moving average (ARIMA) model based on the available data (indicators from 2016 to 2022), employing the Forecast Package and selecting the auto.arima function in R software, version 4.2.2.
Results
First phase
To determine the effects of implementing the IGCP, the trend of changes in the indicators from 2016 to 2022 was plotted. The indicators of care for blood pressure, depression, falls, and nutrition showed that 508, 427, 459, and 470 older people had received these types of care in 2023, respectively. The total number of covered older adults reached 2,780 people in 2022. The highest number of older people participating in group education classes was 44 in 2019. The number and percentage of total care reached 427 people and 15.4% in 2022, respectively.
The forecast value for the total number of covered older adults for 2023 was 2788 (95% CI, 2573.99%, 3002.01%). The number of total care for 2023 was predicted to be 189.29 (95% CI, 43.22%, 421.79%). The values obtained for the total number of covered older adults and the number of total care in 2023 were 2,855 and 571 persons, respectively, which aligns with the forecast values.
Second phase
In the second phase, 9 healthcare providers (5 female and 4 male) with a mean age of 39.11±9.22 years participated. The participants included two physicians, five public health experts, one psychologist, and one nutritionist who responded to the researcher-made questionnaire. Based on the results presented in Table 1, the mean scores were 34.26±15.28 for reach, 49.51±12.08 for effectiveness, 58.64±32.41 for adoption, 72.11±9.98 for implementation, and 55.71±12.26 for maintenance.
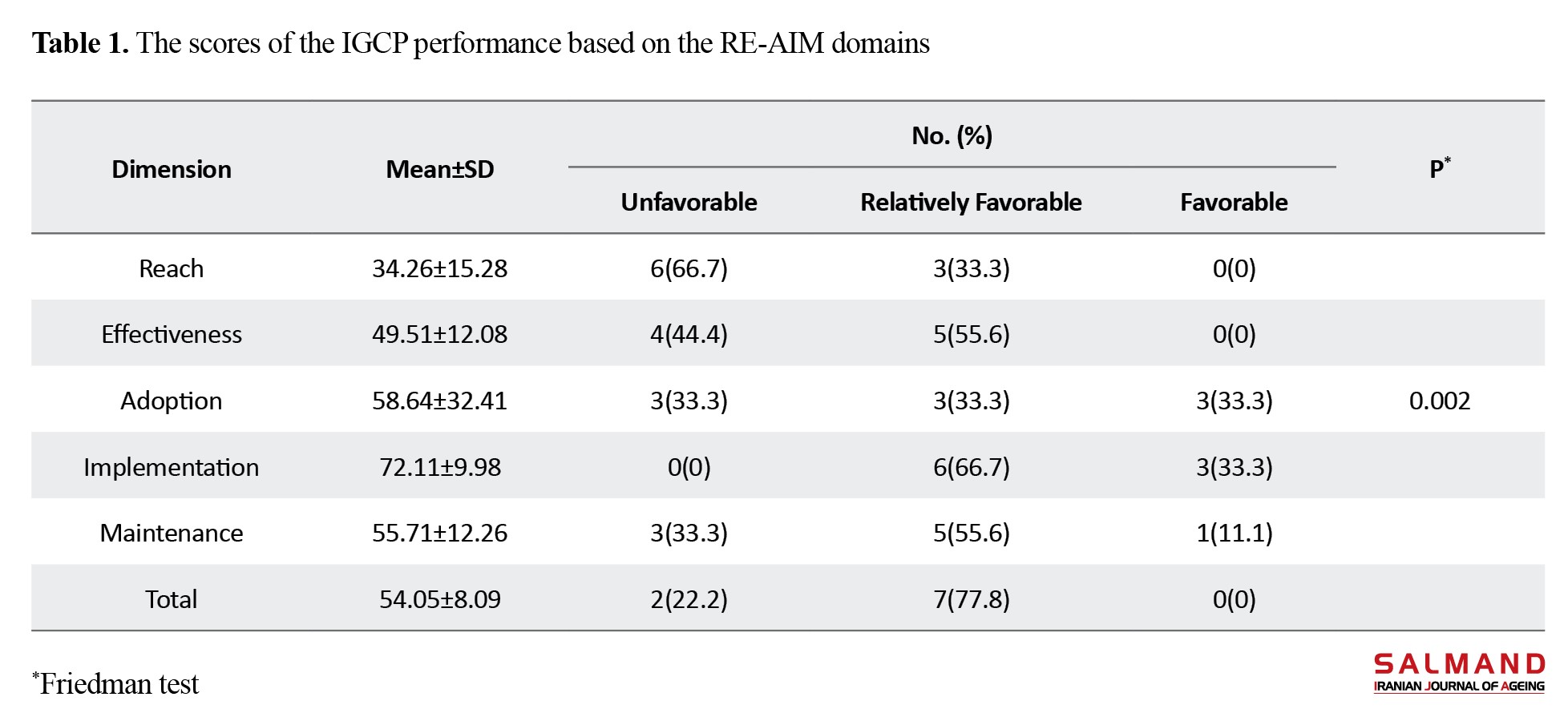
As can be seen, the highest and lowest scores were related to the dimensions of implementation and reach, respectively. According to 66.7% of healthcare providers, the IGCP had unfavorable performance based on the reach dimension. From the perspective of 66.7%, the program had relatively favorable performance in the implementation dimension. Overall, 77.8% of healthcare providers considered the program to have relatively favorable performance. The Friedman test results indicated a statistically significant difference between the scores of different RE-AIM model dimensions (P=0.002).
Conclusion
Overall, the IGCP implementation at Imamshahr Health Center in Yazd is relatively favorable. Based on the reach domain of the RE-AIM framework, the participation of older adults in the program was weak. Therefore, there is a need for necessary actions to improve the participation of older adults in the future. This study provides valuable information that can be a basis for evaluating other programs in primary healthcare. Our findings highlight the importance of aligning the health service delivery programs with the predetermined organizational goals to improve the program implementation. Furthermore, the results of this study provide policymakers and health managers of geriatric care programs in Iran with insights for better decision-making and planning in the future.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Tabriz University of Medical Sciences, Tabriz, Iran (Code: IR.TBZMED.REC.1401.100).
Funding
This article was extracted from the dissertation of Neda Sadat Nazaripanah, funded by Tabriz University of Medical Sciences, Tabriz, Iran (Grant No: 68748).
Authors' contributions
Conceptualization and methodology: Neda Sadat Nazaripanah and, Haidar Nadrian; Validation: Neda Sadat Nazaripanah and, Neda Gilani; Data analysis: Neda Sadat Nazaripanah, Haidar Nadrian and, Neda Gilani; Investigation, editing & review: Neda Sadat Nazaripanah, Haidar Nadrian and, Mina Hahsemiparast; Initial draft preparation: Neda Sadat Nazaripanah; Visualization: All authors; Supervision: Neda Sadat Nazaripanah and , Haidar Nadrian; Project administration, resources, and funding acquisition: Haidar Nadrian.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research and Technology of Tabriz University of Medical Sciences for the financial support and the personnel of Imamshahr Health Center in Yazd city and all participants for their cooperation.
The aging population poses a global challenge. Recently, there has been a rising concern about the increasing prevalence of older people suffering from several chronic diseases at the same time. Such concerns have led to the enhancement of national programs aimed at improving the health, function, and quality of life of older people in Iran. In this regard, a national plan titled “integrated geriatric care program” (IGCP) is currently being implemented by the Iranian Ministry of Health and Medical Education in healthcare centers across Iran. In this plan, the risk factors and key clinical symptoms have been used for early diagnosis, appropriate treatment, and timely referral.
Although healthcare services are being provided to older adults in Iran, there are still many challenges in terms of structure, specialized organizational resources, and service delivery. The evaluation of these service delivery program can help assess the current status, identify service delivery gaps and the areas for improvement. On of the theoretical framework for this purpose is called the reach, effectiveness, adoption, implementation, and maintenance (RE-AIM) model. The use of this model is reported to be suitable for those in the fields of geriatric care, public health, and related disciplines. This study aims to evaluate the IGCP in Yazd City, Iran, based on the RE-AIM model.
Methods & Materials
This is a cross-sectional study conducted at Imamshahr Health Center in Yazd in 2023. Data collection was conducted in two phases. In the first phase, all program indicators from 2016 to 2022 were extracted from the electronic health records of 1,672 older adults covered by the mentioned health center. Then, the obtained data were categorized according to the five dimensions of the RE-AIM model. In the second phase, supplementary information was collected using a researcher-made questionnaire from all healthcare providers at the mentioned health center (n=9). The researcher-made questionnaire was developed by the research team based on the IGCP booklet. It had five sections based on the five dimensions of the RE-AIM model. The results of the expert panel assessments affirmed the adequate validity and reliability of this questionnaire (CVR=0.98, CVI=0.97, Cronbach’s α=0.878).
Data analyses were performed in SPSS software, version 26. Data preprocessing was done to identify outliers and missing values and the normality of data distribution was tested. Friedman test was used to determine the difference between standardized scores of the five evaluation dimensions. The significance level was set at 0.05. The trend of changes in indicators was analyzed using time-series models from 2016 to 2022, followed by forecasting these indicators for 2023. The time-series analysis and forecasting were conducted using the auto regressive integrated moving average (ARIMA) model based on the available data (indicators from 2016 to 2022), employing the Forecast Package and selecting the auto.arima function in R software, version 4.2.2.
Results
First phase
To determine the effects of implementing the IGCP, the trend of changes in the indicators from 2016 to 2022 was plotted. The indicators of care for blood pressure, depression, falls, and nutrition showed that 508, 427, 459, and 470 older people had received these types of care in 2023, respectively. The total number of covered older adults reached 2,780 people in 2022. The highest number of older people participating in group education classes was 44 in 2019. The number and percentage of total care reached 427 people and 15.4% in 2022, respectively.
The forecast value for the total number of covered older adults for 2023 was 2788 (95% CI, 2573.99%, 3002.01%). The number of total care for 2023 was predicted to be 189.29 (95% CI, 43.22%, 421.79%). The values obtained for the total number of covered older adults and the number of total care in 2023 were 2,855 and 571 persons, respectively, which aligns with the forecast values.
Second phase
In the second phase, 9 healthcare providers (5 female and 4 male) with a mean age of 39.11±9.22 years participated. The participants included two physicians, five public health experts, one psychologist, and one nutritionist who responded to the researcher-made questionnaire. Based on the results presented in Table 1, the mean scores were 34.26±15.28 for reach, 49.51±12.08 for effectiveness, 58.64±32.41 for adoption, 72.11±9.98 for implementation, and 55.71±12.26 for maintenance.
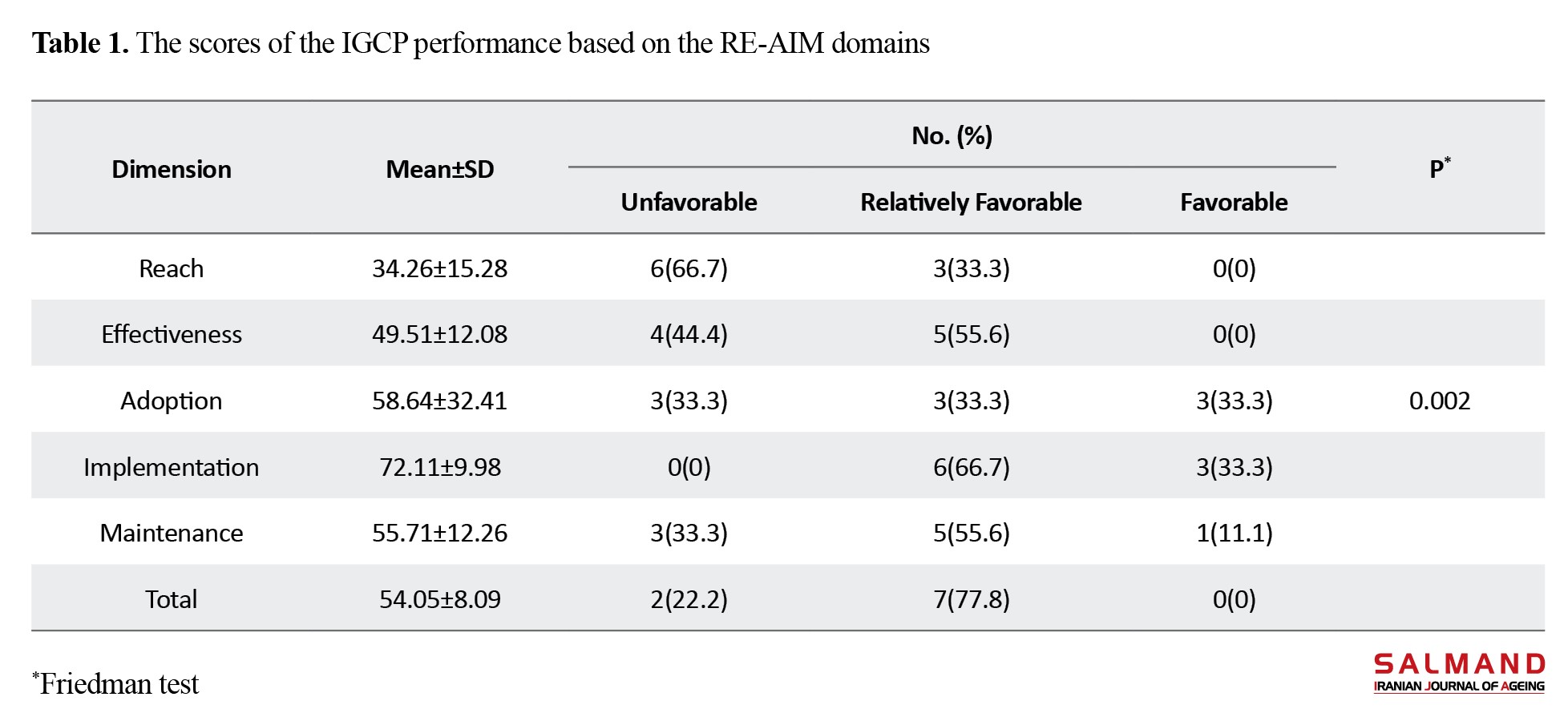
As can be seen, the highest and lowest scores were related to the dimensions of implementation and reach, respectively. According to 66.7% of healthcare providers, the IGCP had unfavorable performance based on the reach dimension. From the perspective of 66.7%, the program had relatively favorable performance in the implementation dimension. Overall, 77.8% of healthcare providers considered the program to have relatively favorable performance. The Friedman test results indicated a statistically significant difference between the scores of different RE-AIM model dimensions (P=0.002).
Conclusion
Overall, the IGCP implementation at Imamshahr Health Center in Yazd is relatively favorable. Based on the reach domain of the RE-AIM framework, the participation of older adults in the program was weak. Therefore, there is a need for necessary actions to improve the participation of older adults in the future. This study provides valuable information that can be a basis for evaluating other programs in primary healthcare. Our findings highlight the importance of aligning the health service delivery programs with the predetermined organizational goals to improve the program implementation. Furthermore, the results of this study provide policymakers and health managers of geriatric care programs in Iran with insights for better decision-making and planning in the future.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Tabriz University of Medical Sciences, Tabriz, Iran (Code: IR.TBZMED.REC.1401.100).
Funding
This article was extracted from the dissertation of Neda Sadat Nazaripanah, funded by Tabriz University of Medical Sciences, Tabriz, Iran (Grant No: 68748).
Authors' contributions
Conceptualization and methodology: Neda Sadat Nazaripanah and, Haidar Nadrian; Validation: Neda Sadat Nazaripanah and, Neda Gilani; Data analysis: Neda Sadat Nazaripanah, Haidar Nadrian and, Neda Gilani; Investigation, editing & review: Neda Sadat Nazaripanah, Haidar Nadrian and, Mina Hahsemiparast; Initial draft preparation: Neda Sadat Nazaripanah; Visualization: All authors; Supervision: Neda Sadat Nazaripanah and , Haidar Nadrian; Project administration, resources, and funding acquisition: Haidar Nadrian.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research and Technology of Tabriz University of Medical Sciences for the financial support and the personnel of Imamshahr Health Center in Yazd city and all participants for their cooperation.
References
- Maresova P, Javanmardi E, Barakovic S, Barakovic Husic J, Tomsone S, Krejcar O, et al. Consequences of chronic diseases and other limitations associated with old age - a scoping review. BMC Public Health. 2019; 19(1):1431. [DOI:10.1186/s12889-019-7762-5] [PMID]
- Fong JH. Disability incidence and functional decline among older adults with major chronic diseases. BMC Geriatrics. 19(1):323. [DOI:10.1186/s12877-019-1348-z] [PMID]
- Skou ST, Mair FS, Fortin M, Guthrie B, Nunes BP, Miranda JJ, et al. Multimorbidity. Nature Reviews. Disease Primers. 2022; 8(1):48. [DOI:10.1038/s41572-022-00376-4] [PMID]
- Ofori-Asenso R, Chin KL, Curtis AJ, Zomer E, Zoungas S, Liew D. Recent patterns of multimorbidity among older adults in high-income countries. Population Health Management. 2019; 22(2):127-37. [DOI:10.1089/pop.2018.0069] [PMID]
- WHO . WHO European Centre for Primary Health Care: annual report of activities 2017. Geneva: World Health Organization. Regional Office for Europe; 2018. [Link]
- Shati M, Azimi MS, Davari S, Solbi Z, Ladoni Sh, Kargozar E, et al. [Integrated and comperhensive health care system for elderly people (for health care staff) (Persian)]. Tehran: Ministry of Health and Medical Education; 2019.
- Nayeri ND, Abazari F, Pouraboli B. Challenges in caring for the elderly in Iran: A systematic review. Ethiopian Medical Journal. 2018; 56(2). [Link]
- Khojamli MA, Dabbaghi FA, Mahmoodi GH. Comparison of integrated care of the elderly in Iran with other selected countries, a comparative study. Pakistan Journal of Medical and Health Sciences. 2021; 14(4):1435-42. [Link]
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. BMJ. 2021; 374:n2061. [DOI:10.1136/bmj.n2061] [PMID]
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health. 1999; 89(9):1322-7. [DOI:10.2105/AJPH.89.9.1322] [PMID]
- Glasgow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter GC, et al. RE-AIM planning and evaluation framework: Adapting to new science and practice with a 20-year review. Frontiers in Public Health. 2019; 7:64. [DOI:10.3389/fpubh.2019.00064] [PMID]
- Ory MG, Altpeter M, Belza B, Helduser J, Zhang C, Smith ML. Perceived Utility of the RE-AIM framework for health promotion/disease prevention initiatives for older adults: A case study from the U.S. evidence-based disease prevention initiative. Frontiers in Public Health. 2015; 2:143. [DOI:10.3389/fpubh.2014.00143] [PMID]
- Schwingel A, Gálvez P, Linares D, Sebastião E. Using a Mixed-Methods RE-AIM framework to evaluate community health programs for older Latinas.Journal of Aging and Health. 2017; 29(4):551-93. [DOI:10.1177/0898264316641075] [PMID]
- Foroumandi E, Alizadeh M, Khodayari-Zarnaq R, Kheirouri S. Process evaluation of a national elderly nutrition-care program in Iran: Perspectives of clients and providers. Risk Management and Healthcare Policy. 2020; 13:1135-47. [DOI:10.2147/RMHP.S261121] [PMID]
- Kohzadi N, Boyd MS, Kermanshahi B, Kaastra I. A comparison of artificial neural network and time series models for forecasting commodity prices. Neurocomputing. 1996; 10(2):169-81. [DOI:10.1016/0925-2312(95)00020-8]
- Borges RA, Tomicki C, Almeida FA, Schwingel A, Chodzko-Zajko W, Benedetti TRB. Reach of “VAMOS” program in basic healthcare-organizational barriers and facilitators. Revista Brasileira de Geriatria e Gerontologia. 2019; 22(03):e180225. [DOI:10.1590/1981-22562019022.180225]
- Najafi M, Gholipour K, Amerzadeh M, Kiaei MZ, Kalhor R. A framework for elderly participation in Primary Health Care in Tabriz Health complexes. BMC Geriatrics. 2023; 23(1):499.[DOI:10.1186/s12877-023-04217-1] [PMID]
- Zendehtalab HR, Vanaki Z, Memarian R. [Improving the quality of geriatric care for the healthy elderly in a comprehensive health centers in Iran (Persian)]. Iranian Journal of Ageing. 2021; 15(4):428-39. [DOI:10.32598/sija.15.4.2881.1]
- Moghadasi AM, Sum S, Matlabi H. Why do older people not use the public health services of the integrated aging program? A multidimensional approach in a qualitative study. BMC Health Services Research. 2022; 22(1):1288. [DOI:10.1186/s12913-022-08689-6] [PMID]
- Dabbaghi F, Mahmoodi G. [Integrated care for the elderly in Health Care Centers: A qualitative study (Persian)]. Iran J Nurs Reas. 2021; 16(1):10-27. [Link]
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Services Research. 2018; 18(1):350. [DOI:10.1186/s12913-018-3161-3] [PMID]
- Lotfalinezhad E, Abolfathi Momtaz Y, Nazaripanah N S, Honarvar MR, Arab Ameri F, Azimi MS. [Effectiveness of integrated and comprehensive geriatric care program of ministry of health on physical and mental health of older adults in Golestan Province (Persian)]. Salmand: Iranian Journal of Ageing. 2021; 16(3):438-451. [DOI:10.32598/sija.2020.16.3.2190.2]
- Domènech-Abella J, Lara E, Rubio-Valera M, Olaya B, Moneta MV, Rico-Uribe LA, et al. Loneliness and depression in the elderly: The role of social network. Social Psychiatry and Psychiatric Epidemiology. 2017; 52(4):381-90. [DOI:10.1007/s00127-017-1339-3] [PMID]
- Røyset B, Talseth-Palmer BA, Lydersen S, Farup PG. Effects of a fall prevention program in elderly: A pragmatic observational study in two orthopedic departments. Clinical Interventions in Aging. 2019; 14:145-54. [DOI:10.2147/CIA.S191832] [PMID]
- Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020; 139:6-11. [DOI:10.1016/j.maturitas.2020.05.018] [PMID]
- Melis RJ, van Eijken MI, Teerenstra S, van Achterberg T, Parker SG, Borm GF, et al. A randomized study of a multidisciplinary program to intervene on geriatric syndromes in vulnerable older people who live at home (Dutch EASYcare Study). The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2008; 63(3):283-90. [DOI:10.1093/gerona/63.3.283] [PMID]
- Martínez-González NA, Berchtold P, Ullman K, Busato A, Egger M. Integrated care programmes for adults with chronic conditions: A meta-review. International Journal for Quality in Health Care. 2014; 26(5):561-70. [DOI:10.1093/intqhc/mzu071] [PMID]
- Eklund K, Wilhelmson K. Outcomes of coordinated and integrated interventions targeting frail elderly people: A systematic review of randomised controlled trials. Health & Social Care in the Community. 2009; 17(5):447-58. [DOI:10.1111/j.1365-2524.2009.00844.x] [PMID]
- Hébert R, Dubois MF, Raîche M, Dubuc N; PRISMA-Estrie Group. The effectiveness of the PRISMA integrated service delivery network: Preliminary report on methods and baseline data. International Journal of Integrated Care. 2008; 8:e03. [DOI:10.5334/ijic.229] [PMID]
- Overbeek A, Korfage IJ, Jabbarian LJ, Billekens P, Hammes BJ, Polinder S, et al. Advance care planning in frail older adults: A cluster randomized controlled trial. Journal of The American Geriatrics Society. 2018; 66(6):1089-95. [DOI:10.1111/jgs.15333] [PMID]
- Taheri E, Araban M, Ghanbari S, Moradi Kalboland M. The relationship between health literacy and rate of receiving integrated and comprehensive geriatric care program with self-care ability in elderly women. Journal of Health Literacy. 2022; 7(1):45-55. [DOI: 10.22038/jhl.2022.62350.1252]
- Benedetti TRB, Schwingel A, Gomez LSR, Chodzko-Zajko W. Program” VAMOS”(Active Living, Enhancing Health): from conception to initial findings. Revista Brasileira de Cineantropometria & Desempenho Humano. 2012; 14(6):723-37. [DOI:10.5007/1980-0037.2012v14n6p723]
- Goharinezhad S, Maleki M, Baradaran HR, Ravaghi H. A qualitative study of the current situation of elderly care in Iran: What can we do for the future? Global Health Action. 2016; 9:32156.[DOI:10.3402/gha.v9.32156] [PMID]
- Bello TK, Gericke GJ, MacIntyre UE. Development, implementation, and process evaluation of a theory-based nutrition education programme for adults living With HIV in Abeokuta, Nigeria. Frontiers in Public Health. 2019; 7:30. [DOI:10.3389/fpubh.2019.00030] [PMID]
- Kim YE, Hong SW. Health-related effects of the elderly care program. BioMed Research International. 2018; 2018:7121037. [DOI:10.1155/2018/7121037] [PMID]
- Petrescu-Prahova M, Belza B, Kohn M, Miyawaki C. Implementation and maintenance of a community-based older adult physical activity program. The Gerontologist. 2016; 56(4):677-86.[DOI:10.1093/geront/gnv024] [PMID]
- Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the diabetes prevention program into the community. The DEPLOY Pilot Study. American Journal of Preventive Medicine. 2008; 35(4):357-63. [DOI:10.1016/j.amepre.2008.06.035] [PMID]
- Cleverley WO, Cleverley JO, Parks AV. Essentials of health care finance. Burlington: Jones & Bartlett Learning; 2023. [Link]
- Jancey J, Lee A, Howat P, Clarke A, Wang K, Shilton T. Reducing attrition in physical activity programs for older adults. Journal of Aging and Physical Activity. 2007; 15(2):152-65. [DOI:10.1123/japa.15.2.152] [PMID]
- Miech EJ, Rattray NA, Flanagan ME, Damschroder L, Schmid AA, Damush TM. Inside help: An integrative review of champions in healthcare-related implementation. SAGE Open Medicine. 2018; 6:2050312118773261. [DOI:10.1177/2050312118773261] [PMID]
- Buman MP, Giacobbi PR Jr, Dzierzewski JM, Morgan AA, McCrae CS, Roberts BL, et al. Peer Volunteers Improve long-term maintenance of physical activity with older adults: A randomized controlled trial. Journal of Physical Activity & Health. 2011; 8(s2):S257-66. [DOI:10.1123/jpah.8.s2.s257] [PMID]
- Van Orden KA, Lutz J. Peer support for older adults. Peer Support in Medicine: A Quick Guide. 2021; 115-29. [DOI:10.1007/978-3-030-58660-7_6]
Type of Study: Research |
Subject:
gerontology
Received: 2024/07/28 | Accepted: 2024/09/29 | Published: 2025/10/01
Received: 2024/07/28 | Accepted: 2024/09/29 | Published: 2025/10/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |