Volume 18, Issue 2 (Summer 2023)
Salmand: Iranian Journal of Ageing 2023, 18(2): 162-177 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Iranagh J A, Mohammadi F, Salem Safi P, Ayoughi V, Sedghiani A, Razi S. Non-pharmacological Intervention to Reduce Sleep Disturbance Among Elderly: A Randomized Controlled Trial Study. Salmand: Iranian Journal of Ageing 2023; 18 (2) :162-177
URL: http://salmandj.uswr.ac.ir/article-1-2368-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2368-en.html
Jamileh Amirzadeh Iranagh *1 

 , Firouz Mohammadi2
, Firouz Mohammadi2 
 , Parviz Salem Safi2
, Parviz Salem Safi2 
 , Vahid Ayoughi2
, Vahid Ayoughi2 
 , Ali Sedghiani2
, Ali Sedghiani2 
 , Saeed Razi2
, Saeed Razi2 



 , Firouz Mohammadi2
, Firouz Mohammadi2 
 , Parviz Salem Safi2
, Parviz Salem Safi2 
 , Vahid Ayoughi2
, Vahid Ayoughi2 
 , Ali Sedghiani2
, Ali Sedghiani2 
 , Saeed Razi2
, Saeed Razi2 

1- Social Factors of Health Research Center, Faculty of Health, Urmia University of Medical Sciences, Urmia, Iran. , jamileh.amirzadeh@gmail.com
2- Social Factors of Health Research Center, Faculty of Health, Urmia University of Medical Sciences, Urmia, Iran.
2- Social Factors of Health Research Center, Faculty of Health, Urmia University of Medical Sciences, Urmia, Iran.
Full-Text [PDF 6042 kb]
(2371 Downloads)
| Abstract (HTML) (5142 Views)
Full-Text: (2127 Views)
Introduction
Epidemiological studies have shown that 40-57% of the elderly face sleep problems [1] and, to deal with sleep disorders, they use sleeping pills, such that 39% of sleeping pills are used by people over 60 years old [2]. This is while these drugs relieve sleep disorders temporarily [3]. The use of anti-anxiety drugs and barbiturates can increase insomnia in the elderly by 50% [4]. Other disadvantages of these drugs are drug dependence, resistant to drugs, and the cost imposed on people. To deal with sleep disorders, experts suggest non-pharmacological methods that increase the interaction between mind and body and thus support sleep [5]. Among these methods, music therapy and sleep hygiene can be mentioned that can make it easier to fall asleep and avoid behaviors that interfere with sleep. This study aims to assess the effect of music therapy (MT) and sleep hygiene (SH) education on sleep disorders of the elderly in Urmia, Iran.
Methods
This is a randomized controlled clinical trial. For sampling, the city of Urmia was first divided into two parts, north and south, where there were 18 comprehensive health centers in the northern part and 8 in the southern part. Among these centers, 9 centers from the north and 4 centers from the south were randomly selected. After the screening and interview, based on the inclusion criteria, 150 seniors over 60 years of age were selected from comprehensive health centers and divided into three groups of SH+MT, SH, and control using the block randomization method. To measure their sleep quality, the standard Pittsburgh sleep quality index (PSQI) was used, which was completed by the participants or by the researcher on behalf of them [6, 7]. The education program consisted of 4 one-hour sessions about the knowledge of the stages of sleep, how to provide a suitable environment for sleep, avoiding cigarettes, tea, coffee, soda, hunger and complete satiety, and having a regular sleep schedule, which was provided separately to the intervention groups. In the first group, the participants, after receiving the SH education, received MT by listening to a selected Azeri music for one month for 30-45 minutes before going to bed. After collecting the data, it was entered into SPSS software, version 21. To describe the data, Mean±SD, frequency and percentage were used. To know the baseline difference in the qualitative variables among the three groups, chi-square test was used. Kolmogorov Smirnov test was used to check the normality of data distribution and then one-way ANOVA test was used to compare the seven dimensions of PSQI among the three groups. Due to the significance of ANOVA test results, Bonferroni post hoc test was used to perform pairwise comparisons. The significance level was set at 0.05.
Results
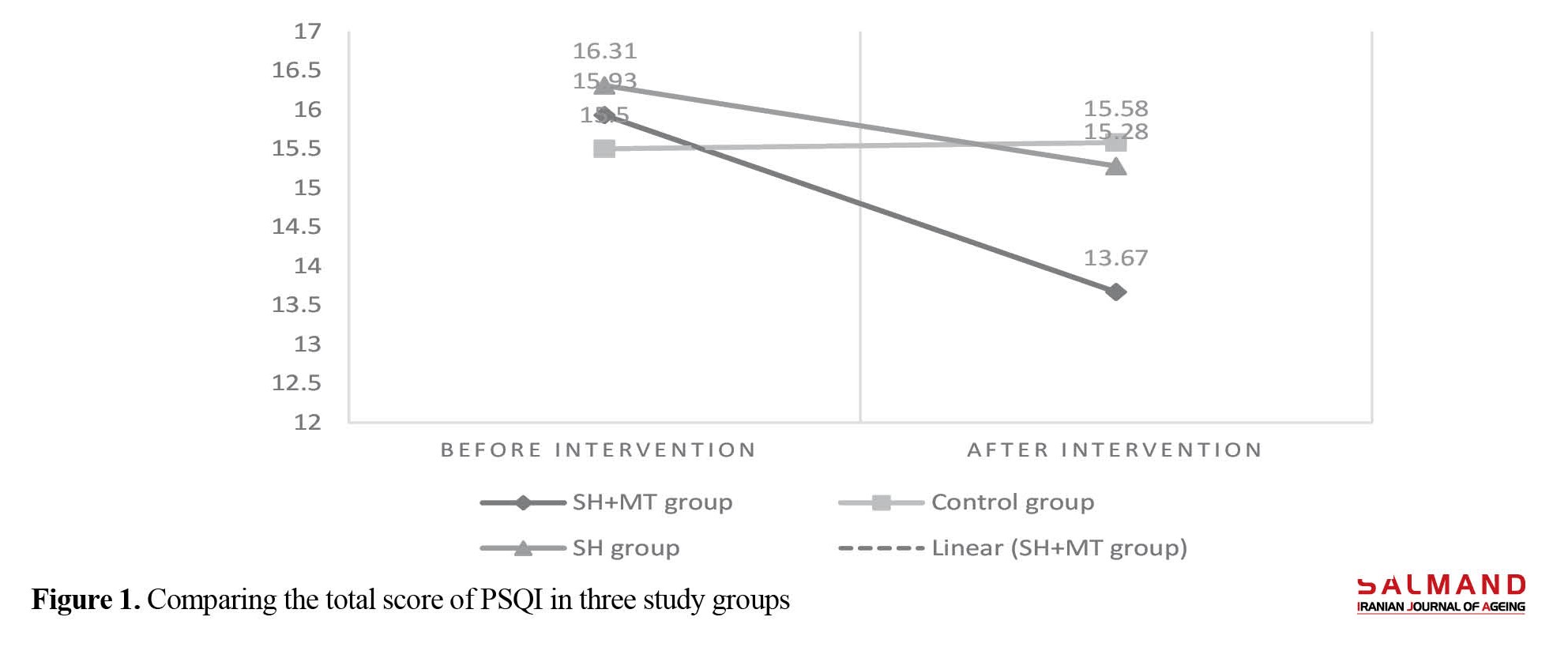
Of 150 participants, 74.80% were female. Their mean age was 64.39±5.23 years. Most of them (58.48 %) had lower than high school education, 59.84% were not employed, and 79.52% were living in their own houses. There was no statistically significant difference among the three groups in terms of age, educational level, occupation, marital status, and gender. During the study, 13 people from the SH+MT group and 11 from the SH group were excluded from the study. The comparison of PSQI dimensions showed that subjective sleep quality (F=14.34, P=0.0001), sleep latency (F=10.05, P=0.0001), sleep duration (F=21.91, P=0.0001), habitual sleep efficiency (F=24.98, P=0.0001), sleep disturbances (F=15.37, P=0.0001), use of sleep medication (F=1.840, P=0.04) and daytime drowsiness (F=1.181, P=0.02) were significantly different among the three groups. As can be seen in Figure 1, before the intervention, the mean total score of PSQI was 15.93±3.13 in the SH+MT group and 16.31±2.57 in the SH group. After the intervention, they were significantly decreased to 13.67±2.24 and 15.28±3.57, respectively, which indicates the success of the intervention (P=0.001). In the control group, the score changed from 15.50±3.01 to 15.58±3.01 after the intervention, which is very low and negligible.
Conclusion
Non-invasive interventions such as MT and SH education can be suitable alternatives for treating sleep disorders in older adults. By teaching SH strategies, lifestyle and habits can be improved for better sleep. Insomnia and sleep quality can be improved by complementary methods, such as MT using songs suitable for each culture. Therefore, it is suggested that these methods be used as non-pharmacological treatment methods for older people with sleep disorders by caregivers in families and nursing homes.
Ethical Considerations
Compliance with ethical guidelines
This study was app=roved by the Urmia University of Medical Sciences (Code: IR.UMSU.REC.1396.180). It was explained to the older adults about the objectives of the research and assuring them of the confidentiality of their information, informed consent was obtained from all participants.
Funding
This study was funded by Urmia University of Medical Sciences.
Authors' contributions
Conceptualization: All author; Methodology: Jamileh Amirzadeh Iranagh, Firouz Mohammadi, Vahid Ayoughi: Saeed Razi; Supervision: Jamileh Amirzadeh Iranagh, Parviz Salem Safi, Vahid Ayoughi and Ali Sedghiani.Investigation: Jamileh Amirzadeh Iranagh, Firouz Mohammadi, Vahid Ayoughi and Parviz Salem Safi; Writing–original draft, writing–review & editing, funding acquisition, resources: Jamileh Amirzadeh Iranagh.
Conflicts of interest
The authors declared no conflict of interest.
References
Epidemiological studies have shown that 40-57% of the elderly face sleep problems [1] and, to deal with sleep disorders, they use sleeping pills, such that 39% of sleeping pills are used by people over 60 years old [2]. This is while these drugs relieve sleep disorders temporarily [3]. The use of anti-anxiety drugs and barbiturates can increase insomnia in the elderly by 50% [4]. Other disadvantages of these drugs are drug dependence, resistant to drugs, and the cost imposed on people. To deal with sleep disorders, experts suggest non-pharmacological methods that increase the interaction between mind and body and thus support sleep [5]. Among these methods, music therapy and sleep hygiene can be mentioned that can make it easier to fall asleep and avoid behaviors that interfere with sleep. This study aims to assess the effect of music therapy (MT) and sleep hygiene (SH) education on sleep disorders of the elderly in Urmia, Iran.
Methods
This is a randomized controlled clinical trial. For sampling, the city of Urmia was first divided into two parts, north and south, where there were 18 comprehensive health centers in the northern part and 8 in the southern part. Among these centers, 9 centers from the north and 4 centers from the south were randomly selected. After the screening and interview, based on the inclusion criteria, 150 seniors over 60 years of age were selected from comprehensive health centers and divided into three groups of SH+MT, SH, and control using the block randomization method. To measure their sleep quality, the standard Pittsburgh sleep quality index (PSQI) was used, which was completed by the participants or by the researcher on behalf of them [6, 7]. The education program consisted of 4 one-hour sessions about the knowledge of the stages of sleep, how to provide a suitable environment for sleep, avoiding cigarettes, tea, coffee, soda, hunger and complete satiety, and having a regular sleep schedule, which was provided separately to the intervention groups. In the first group, the participants, after receiving the SH education, received MT by listening to a selected Azeri music for one month for 30-45 minutes before going to bed. After collecting the data, it was entered into SPSS software, version 21. To describe the data, Mean±SD, frequency and percentage were used. To know the baseline difference in the qualitative variables among the three groups, chi-square test was used. Kolmogorov Smirnov test was used to check the normality of data distribution and then one-way ANOVA test was used to compare the seven dimensions of PSQI among the three groups. Due to the significance of ANOVA test results, Bonferroni post hoc test was used to perform pairwise comparisons. The significance level was set at 0.05.
Results
Of 150 participants, 74.80% were female. Their mean age was 64.39±5.23 years. Most of them (58.48 %) had lower than high school education, 59.84% were not employed, and 79.52% were living in their own houses. There was no statistically significant difference among the three groups in terms of age, educational level, occupation, marital status, and gender. During the study, 13 people from the SH+MT group and 11 from the SH group were excluded from the study. The comparison of PSQI dimensions showed that subjective sleep quality (F=14.34, P=0.0001), sleep latency (F=10.05, P=0.0001), sleep duration (F=21.91, P=0.0001), habitual sleep efficiency (F=24.98, P=0.0001), sleep disturbances (F=15.37, P=0.0001), use of sleep medication (F=1.840, P=0.04) and daytime drowsiness (F=1.181, P=0.02) were significantly different among the three groups. As can be seen in Figure 1, before the intervention, the mean total score of PSQI was 15.93±3.13 in the SH+MT group and 16.31±2.57 in the SH group. After the intervention, they were significantly decreased to 13.67±2.24 and 15.28±3.57, respectively, which indicates the success of the intervention (P=0.001). In the control group, the score changed from 15.50±3.01 to 15.58±3.01 after the intervention, which is very low and negligible.
Conclusion
Non-invasive interventions such as MT and SH education can be suitable alternatives for treating sleep disorders in older adults. By teaching SH strategies, lifestyle and habits can be improved for better sleep. Insomnia and sleep quality can be improved by complementary methods, such as MT using songs suitable for each culture. Therefore, it is suggested that these methods be used as non-pharmacological treatment methods for older people with sleep disorders by caregivers in families and nursing homes.
Ethical Considerations
Compliance with ethical guidelines
This study was app=roved by the Urmia University of Medical Sciences (Code: IR.UMSU.REC.1396.180). It was explained to the older adults about the objectives of the research and assuring them of the confidentiality of their information, informed consent was obtained from all participants.
Funding
This study was funded by Urmia University of Medical Sciences.
Authors' contributions
Conceptualization: All author; Methodology: Jamileh Amirzadeh Iranagh, Firouz Mohammadi, Vahid Ayoughi: Saeed Razi; Supervision: Jamileh Amirzadeh Iranagh, Parviz Salem Safi, Vahid Ayoughi and Ali Sedghiani.Investigation: Jamileh Amirzadeh Iranagh, Firouz Mohammadi, Vahid Ayoughi and Parviz Salem Safi; Writing–original draft, writing–review & editing, funding acquisition, resources: Jamileh Amirzadeh Iranagh.
Conflicts of interest
The authors declared no conflict of interest.
References
- Albou Kordi M, Ramezani M, Arizi F. [A study on the quality of life among elderly Shahinshahr area of Isfahan province in year 2004 (Persian)]. Jundishapur Scientific Medical Journal. 2007; 5(4):7-1-7. [Link]
- Donmez L, Gokkoca Z, Dedeoglu N. Disability and its effects on quality of life among older people living in Antalya city center, Turkey. Archives of Gerontology and Geriatrics. 2005; 40(2):213-23. [DOI:10.1016/j.archger.2004.08.006] [PMID]
- Tonn B, Eisenberg J. The aging US population and residential energy demand. Energy Policy. 2007; 35(1):743-5. [DOI:10.1016/j.enpol.2005.12.011]
- Hashemi Siyavoshani M, Fallahi Arezodar F, Pishgooei SA, Jadid_Milani M. [The effect of rose water on the anxiety level of aged admitted to cardiac intensive care units (Persian)]. Iranian Journal of Nursing Research. 2020; 15(1):59-68. [Link]
- Heidari M, Shahbazi S. [Effect of self-care training program on quality of life of elders (Persian)]. Iran Journal of Nursing. 2012; 25(75):1-8. [Link]
- Alizadeh M, Hoseini M, Shojaeizadeh D, Rahimi A, Arshinchi M, Rohani H. [Assessing anxiety, depression and psychological wellbeing status of urban elderly under represent of Tehran Metropolitan City (Persian)] . Iranian Journal of Aging. 2012; 7(3):66-73. [Link]
- Abbasi A, Bahrami H, Beygi B, Musa Farkhani E, Vakili V, Rezaee Talab F, et al. [Risk factors of sleep disorders in elderly: A population-based case-control study (Persian)]. Iranian Journal of Epidemiology. 2019; 15(2):172-8. [Link]
- Ohayon MM. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Medicine Reviews. 2002; 6(2):97-111. [DOI:10.1053/smrv.2002.0186] [PMID]
- Morin CM, LeBlanc M, Daley M, Gregoire JP, Mérette C. Epidemiology of insomnia: Prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Medicine. 2006; 7(2):123-30. [DOI:10.1016/j.sleep.2005.08.008] [PMID]
- Aminnia N, Aghaei A, Molavi H, Najafi MR. [The effectiveness of group cognitive therapy on symptoms of insomnia in women with chronic insomnia (Persian)]. Knowledge & Research in Applied Psychology. 2011; 12(2):13-19. [Link]
- Krishnan P, Hawranik P. Diagnosis and management of geriatric insomnia: A guide for nurse practitioners. Journal of the American Academy of Nurse Practitioners. 2008; 20(12):590-9. [DOI:10.1111/j.1745-7599.2008.00366.x] [PMID]
- Ancoll-Israel S. Sleep disorders in older adults. A primary care guide to assessing 4 common sleep problems in geriatric patients. Geriatrics. 2004; 59(1):37-40. [PMID]
- Harrington JJ, Avidan AY. Treatment of sleep disorders in elderly patients. Current Treatment Options in Neurology. 2005; 7(5):339-52. [DOI:10.1007/s11940-005-0027-x] [PMID]
- Nobahar M, Vafaee AA. [Assessment of elderlies sleep disorders and different confronts methods among them (Persian)]. Iranian Journal of Ageing. 2007; 2(2):263-8. [Link]
- Montgomery P. Treatments for sleep problems in elderly people. BMJ. 2002; 325(7372):1049. [DOI:10.1136/bmj.325.7372.1049] [PMID] [PMCID]
- Ford DE, Cooper‐Patrick L. Sleep disturbances and mood disorders: An epidemiologic perspective. Depression and Anxiety. 2001; 14(1):3-6. [DOI:10.1002/da.1041] [PMID]
- Kozasa EH, Hachul H, Monson C, Pinto L Jr, Garcia MC, Mello LE, et al. Mind-body interventions for the treatment of insomnia: A review. Revista Brasileira de Psiquiatria. 2010; 32(4):437-43. [DOI:10.1590/S1516-44462010000400018] [PMID]
- Baghaei R, Moradi Y. [The Effect of sleep hygiene education on sleep quality of patients with heart failure hospitalized in cardiac care units of urmia teaching hospitals 2017-2018 (Persian)]. Nursing and Midwifery Journal. 2019; 17(9):674-89. [Link]
- Taheri Tanjani P, Khodabakhshi H, Etemad K, Mohammadi M. [Effect of sleep hygiene education on sleep quality and general health of elderly women with sleep disorders living in Birjand City, Iran, in 2016 (Persian)]. Salmand: Iranian Journal of Ageing. 2019; 14(2):248-59. [Link]
- Moradi M, Mohammadzadeh H, Noori R, Basiri Moghadam K, Sadeghmoghadam L. [Effect of a sleep hygiene education program using telephone follow-up method on the sleep quality of the elderly (Persian)]. Iranian Journal of Ageing. 2021; 15(4):484- 95. [DOI:10.32598/sija.15.4.2895.1]
- Chang ET, Lai HL, Chen PW, Hsieh YM, Lee LH. The effects of music on the sleep quality of adults with chronic insomnia using evidence from polysomnographic and self-reported analysis: A randomized control trial. International Journal of Nursing Studies. 2012; 49(8):921-30. [DOI:10.1016/j.ijnurstu.2012.02.019] [PMID]
- Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database of Systematic Reviews. 2006; 2(2). [DOI:10.1002/14651858.CD004843.pub2]
- Lai HL, Good M. Music improves sleep quality in older adults. Journal of Advanced Nursing. 2005; 49(3):234-44. [DOI:10.1111/j.1365-2648.2004.03281.x] [PMID]
- Cruise CJ, Chung F, Yogendran S, Little D. Music increases satisfaction in elderly outpatients undergoing cataract surgery. Canadian Journal of Anaesthesia. 1997; 44(1):43-8. [DOI:10.1007/BF03014323] [PMID]
- Winter MJ, Paskin S, Baker T. Music reduces stress and anxiety of patients in the surgical holding area. Journal of Post Anesthesia Nursing. 1994; 9(6):340-3. [PMID]
- Nilsson U. Music: A nursing intervention. European Journal of Cardiovascular Nursing. 2011; 10(2):73-4. [DOI:10.1016/j.ejcnurse.2010.06.004] [PMID]
- Nilsson J, Parker MG, Kabir ZN. Assessing health -related quality of life among older people in rural Bangladesh. Jornal of Trans Cultural Nursing. 2004; 15(4):298-307. [DOI:10.1177/1043659604268968] [PMID]
- Nilsson U. The anxiety-and pain-reducing effects of music interventions: A systematic review. AORN Journal. 2008; 87(4):780-807. [DOI:10.1016/j.aorn.2007.09.013] [PMID]
- de Niet G, Tiemens B, Lendemeijer B, Hutschemaekers G. Music‐assisted relaxation to improve sleep quality: Meta‐analysis. Journal of Advanced Nursing. 2009; 65(7):1356-64. [DOI:10.1111/j.1365-2648.2009.04982.x] [PMID]
- Möckel M, Röcker L, Störk T, Vollert J, Danne O, Eichstädt H, et al. Immediate physiological responses of healthy volunteers to different types of music: Cardiovascular, hormonal and mental changes. European Journal of Applied Physiology and Occupational Physiology. 1994; 68(6):451-9. [DOI:10.1007/BF00599512] [PMID]
- Lindquist R, Snyder M, Tracy MF. Complementary & alternative therapies in Nursing. New York: Springer Publishing Company; 2013. [DOI:10.1891/9780826196347]
- Lai HL, Hwang MJ, Chen CJ, Chang KF, Peng TC, Chang FM. Randomised controlled trial of music on state anxiety and physiological indices in patients undergoing root canal treatment. Journal of Clinical Nursing. 2008; 17(19):2654-60. [DOI:10.1111/j.1365-2702.2008.02350.x] [PMID]
- Lai HL, Li YM. The effect of music on biochemical markers and self‐perceived stress among first‐line nurses: A randomized controlled crossover trial. Journal of Advanced Nursing. 2011; 67(11):2414-24. [DOI:10.1111/j.1365-2648.2011.05670.x] [PMID]
- Ventura T, Gomes M, Carreira T. Cortisol and anxiety response to a relaxing intervention on pregnant women awaiting amniocentesis. Psychoneuroendocrinology. 2012; 37(1):148-56. [DOI:10.1016/j.psyneuen.2011.05.016] [PMID]
- Harmat L, Takács J, Bodizs R. Music improves sleep quality in students. Journal of Advanced Nursing. 2008; 62(3):327-35. [DOI:10.1111/j.1365-2648.2008.04602.x] [PMID]
- Standley JM. Music research in medical/dental treatment: Meta-analysis and clinical applications. Journal of Music Therapy. 1986; 23(2):56-122. [DOI:10.1093/jmt/23.2.56] [PMID]
- Abbasi Tadi S, Saberi M, Akbari H. [Effect of acupressure at ShenMen acupoint on the sleep quality of nurses in emergency departments and intensive care units (Persian)]. Complementary Medicine Journal. 2021; 10(4):380-95. [Link]
- Allami Z, khankeh H, Dalvandi A, Ali Zademohammai M, Rezasoltani P. [Effect of music-therapy on quality of sleep among elderly male of the Isfahan city petroleum’s Retirement Association 2012 (Persian)]. Journal of Geriatric Nursing. 2014; 1(1):55-63. [Link]
- Majedi H, Shamlou Kia S. [The impression of nature & environment on Iranian music (Persian)]. Journal of Environmental Science and Technology. 2011; 13(2):93-102. [Link]
- Wishlaqi J. [Examining the types of poems of Azerbaijani local musicians (Persian)]. Culture of the Iranian People. 2007; 10:139-64. [Link]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989; 28(2):193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Mottaghi R, Maredpour A, Karamin S. [A comparison study on the effectiveness of acceptance and commitment therapy and sleep hygiene education on sleep quality and physiological parameters in older adults (Persian)]. Salmand: Iranian Journal of Ageing. 2022; 17(2):170-85. [Link]
- Farrahi J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Psychometric properties of the Persian version of the Pittsburgh Sleep Quality Index addendum for PTSD (PSQI-A). Sleep & Breathing = Schlaf & Atmung. 2009; 13(3):259-62. [DOI:10.1007/s11325-008-0233-3] [PMID]
- Thichumpa W, Howteerakul N, Suwannapong N, Tantrakul V. Sleep quality and associated factors among the elderly living in rural Chiang Rai, northern Thailand. Epidemiology and Health. 2018; 40:e2018018-e. [DOI:10.4178/epih.e2018018] [PMID] [PMCID]
- Wang P, Song L, Wang K, Han X, Cong L, Wang Y, et al. Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area: A population-based study. Aging Clinical and Experimental Research. 2020; 32(1):125-31. [DOI:10.1007/s40520-019-01171-0] [PMID] [PMCID]
- Zhang HS, Li Y, Mo HY, Qiu DX, Zhao J, Luo JL, et al. A community-based cross-sectional study of sleep quality in middle-aged and older adults. Quality of Life Research. 2017; 26(4):923-33. [DOI:10.1007/s11136-016-1408-1] [PMID]
- Kalleinen N, Polo O, Himanen SL, Joutsen A, Urrila AS, Polo-Kantola P. Sleep deprivation and hormone therapy in postmenopausal women. Sleep Medicine. 2006; 7(5):436-47. [DOI:10.1016/j.sleep.2006.02.004] [PMID]
- Izadi Avanji FS, Adib Hajbaghery M, Afazel MR. [Quality of sleep and it’s related factors in the hospitalized elderly patients of Kashan hospitals in 2007 (Persian)]. KAUMS Journal (FEYZ). 2009; 12(4):52-60. [Link]
- Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. Journal of Thoracic Disease. 2015; 7(8):1311-22. [PMID]
- Luo J, Zhu G, Zhao Q, Guo Q, Meng H, Hong Z, et al. Prevalence and risk factors of poor sleep quality among Chinese elderly in an urban community: Results from the Shanghai aging study. Plos One. 2013; 8(11):e81261. [DOI:10.1371/journal.pone.0081261] [PMID] [PMCID]
- Friedman EM, Love GD, Rosenkranz MA, Urry HL, Davidson RJ, Singer BH, et al. Socioeconomic status predicts objective and subjective sleep quality in aging women. Psychosomatic Medicine. 2007; 69(7):682-91. [DOI:10.1097/PSY.0b013e31814ceada] [PMID]
- Arasteh M, Yousefi F, Sharifi Z. [Investigation of sleep quality and its influencing factors in patients admitted to the gynecology and general surgery of besat hospital in sanandaj (Persian)]. Medical Journal of Mashhad University of Medical Sciences. 2014; 57(6):762-9. [Link]
- Hosseini SR, Saadat P, Esmaili M, Bijani A. The prevalence of self-reported sleep problems and some factors affecting it among the elderly in Amirkola. Shiraz E-Medical Journal. 2018; 19(3):e59461 [DOI:10.5812/semj.59461]
- Mirzaei M, Gholamrezaei E, Bidaki R, Fallahzadeh H, Ravaei J. [Quality of sleep and methods of management of sleep disorders in elderly of Yazd city in 2016 (Persian)]. Journal of Shahid Sadoughi University of Medical Sciences. 2017; 25(6):467-75. [Link]
- Torabi S, Shahriari L, Zahedi R, Rahmanian S, Rahmanian K. A survey the prevalence of sleep disorders and their management in the elderly in Jahrom City, 2008. Journal of Jahrom University of Medical Sciences. 2013; 10(4):31. [Link]
- Wong WS, Fielding R. Prevalence of insomnia among Chinese adults in Hong Kong: A population‐based study. Journal of Sleep Research. 2011; 20(1pt1):117-26. [DOI:10.1111/j.1365-2869.2010.00822.x] [PMID]
- Rezaei B, Shooshtarizadeh S. [Factors related to sleep quality among elderly residing at Isfahan nursing homes (Persian)]. Iranian Journal of Geriatric Nursing. 2016; 2(2):37-49. [Link]
- Kor A, Muosavi S, Reza Masouleh S, Behnam Puor N. [Assessment of the correlation between lifestyle and quality of sleep in elderly who referred to retirement center in Rasht, 2007 (Persian)]. Journal of Holistic Nursing and Midwifery. 2007; 17(2):15-22. [Link]
- JinJu S, HyunWoo J. The effects of sleep hygiene program on sleep quality in the elderly women. Indian Journal of Science and Technology. 2016; 9(37):1-7. [DOI:10.17485/ijst/2016/v9i37/102541]
- Chen PH, Kuo HY, Chueh KH. Sleep hygiene education: Efficacy on sleep quality in working women. Journal of Nursing Research. 2010; 18(4):283-9. [DOI:10.1097/JNR.0b013e3181fbe3fd] [PMID]
- Khodabakhshi-Koolaee A, Zahmatkesh M, Barzeghar Khezri R. [The effect of relaxation and instrumental music by arnd stein on quality of sleep and happiness among ageing women (Persian)]. Journal of Torbat Heydariyeh University of Medical Sciences. 2018; 5(4):46 -53. [Link]
- Lai HL. Music preference and relaxation in Taiwanese elderly people. Geriatric Nursing. 2004; 25(5):286-91. [DOI:10.1016/j.gerinurse.2004.08.009] [PMID]
- Wang CF, Sun YL, Zang HX. Music therapy improves sleep quality in acute and chronic sleep disorders: A meta-analysis of 10 randomized studies. International Journal of Nursing Studies. 2014; 51(1):51-62. [DOI:10.1016/j.ijnurstu.2013.03.008] [PMID]
- Allami Z, Dalvandi A, Rezasoltani P. [Effect of music-therapy on quality of sleep among elderly male of the Isfahan city petroleum’s Retirement Association 2012 (Persian)]. Journal of Geriatric Nursing. 2014; 1(1):55-63. [Link]
- Feng F, Zhang Y, Hou J, Cai J, Jiang Q, Li X, et al. Can music improve sleep quality in adults with primary insomnia? A systematic review and network meta-analysis. International Journal of Nursing Studies. 2018; 77:189-96. [DOI:10.1016/j.ijnurstu.2017.10.011] [PMID]
- Huang CY, Chang ET, Hsieh YM, Lai HL. Effects of music and music video interventions on sleep quality: A randomized controlled trial in adults with sleep disturbances. Complementary Therapies in Medicine. 2017; 34:116-22. [DOI:10.1016/j.ctim.2017.08.015] [PMID]
- Chan MF, Chan EA, Mok E. Effects of music on depression and sleep quality in elderly people: A randomised controlled trial. Complementary Therapies in Medicine. 2010; 18(3):150-9. [DOI:10.1016/j.ctim.2010.02.004] [PMID]
Type of Study: Research |
Subject:
gerontology
Received: 2021/12/07 | Accepted: 2022/05/15 | Published: 2023/07/01
Received: 2021/12/07 | Accepted: 2022/05/15 | Published: 2023/07/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |