Volume 18, Issue 2 (Summer 2023)
Salmand: Iranian Journal of Ageing 2023, 18(2): 284-303 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rahmani F, Marsa R, Khanjani M S, Marsa S, Shahrivar K. Recognition Discriminability and Response Bias in the Shiraz Verbal Learning Test Among Older People With Amnestic Mild Cognitive Impairment, Alzheimer's Disease, and Memory Normal. Salmand: Iranian Journal of Ageing 2023; 18 (2) :284-303
URL: http://salmandj.uswr.ac.ir/article-1-2392-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2392-en.html
1- Department of Counseling, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Student Research Committee, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,r_marsa@yahoo.com
3- Department of Psychology and Education of Exceptional Children, Faculty of Humanities and Social Sciences, Science and Research Branch, Islamic Azad University, Tehran, Iran.
4- Department of Medicine, School of Medicine, Jahrom University of Medical Science, Jahrom, Iran.
2- Student Research Committee, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Department of Psychology and Education of Exceptional Children, Faculty of Humanities and Social Sciences, Science and Research Branch, Islamic Azad University, Tehran, Iran.
4- Department of Medicine, School of Medicine, Jahrom University of Medical Science, Jahrom, Iran.
Keywords: Alzheimer’s disease, Amnesia, Mild cognitive impairment, Recognition memory, Shiraz verbal learning test, Elderly
Full-Text [PDF 7469 kb]
(1951 Downloads)
| Abstract (HTML) (4821 Views)
Full-Text: (1939 Views)
Introduction
Defect of memory is one of the most common cognitive disorders related to aging [1]. Until 1990, few studies investigated cognitive impairment in the stage before the diagnosis of Alzheimer’s disease, while subsequent studies focused on the pre-disease or prodromal stage of Alzheimer’s disease [2, 3]. The concept of mild cognitive impairment (MCI) has emerged significantly over the past two decades and is defined as the intermediate stage between the cognitive changes of normal aging and dementia. In the elderly with amnestic MCI, who are at risk of developing Alzheimer’s disease, the impaired ability to learn and remember new information, especially verbal episodic memory impairment, is one of the most important cognitive dimensions related to age that deteriorates at a faster rate [4, 5]. In 1987, Delis et al. added a recognition discriminability (RD) index to the first edition of the California verbal learning test (CVLT), where the hit rate is compared to the number of false-positive errors [3]. In addition, response bias (RB) index was added to the CVLT, which is related to the individual’s tendency to give “yes” or “no” answers, regardless of the type of stimulus. The Shiraz verbal learning test (SVLT), like this test, use the yes/no answering method (16 words from list A and 32 false-positive words) in the memory recognition part to measure the recognition discriminability index and response bias index [6, 7]. Since it seems that in-depth investigation of recognition memory patterns in healthy elderly and those with MCI can help in the early diagnosis of cognitive impairment and the onset of Alzheimer’s disease, the present study aims to compare the RD and RB in the SVLT between healthy elderly and those with amnestic MCI and Alzheimer’s disease.
Methods
This is a descriptive cross-sectional study that was conducted from May to December 2021. The sample were 190 older people ranged 60-89 years in three groups of Alzheimer’s disease (n=61), amnestic MCI (n=60), and healthy (n=59). The criteria for entering the elderly group with Alzheimer’s were the diagnosis of Alzheimer’s or cortical dementia (mild to moderate) based on MRI and the diagnostic and statistical manual of mental disorders (DSM-5) criteria, as well as neuropsychological tests, SVLT, and mini-mental status examination (MMSE), no psychiatric disorders such as major depressive disorder, no neurological diseases other than Alzheimer’s (such as Korsakoff’s and Huntington’s disease), and no aphasia. Those in the amnestic MCI groups were selected based on Patterson & Clarfield’s theory where the inclusion criteria are: Subjective memory complaint (score between -1 and -1.5 standard deviations from the mean in SVLT subscales), normal daily life activity, normal general cognitive function, abnormal memory function, no dementia (cortical or subcortical), no psychiatric disorders, and no aphasia.
Data collection tools were SVLT and MMSE. The SVLT has acceptable psychometric properties in Persian form. Rahmani et al. [8], examined its test-retest reliability on 183 healthy individuals and the results showed that the correlation was in the moderate-to-high range (29-94 in the main variables of the SVLT). In the SVLT, two indices are used derived from the “signal detection theory”, including RB and RD. The MMSE, which has a cut-off point of 21, a sensitivity of 90% and a specificity of 84% in Iranian population [21], is a tool to screen for cognitive disorders. In this study, descriptive statistics, one-way ANOVA, and Scheffe’s post hoc test were used to analyze the data in SPSS software, version 19.
Results
According to the results of one-way ANOVA, no significant difference was observed between the three groups in age and education (P=0.42 and P=0.21, respectively). In terms of cognitive performance, the results of MMSE showed that patients with Alzheimer’s disease and amnestic MCI had significantly lower performance (P<0.001) than healthy older people. The Mean±SD of RD domains (general, semantic, source, and new) in Table 1 showed that the healthy group had higher scores compared to the two groups of Alzheimer’s and amnestic MCI, and they were able to discriminate more correctly in all RD domains (P<0.001).
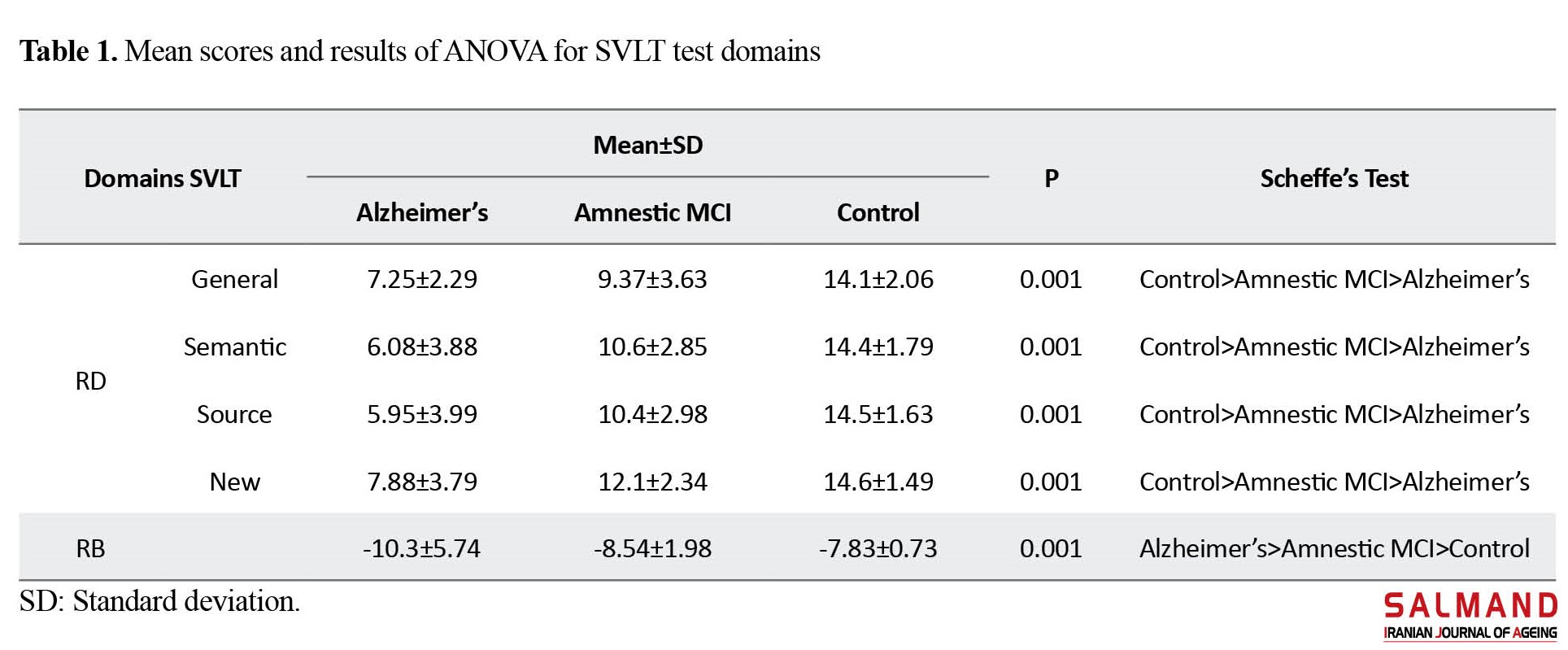
The results of Scheffe’s post hoc test also showed that there was a significant difference between all pairs of groups (P<0.001). Table 1 shows the Mean±SD of the RB variable for the three groups. The results of one-way ANOVA showed a significant difference among the three groups (P<0.001). The results of Scheffe’s post hoc test showed a significant difference between the Alzheimer’s group compared to the healthy group and amnestic MCI group (P<0.001), but there was no significant difference between the amnestic MCI and healthy groups.
Conclusion
There is an impaired recognition memory in Alzheimer’s disease and amnestic MCI. The SVLT, by evaluating the recognition memory performance, can be used to screen people with Alzheimer’s disease and amnestic MCI before the clinical stages are fully revealed.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1400.140)
Funding
This work was supported financially by the Student Research Committee of the University of Social Welfare and Rehabilitation Sciences (Grant No.: 2625).
Authors' contributions
The authors equally contributed in the preparation of this article.
Conflicts of interest
The authors declared no conflict of interest.
References
Defect of memory is one of the most common cognitive disorders related to aging [1]. Until 1990, few studies investigated cognitive impairment in the stage before the diagnosis of Alzheimer’s disease, while subsequent studies focused on the pre-disease or prodromal stage of Alzheimer’s disease [2, 3]. The concept of mild cognitive impairment (MCI) has emerged significantly over the past two decades and is defined as the intermediate stage between the cognitive changes of normal aging and dementia. In the elderly with amnestic MCI, who are at risk of developing Alzheimer’s disease, the impaired ability to learn and remember new information, especially verbal episodic memory impairment, is one of the most important cognitive dimensions related to age that deteriorates at a faster rate [4, 5]. In 1987, Delis et al. added a recognition discriminability (RD) index to the first edition of the California verbal learning test (CVLT), where the hit rate is compared to the number of false-positive errors [3]. In addition, response bias (RB) index was added to the CVLT, which is related to the individual’s tendency to give “yes” or “no” answers, regardless of the type of stimulus. The Shiraz verbal learning test (SVLT), like this test, use the yes/no answering method (16 words from list A and 32 false-positive words) in the memory recognition part to measure the recognition discriminability index and response bias index [6, 7]. Since it seems that in-depth investigation of recognition memory patterns in healthy elderly and those with MCI can help in the early diagnosis of cognitive impairment and the onset of Alzheimer’s disease, the present study aims to compare the RD and RB in the SVLT between healthy elderly and those with amnestic MCI and Alzheimer’s disease.
Methods
This is a descriptive cross-sectional study that was conducted from May to December 2021. The sample were 190 older people ranged 60-89 years in three groups of Alzheimer’s disease (n=61), amnestic MCI (n=60), and healthy (n=59). The criteria for entering the elderly group with Alzheimer’s were the diagnosis of Alzheimer’s or cortical dementia (mild to moderate) based on MRI and the diagnostic and statistical manual of mental disorders (DSM-5) criteria, as well as neuropsychological tests, SVLT, and mini-mental status examination (MMSE), no psychiatric disorders such as major depressive disorder, no neurological diseases other than Alzheimer’s (such as Korsakoff’s and Huntington’s disease), and no aphasia. Those in the amnestic MCI groups were selected based on Patterson & Clarfield’s theory where the inclusion criteria are: Subjective memory complaint (score between -1 and -1.5 standard deviations from the mean in SVLT subscales), normal daily life activity, normal general cognitive function, abnormal memory function, no dementia (cortical or subcortical), no psychiatric disorders, and no aphasia.
Data collection tools were SVLT and MMSE. The SVLT has acceptable psychometric properties in Persian form. Rahmani et al. [8], examined its test-retest reliability on 183 healthy individuals and the results showed that the correlation was in the moderate-to-high range (29-94 in the main variables of the SVLT). In the SVLT, two indices are used derived from the “signal detection theory”, including RB and RD. The MMSE, which has a cut-off point of 21, a sensitivity of 90% and a specificity of 84% in Iranian population [21], is a tool to screen for cognitive disorders. In this study, descriptive statistics, one-way ANOVA, and Scheffe’s post hoc test were used to analyze the data in SPSS software, version 19.
Results
According to the results of one-way ANOVA, no significant difference was observed between the three groups in age and education (P=0.42 and P=0.21, respectively). In terms of cognitive performance, the results of MMSE showed that patients with Alzheimer’s disease and amnestic MCI had significantly lower performance (P<0.001) than healthy older people. The Mean±SD of RD domains (general, semantic, source, and new) in Table 1 showed that the healthy group had higher scores compared to the two groups of Alzheimer’s and amnestic MCI, and they were able to discriminate more correctly in all RD domains (P<0.001).
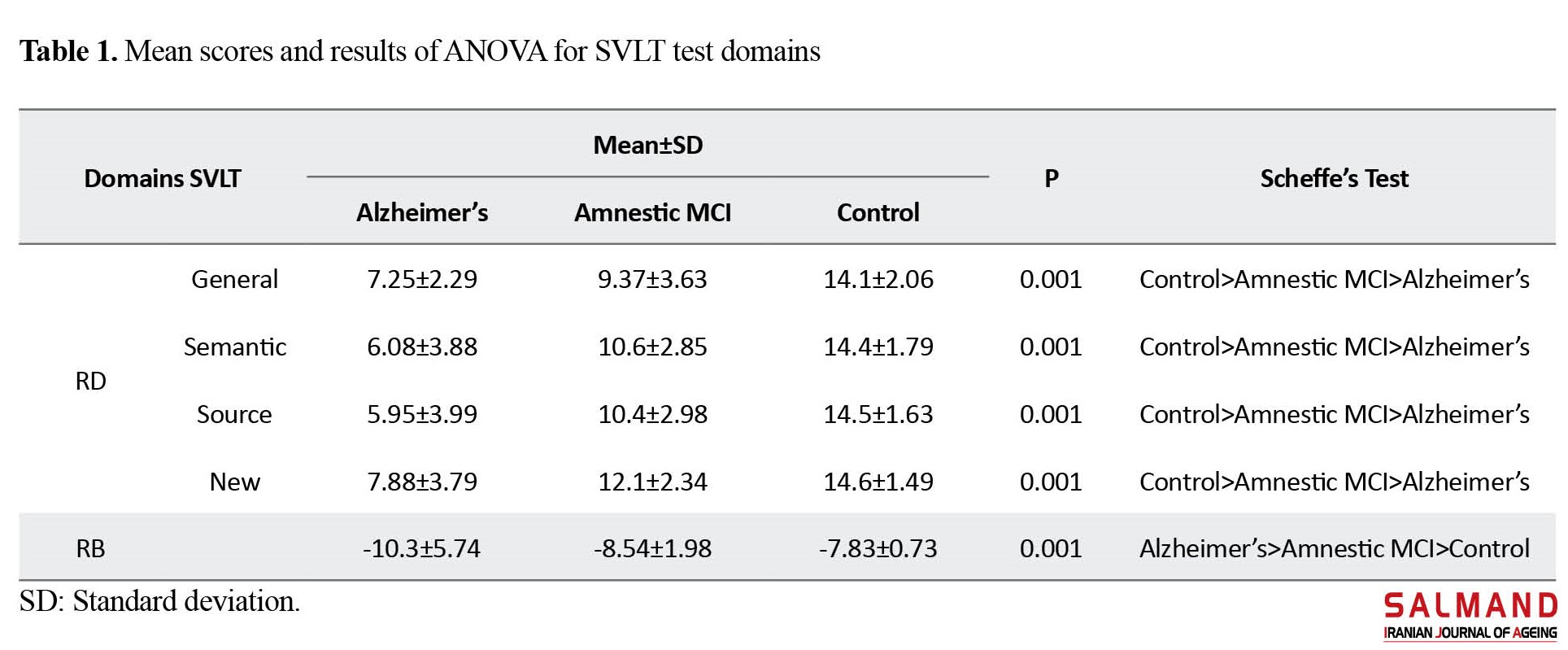
The results of Scheffe’s post hoc test also showed that there was a significant difference between all pairs of groups (P<0.001). Table 1 shows the Mean±SD of the RB variable for the three groups. The results of one-way ANOVA showed a significant difference among the three groups (P<0.001). The results of Scheffe’s post hoc test showed a significant difference between the Alzheimer’s group compared to the healthy group and amnestic MCI group (P<0.001), but there was no significant difference between the amnestic MCI and healthy groups.
Conclusion
There is an impaired recognition memory in Alzheimer’s disease and amnestic MCI. The SVLT, by evaluating the recognition memory performance, can be used to screen people with Alzheimer’s disease and amnestic MCI before the clinical stages are fully revealed.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1400.140)
Funding
This work was supported financially by the Student Research Committee of the University of Social Welfare and Rehabilitation Sciences (Grant No.: 2625).
Authors' contributions
The authors equally contributed in the preparation of this article.
Conflicts of interest
The authors declared no conflict of interest.
References
- Mooldijk SS, Yaqub A, Wolters FJ, Licher S, Koudstaal PJ, Ikram MK, et al. Life expectancy with and without dementia in persons with mild cognitive impairment in the community. Journal of the American Geriatrics Society. 2022; 70(2):481-9. [DOI:10.1111/jgs.17520] [PMID] [PMCID]
- Bondi MW, Edmonds EC, Salmon DP. Alzheimer’s Disease: Past, present, and future. Journal of the International Neuropsychological Society: JINS. 2017; 23(9-10):818-31. [DOI:10.1017/S135561771700100X] [PMID] [PMCID]
- Delis DC, Kramer JH, Kaplan E, Ober BA. California verbal learning test-Second Edition. San Antonia, TX: The Psychological Corporation. 2000. [Link]
- Bessi V, Mazzeo S, Padiglioni S, Piccini C, Nacmias B, Sorbi S, et al. From subjective cognitive decline to alzheimer’s disease: The predictive role of neuropsychological assessment, personality traits, and cognitive reserve. A 7-year follow-up study. Journal of Alzheimer’s Disease : JAD. 2018; 63(4):1523-35. [DOI:10.3233/JAD-171180] [PMID]
- Russo MJ, Campos J, Vázquez S, Sevlever G, Allegri RF, Weiner MW, et al. Adding recognition discriminability index to the delayed recall is usefulto predict conversion from mild cognitive impairment to Alzheimer’s disease in the Alzheimer’s disease neuroimaging initiative. Frontiers in Aging Neuroscience. 2017; 9:46. [DOI:10.3389/fnagi.2017.00046] [PMID] [PMCID]
- Campos-Magdaleno M, Facal D, Lojo-Seoane C, Pereiro AX, Juncos-Rabadán O. Longitudinal assessment of verbal learning and memory in amnestic mild cognitive impairment: Practice effects and meaningful changes. Frontiers in Psychology. 2017; 8:1231. [DOI:10.3389/fpsyg.2017.01231] [PMID] [PMCID]
- Greenaway MC, Lacritz LH, Binegar D, Weiner MF, Lipton A, Munro Cullum C. Patterns of verbal memory performance in mild cognitive impairment, Alzheimer disease, and normal aging. Cognitive and Behavioral Neurology. 2006; 19(2):79-84. [DOI:10.1097/01.wnn.0000208290.57370.a3] [PMID]
- Clark LR, Stricker NH, Libon DJ, Delano-Wood L, Salmon DP, Delis DC, et al. Yes/no versus forced-choice recognition memory in mild cognitive impairment and Alzheimer’s disease: Patterns of impairment and associations with dementia severity. The Clinical Neuropsychologist. 2012; 26(7):1201-16. [DOI:10.1080/13854046.2012.728626] [PMID] [PMCID]
- García-Herranz S, Díaz-Mardomingo MC, Peraita H. Neuropsychological predictors of conversion to probable Alzheimer disease in elderly with mild cognitive impairment. Journal of Neuropsychology. 2016; 10(2):239-55. [DOI:10.1111/jnp.12067] [PMID]
- Rahmani F, Khanjani MS, Marsa R, Sharifi G, Bahadori E, Sarani EM. Learning strategies and verbal memory deficits on the Shiraz verbal learning test in patients with alzheimer’s disease and amnestic mild cognitive impairment. Iranian Journal of Psychiatry and Behavioral Sciences. 2022 ; 16(2):e118139. [Link]
- De Simone MS, Perri R, Fadda L, Caltagirone C, Carlesimo GA. Predicting progression to Alzheimer’s disease in subjects with amnestic mild cognitive impairment using performance on recall and recognition tests. Journal of Neurology. 2019; 266(1):102-11. [DOI:10.1007/s00415-018-9108-0] [PMID]
- Rudebeck S. The human medial temporal lobe, brain connectivity, and recognition memory[PhD dissertation]. Oxford: University of Oxford; 2012. [Link]
- Fine EM, Delis DC, Wetter SR, Jacobson MW, Hamilton JM, Peavy G, et al. Identifying the “source” of recognition memory deficits in patients with Huntington’s disease or Alzheimer’s disease: Evidencefrom the CVLT-II. Journal of Clinical and Experimental Neuropsychology. 2008; 30(4):463-70. [DOI:10.1080/13803390701531912] [PMID] [PMCID]
- Graves LV. Modifications to the CVLT-II recognition discriminability indices to enhance the characterization of recognition memory impairment in healthy aging and neurodegenerative disease [PhD dissertation]. San Diego: San Diego State University; 2019. [Link]
- Graves LV, Holden HM, Van Etten EJ, Delano-Wood L, Bondi MW, Salmon DP, et al. New yes/no recognition memory analysis on the California Verbal Learning Test-3: Clinical utility in Alzheimer’s and Huntington’s disease. Journal of the International Neuropsychological Society. 2018; 24(8):833-41. [DOI:10.1017/S1355617718000474] [PMID] [PMCID]
- Van Etten EJ, Graves LV, Taylor B, Holden HM, Lopez FV, Williams ME, et al. Recall and recognition discriminability in Parkinson’s disease and Huntington’s disease. Journal of Huntington’s Disease. 2019; 8(4):459-65. [DOI:10.3233/JHD-190346] [PMID]
- Rahmani F, Fathi M, Kazemi M, Bahadori E. Recognition of famous and unfamiliar faces among patients suffering from Amnesia Mild Cognitive Impairment (AMCI) and Alzheimer’s Disease. Iranian Journal of Psychiatry. 2019; 14(3):227-35. [DOI:10.18502/ijps.v14i3.1330] [PMID] [PMCID]
- Rahmani F, Haghshenas H, Mehrabanpour A, Mani A, Mahmoodi M. Shiraz Verbal Learning Test (SVLT): Normative data for neurologically intact speakers of Persian. Archives of Clinical Neuropsychology : The Official Journal of the National Academy of Neuropsychologists. 2017; 32(5):598-609. [DOI:10.1093/arclin/acx030] [PMID]
- Marsa R, Bahmani B, Barekati S. [Demoralization syndrome in elderly people living in nursing homes, community-dwelling elderly people and those receiving day care services from rehabilitation centers (Persian)]. Salmand: Iranian Journal of Ageing. 2020; 14(4):436-49. [Link]
- Patterson C, Clarfield M. Diagnostic procedures for dementia. Dementia: Presentations, differential diagnosis, and nosology. 2003; 61-88.
- Foroughan M, Jafari Z, Shirin Bayan P, Ghaem Magham Farahani Z, Rahgozar M. [Validation of Mini- Mental State Examination (MMSE) in the elderly population of Tehran (Persin)]. Advances in Cognitive Sciences. 2008; 10(2):29-37. [Link]
- Strauss E, Sherman EMS, Spreen O. A compendium of neuropsychological tests: Administration, norms, and commentary.New York: Oxford University Press. [Link]
- Clark LR, Delano-Wood L, Libon DJ, McDonald CR, Nation DA, Bangen KJ, et al. Are empirically-derived subtypes of mild cognitive impairment consistent with conventional subtypes? Journal of the International Neuropsychological Society. 2013; 19(6):635-45. [DOI:10.1017/S1355617713000313] [PMID] [PMCID]
- Russo MJ, Cohen G, Campos J, Martín ME, Clarens MF, Sabe L, et al. Usefulness of discriminability and response bias indices for the evaluation of recognition memory in mild cognitive impairment and Alzheimer disease. Dementia and Geriatric Cognitive Disorders. 2017; 43(1-2):1-14. [DOI:10.1159/000452255] [PMID]
- Algarabel S, Fuentes M, Escudero J, Pitarque A, Peset V, Mazón JF, et al. Recognition memory deficits in mild cognitive impairment. Neuropsychology, Development, and Cognition. Section B, Aging, Neuropsychology and Cognition. 2012; 19(5):608-19. [DOI:10.1080/13825585.2011.640657] [PMID]
- Bennett IJ, Golob EJ, Parker ES, Starr A. Memory evaluation in mild cognitive impairment using recall and recognition tests. Journal of Clinical and Experimental Neuropsychology. 2006; 28(8):1408-22. [DOI:10.1080/13803390500409583] [PMID]
- Budson AE, Wolk DA, Chong H, Waring JD. Episodic memory in Alzheimer’s disease: separating response bias from discrimination. Neuropsychologia. 2006; 44(12):2222-32. [DOI:10.1016/j.neuropsychologia.2006.05.024] [PMID]
- Flanagan EC, Wong S, DuttA, Tu S, Bertoux M, Irish M, et al. False recognition in behavioral variant frontotemporal dementia and Alzheimer’s disease-Disinhibition or amnesia? Frontiers in Aging Neuroscience. 2016; 8:177. [DOI:10.3389/fnagi.2016.00177] [PMID] [PMCID]
- Graves LV, Moreno CC, Seewald M, Holden HM, Van Etten EJ, Uttarwar V, et al. Effects of age and gender on recall and recognition discriminability. Archives of Clinical Neuropsychology. 2017; 32(8):972-9. [DOI:10.1093/arclin/acx024] [PMID] [PMCID]
- Hogervorst E, Xin X, Rahardjo T, Shifu X. The Hopkins Verbal Learning Test and detection of MCI and mild dementia: A literature review. Journal of Alzheimers Disease & Parkinsonism. 2014; 4(5):166. [Link]
- Lee M, Pooley J, Shankle W. Recognition memory deficits in Alzheimer’s disease: Modeling clinical groups and individual patients. Proceedings of theAnnual Meeting of the Cognitive Science Society. 2009; 31(13):2849-54. [Link]
- Libon DJ, Bondi MW, Price CC, Lamar M, Eppig J, Wambach DM, et al. Verbal serial list learning in mild cognitive impairment: A profile analysis of interference, forgetting, and errors. Journal ofthe International Neuropsychological Society. 2011; 17(5):905-14. [DOI:10.1017/S1355617711000944] [PMID] [PMCID]
- Matura S, Prvulovic D, Butz M, Hartmann D, Sepanski B, Linnemann K, et al. Recognition memory is associated with altered resting-state functional connectivity in people at genetic riskfor Alzheimer’s disease. European Journal of Neuroscience. 2014; 40(7):3128-35. [DOI:10.1111/ejn.12659] [PMID]
- O’Brien TJ. Memory profiles in amnestic mild cognitive impairment and their associations with other cognitive domains and functional abilities [PhD dissertation]. Birmingham: The University of Alabama at Birmingham; 2012. [Link]
- Rabin LA, Paré N, Saykin AJ, Brown MJ, Wishart HA, Flashman LA, et al. Differential memory test sensitivity for diagnosing amnestic mild cognitive impairment and predicting conversion to Alzheimer’s disease. Aging, Neuropsychology, and Cognition. 2009; 16(3):357-76. [DOI:10.1080/13825580902825220] [PMID] [PMCID]
- Sanborn V, Putcha D, Tremont G. Correlates of recognition memory performance in amnestic mild cognitive impairment. Journal of Clinical and Experimental Neuropsychology. 2018; 40(2):205-11. [DOI:10.1080/13803395.2017.1334043] [PMID]
- Snodgrass JG, Corwin J. Pragmatics of measuring recognition memory: Applications to dementia and amnesia. Journal of Experimental Psychology: General. 1988; 117(1):34-50. [DOI:10.1037/0096-3445.117.1.34] [PMID]
- Lekeu F, Van der Linden M, Degueldre C, Lemaire C, Luxen A, Franck G, et al. Effects of Alzheimer’s diseaseon the recognition of novel versus familiar words: Neuropsychological and clinico-metabolic data. Neuropsychology. 2003; 17(1):143-54. [DOI:10.1037/0894-4105.17.1.143] [PMID]
Type of Study: Research |
Subject:
Neurology
Received: 2022/01/13 | Accepted: 2022/07/20 | Published: 2023/07/01
Received: 2022/01/13 | Accepted: 2022/07/20 | Published: 2023/07/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |