Volume 18, Issue 4 (Winter 2024)
Salmand: Iranian Journal of Ageing 2024, 18(4): 554-569 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Damerchi lou A, Ghaffari M, Sadeghipour Roudsari M, Rakhshanderou S. Relationship of Perceived Social Support With Sleep Quality and Mental Health in the Elderly Referred to Health Centers in Tehran, Iran. Salmand: Iranian Journal of Ageing 2024; 18 (4) :554-569
URL: http://salmandj.uswr.ac.ir/article-1-2524-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2524-en.html
Aazam Damerchi lou1 

 , Mohtasham Ghaffari1
, Mohtasham Ghaffari1 

 , Maasomeh Sadeghipour Roudsari1
, Maasomeh Sadeghipour Roudsari1 

 , Sakineh Rakhshanderou *
, Sakineh Rakhshanderou * 

 2
2


 , Mohtasham Ghaffari1
, Mohtasham Ghaffari1 

 , Maasomeh Sadeghipour Roudsari1
, Maasomeh Sadeghipour Roudsari1 

 , Sakineh Rakhshanderou *
, Sakineh Rakhshanderou * 

 2
2
1- Department of Public Health, School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Public Health, School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran. , s_rakhshanderou@sbmu.ac.ir
2- Department of Public Health, School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran. , s_rakhshanderou@sbmu.ac.ir
Full-Text [PDF 7690 kb]
(506 Downloads)
| Abstract (HTML) (1065 Views)
Full-Text: (105 Views)
Introduction
The physical and functional changes in old age are effective in the social and psychological conditions of the person [1]. Due to issues such as retirement and loneliness, the elderly are prone to suffering from mental problems [2]. Depression is one of the common psychological disorders in old age [3]. Sleep disorders are also one of the most common problems that can cause a decrease in the quality of life, an increase in the risk of mental problems, a decrease in daily performance, and a disturbance in the emotions and motivation of the elderly [4]. Social support is one of the important factors that play a decisive role in improving mental health [5]. People with high social support have higher sense of belonging and self-esteem [6]. Some evidence has shown that a high level of social support encourages people to choose healthier lifestyles [7]. This study aims to examine the relationship between perceived social support and mental health components in the Iranian elderly.
Methods
This is a descriptive-analytical study that was conducted on the elderly in Tehran, Iran. The inclusion criteria were the ability to complete the questionnaire, the ability to communicate, and not having cognitive impairment. The exclusion criterion was the incomplete return of the questionnaire. Sampling was done by a two-stage cluster method. Using Cochran’s formula, the sample size was estimated to be 420 people at a confidence interval of 95%, considering P=0. 5, d=0. 05, and 10% sample drop. Data were collected using a demographic form, pittsburgh sleep quality index (PSQI), depression anxiety stress scale-21 (DASS-21), and the multidimensional scale of perceived social support (MSPSS).
The PSQI has 7 items and the total score ranges from 0 to 21; a higher score show the lower sleep quality. The DASS-21 is a self-report tool with 21 items rated on a 4-point scale as 0= Did not apply to me at all, 1= Applied to me to some degree, or some of the time, 2= Applied to me to a considerable degree or a good part of time, and 3= Applied to me very much or most of the time. The total score ranges from 0 to 42, where higher scores indicate higher levels of anxiety, depression, and stress. The MSPSS is a 12-item instrument. This scale measures a person’s perceived level of social support from three sources: family, friends, and significant others. The items are rated on a five-point scale ranging from strongly disagree to strongly agree. The total score ranges from 12 to 60, with a higher score indicating more perceived social support. Data were analyzed using descriptive statistics (frequency, percentage, mean, standard deviation, skewness and kurtosis) in SPSS software, version 25 and inferential statistics (path analysis) in EQS software, version 6.4. In path analysis, stress, anxiety and depression variables were considered as mediating variables. The direct and indirect relationships of social support and the components of mental health (stress, anxiety and depression) with the sleep quality of the elderly were calculated using the path analysis.
Results
In this study, 69% of the elderly were between 60 and 74 years old (younger elderly), and 31% were between 75 and 90 years old (older elderly). Moreover, 53.8% of the elderly were female and 46. 2% were male; 77.9% were married and 22.1% were unmarried; 12.6% had university education, 19.3% had diploma and 68.1% had lower than high school education; 13.6% had poor economic status, 70.2% had moderate economic status and 16.2% reported good economic status.
Skewness and kurtosis values for all variables were in the range of -2 to +2; therefore, the data had a normal distribution. The mean scores of depression, anxiety, and stress were 12.9±27.9,11.55±8.8, and 15.05±9.8, respectively. Based on the scores, 19. 3% had mild stress, 10.7% had moderate stress, 16% had severe stress, and 3.3% had very severe stress. Moreover, 6.7% reported mild anxiety, 23.1% moderate anxiety, 14.8% severe anxiety and 19.5% very severe anxiety. Furthermore, 9.5% had mild depression, 20.7% moderate depression, 8.3% severe depression and 6% very severe depression. The mean scores of PSQI and MSPSS were 8.5±2.52 and 47.26±8.5, respectively. Based on the scores, 8. 6% of the elderly had normal sleep quality and 91. 4% had sleep disorders.
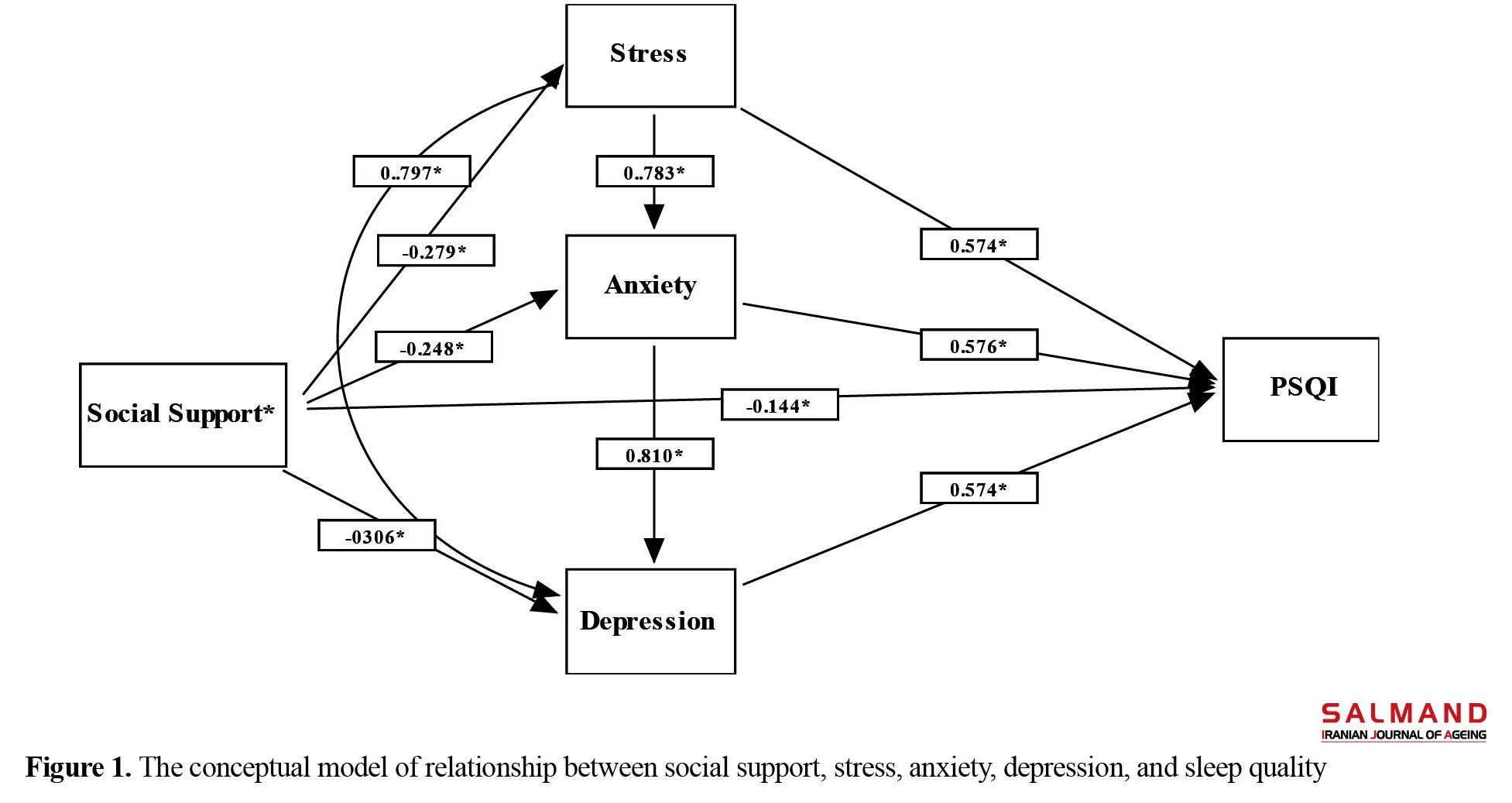
The findings from path analysis showed that social support had an indirect and significant relationship with the sleep quality, while the relationship between the components of mental health (stress, anxiety and depression) with the sleep quality was direct and significant. According to the findings, the direct correlation coefficient between social support and sleep quality was about 0.14 and the indirect correlation coefficient was about 0.48. The total direct and indirect correlation coefficient between social support and sleep quality was about 0.62. In other words, with increasing social support, the amount of change in sleep quality was 62%, and it can lead to better sleep quality. Figure 1 shows the structural model of the study.
Conclusion
The findings of this study showed a negative and significant relationship between social support and mental health components of the elderly in Tehran, Iran. In other words, higher social support perceived by an elderly person can lead to lower stress, anxiety, and depression and thus better mental health. Social support increases the mental health of the elderly by increasing the sense of intimacy and emotional support. Social support can be effective for subjective assessment of stressors. It can reduce stress and anxiety and promote social adjustment and well-being. By regulating the biological rhythm, it has an effect on maintaining sleep and wakefulness of an elderly person and causes a good quality of sleep in them.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the research ethics committee of Shahid Beheshti University of Medical Sciences (Code: R.SBMU.PHNS.REC.1400.070).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Implementation of the project, writing the article: Azam Demarchi Lo; design, data analysis, and interpretation: Sakineh Rakhshanderou; Methodology and data interpretation: Mohtsham Ghaffari; Consulting: Masoumeh Sadeghipour Rudsari. All authors reviewed and approved the manuscript.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all seniors and their families and the staff of comprehensive health service centers affiliated to Shahid Beheshti University of Medical Sciences for their cooperation in this study.
The physical and functional changes in old age are effective in the social and psychological conditions of the person [1]. Due to issues such as retirement and loneliness, the elderly are prone to suffering from mental problems [2]. Depression is one of the common psychological disorders in old age [3]. Sleep disorders are also one of the most common problems that can cause a decrease in the quality of life, an increase in the risk of mental problems, a decrease in daily performance, and a disturbance in the emotions and motivation of the elderly [4]. Social support is one of the important factors that play a decisive role in improving mental health [5]. People with high social support have higher sense of belonging and self-esteem [6]. Some evidence has shown that a high level of social support encourages people to choose healthier lifestyles [7]. This study aims to examine the relationship between perceived social support and mental health components in the Iranian elderly.
Methods
This is a descriptive-analytical study that was conducted on the elderly in Tehran, Iran. The inclusion criteria were the ability to complete the questionnaire, the ability to communicate, and not having cognitive impairment. The exclusion criterion was the incomplete return of the questionnaire. Sampling was done by a two-stage cluster method. Using Cochran’s formula, the sample size was estimated to be 420 people at a confidence interval of 95%, considering P=0. 5, d=0. 05, and 10% sample drop. Data were collected using a demographic form, pittsburgh sleep quality index (PSQI), depression anxiety stress scale-21 (DASS-21), and the multidimensional scale of perceived social support (MSPSS).
The PSQI has 7 items and the total score ranges from 0 to 21; a higher score show the lower sleep quality. The DASS-21 is a self-report tool with 21 items rated on a 4-point scale as 0= Did not apply to me at all, 1= Applied to me to some degree, or some of the time, 2= Applied to me to a considerable degree or a good part of time, and 3= Applied to me very much or most of the time. The total score ranges from 0 to 42, where higher scores indicate higher levels of anxiety, depression, and stress. The MSPSS is a 12-item instrument. This scale measures a person’s perceived level of social support from three sources: family, friends, and significant others. The items are rated on a five-point scale ranging from strongly disagree to strongly agree. The total score ranges from 12 to 60, with a higher score indicating more perceived social support. Data were analyzed using descriptive statistics (frequency, percentage, mean, standard deviation, skewness and kurtosis) in SPSS software, version 25 and inferential statistics (path analysis) in EQS software, version 6.4. In path analysis, stress, anxiety and depression variables were considered as mediating variables. The direct and indirect relationships of social support and the components of mental health (stress, anxiety and depression) with the sleep quality of the elderly were calculated using the path analysis.
Results
In this study, 69% of the elderly were between 60 and 74 years old (younger elderly), and 31% were between 75 and 90 years old (older elderly). Moreover, 53.8% of the elderly were female and 46. 2% were male; 77.9% were married and 22.1% were unmarried; 12.6% had university education, 19.3% had diploma and 68.1% had lower than high school education; 13.6% had poor economic status, 70.2% had moderate economic status and 16.2% reported good economic status.
Skewness and kurtosis values for all variables were in the range of -2 to +2; therefore, the data had a normal distribution. The mean scores of depression, anxiety, and stress were 12.9±27.9,11.55±8.8, and 15.05±9.8, respectively. Based on the scores, 19. 3% had mild stress, 10.7% had moderate stress, 16% had severe stress, and 3.3% had very severe stress. Moreover, 6.7% reported mild anxiety, 23.1% moderate anxiety, 14.8% severe anxiety and 19.5% very severe anxiety. Furthermore, 9.5% had mild depression, 20.7% moderate depression, 8.3% severe depression and 6% very severe depression. The mean scores of PSQI and MSPSS were 8.5±2.52 and 47.26±8.5, respectively. Based on the scores, 8. 6% of the elderly had normal sleep quality and 91. 4% had sleep disorders.
The findings from path analysis showed that social support had an indirect and significant relationship with the sleep quality, while the relationship between the components of mental health (stress, anxiety and depression) with the sleep quality was direct and significant. According to the findings, the direct correlation coefficient between social support and sleep quality was about 0.14 and the indirect correlation coefficient was about 0.48. The total direct and indirect correlation coefficient between social support and sleep quality was about 0.62. In other words, with increasing social support, the amount of change in sleep quality was 62%, and it can lead to better sleep quality. Figure 1 shows the structural model of the study.
Conclusion
The findings of this study showed a negative and significant relationship between social support and mental health components of the elderly in Tehran, Iran. In other words, higher social support perceived by an elderly person can lead to lower stress, anxiety, and depression and thus better mental health. Social support increases the mental health of the elderly by increasing the sense of intimacy and emotional support. Social support can be effective for subjective assessment of stressors. It can reduce stress and anxiety and promote social adjustment and well-being. By regulating the biological rhythm, it has an effect on maintaining sleep and wakefulness of an elderly person and causes a good quality of sleep in them.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the research ethics committee of Shahid Beheshti University of Medical Sciences (Code: R.SBMU.PHNS.REC.1400.070).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Implementation of the project, writing the article: Azam Demarchi Lo; design, data analysis, and interpretation: Sakineh Rakhshanderou; Methodology and data interpretation: Mohtsham Ghaffari; Consulting: Masoumeh Sadeghipour Rudsari. All authors reviewed and approved the manuscript.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all seniors and their families and the staff of comprehensive health service centers affiliated to Shahid Beheshti University of Medical Sciences for their cooperation in this study.
References
- van Gaans D, Dent E. Issues of accessibility to health services by older Australians: A review. Public Health Reviews. 2018; 39:20. [DOI:10.1186/s40985-018-0097-4] [PMID]
- Mirzaei M, Shams Ghahfarokhi M. [Demography of elder population in Iran over the period 1956 to 2006 (Persian)]. Salmand. 2007l 2(3):326-31. [Link]
- Davary Feizpour Azar S, Mehrmohammadi M, Talaie E, Imani M. [Identifying and prioritizing the educational needs of Iranian older adults (Persian)]. Salmand: Iranian Journal of Ageing. 2023; 18(3):378-95. [Link]
- Nabavi SH, Alipour F, Hejazi A, Rabani E, Rashedi V. [Relationship between social support and mental health in older adults (Persian)]. Medical Journal of Mashhad University of Medical Sciences. 2014; 57(7):841-6. [DOI:10.22038/MJMS.2014.3756]
- de Vries M, Emons WH, Plantinga A, Pietersma S, van den Hout WB, Stiggelbout AM, et al. Comprehensively measuring health-related subjective well-being: Dimensionality analysis for improved outcome assessment in health economics.Value in Health. 2016; 19(2):167-75. [PMID]
- Imanzadeh A, Alipoor S. [Examining the elderly women’s experiences of loneliness: A phenomenological study (Persian)]. Aging Psychology. 2017; 3(1):31-43. [Link]
- Hosseini zare SM, Movahed E, Pourreza A, Rahimi Foroshani A. [The effect of social support on the health of the elderly in Tehran (Persian)]. Journal of Hospital. 2015; 13(4):115-21. [Link]
- Bakhtiyari M, Emaminaeini M, Hatami H, Khodakarim S, Sahaf R. Depression and perceived social support in the elderly. Salmand. 2017; 12(2):192-207. [DOI:10.21859/sija-1202192]
- Anbäcken EM, Almqvist AL, Johansson C, Kinugasa K, Obata M, Hyun J, et al. Older adults and care: Reshaped family roles in societal change. A comparative study of Japan, South Korea, and Sweden. In: Claster PN, Blair SL, editors. Aging and the family: Understanding changes in structural and relationship dynamics. Leeds: Emerald Publishing Limited; 2021. [Link]
- World Health Organization. Mental health and psychological resilience during the COVID-19 pandemic [Internet]. 2020 [Updated 2020 March 27]. Available from: [Link]
- Asmundson GJG, Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders. 2020; 71:102211. [DOI:10.1016/j.janxdis.2020.102211] [PMID]
- Kwong ASF, Pearson RM, Adams MJ, Northstone K, Tilling K,Smith D, et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. The British Journal of Psychiatry. 2021; 218(6):334-43. [DOI:10.1192/bjp.2020.242] [PMID]
- Szkody E, Stearns M, Stanhope L, McKinney C. Stress-buffering role of social support during COVID-19. Family Process. 2021; 60(3):1002-15. [DOI:10.1111/famp.12618] [PMID]
- Grey I, Arora T, Thomas J, Saneh A, Tohme P, Abi-Habib R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Research. 2020; 293:113452. [PMID]
- Poorsharifi H, Farahmand Sabet M. [The relationship between social support and sleep quality with general health in residing nursing house elderly (Persian)]. Aging Psychology. 2015; 1(1):31-9. [Link]
- Poordad S, Momeni K, karami J. [The mediation role of social support and happiness on the relationship between gratitude and death anxiety in the elderly (Persian)]. Journal of Psychological Studies. 2019; 15(1):57-80. [Link]
- Amini chokami A, Razavi V. [Relationship between social support and hope and death anxiety among the old people of Tehran Omid Cultural Center (Persian)]. International Journal of Life Sciences. 2015; 9(2):65-70. [DOI:10.3126/ijls.v9i2.12052]
- Akbari M, Najafi S, Nadrian H. [The relationship between social capital perceived social support and the Women’s mental health in Sanandaj: A community-based study (Persian)]. Iranian Journal of Health Education and Health Promotion. 2017; 5(3):155-63. [DOI:10.30699/acadpub.ijhehp.5.3.155]
- Bavazin F, Sepahvandi MA. [The study of the relationship between social support and social and psychological well-being among elderly people in city of Khorramabad in 2017 (Persian)]. Nursing and Midwifery Journal. 2018; 15(12):931-8. [Link]
- Moghadam K, Mansour-Ghanaei R, Esmaeilpour Bandboni M, Atrkar-Roshan Z. [The relationship between social supports with depression among elderly in the eastern cities of Guilan (Persian)]. Tolooebehdasht. 2020; 19(2):85-95. [DOI:10.18502/tbj.v19i2.3398]
- Papi S, Karimi Z, Ghaed Amini Harooni G, Nazarpour A, Shahry P. [Determining the prevalence of sleep disorder and its predictors among elderly residents of nursing homes of Ahvaz city in 2017 (Persian)]. Salmand. 2019; 13(5):576-87. [DOI:10.32598/SIJA.13.Special-Issue.576]
- Sugisawa H. [Difference in impact of social support on morale and medical utilization between elderly with low activity of daily living and elderly with high activity of daily living (Japanese)]. Nihon Koshu Eisei Zasshi. 1993; 40(3):171-80. [PMID]
- Harbison J. Sleep disorders in older people. Age and Ageing. 2002; 31(suppl_2):6-9. [DOI:10.1093/ageing/31.suppl_2.6]
- Poursharifi H, Farahmand Sabet M. [The relationship between social support and sleep quality with general health in residing nursing house elderly (Persian)]. Aging Psychology. 2015; 1(1):31-9. [Link]
- Crowley K. Sleep and sleep disorders in older adults. Neuropsychology Review. 2011; 21(1):41-53. [DOI:10.1007/s11065-010-9154-6] [PMID]
- Farhadi A, Obeidavi Z, Movahedi Y, Rahimi M, Mobasher A. [The comparison and relationship of social support and stress with life satisfaction among the elderly of Khorramabad city in 2013 (Persian)]. Yafteh. 2015; 17(2):14-22. [Link]
- Maghsoudi A, Dindarloo S, Jamali T, Ghaed S, Rastgoo Z, Hassanipour Azgomi S. [Comparison of sleep quality and general health in elderly individuals living in their houses and nursing homes (Persian)]. Sadra Medical Journal. 2016; 4(3):161-72. [Link]
- Torabi S, Shahriari L, Zahedi R, Rahmanian S, Rahmanian K. A survey the prevalence of sleep disorders and their management in the elderly in Jahrom City; 2008. Journal of Jahrom University of Medical Sciences; 2012. 10(4):35-41. [DOI:10.29252/jmj.10.4.35]
- Mirzaei F, Khodabakhshi-Koolaee A. [The relationship between sleep quality and perceived social support with loneliness in elderly men (Persian)]. Journal of Gerontology. 2018; 2(4):11-20. [DOI:10.29252/joge.2.3.11]
- Cobb S. Presidential Address-1976. Social support as a moderator of life stress. Psychosomatic Medicine. 1976; 38(5):300-14. [DOI:10.1097/00006842-197609000-00003] [PMID]
- Bakhtiyari F, Foroughan M, Fakhrzadeh H, Nazari N, Najafi B, Alizadeh M, et al. [Validation of the persian version of abbreviated mental test (AMT) in elderly residents of Kahrizak charity foundation (Persian)]. Iranian Journal of Diabetes and Metabolism. 2014; 13(6):487-94. [Link]
- Foroughan M, Wahlund LO, Jafari Z, Rahgozar M, Farahani IG, Rashedi V. Validity and reliability of Abbreviated Mental Test Score (AMTS) among older Iranian. Psychogeriatrics. 2017; 17(6):460-5. [DOI:10.1111/psyg.12276] [PMID]
- Ahmadzadeh Vosta H, Hosseini R, Saneei H. [The relationship between sleep habits and sleep timing variables with sleep quality in the college students (Persian)]. Journal of Ilam University of Medical Sciences. 2013; 21(4):273-83. [Link]
- Hossein-Abadi R, Nowrouzi K, Pouresmaili R, Karimloo M, Maddah SSB. [Acupoint massage in improving sleep quality of older adults (Persian)]. Archives of Rehabilitation. 2008; 9(2):8-14. [Link]
- Sahebi A, Asghari M, Salari RS. Validation of anxiety, depression and stress scale (DASS21) for the Iranian population (Persian)]. Developmental Pscychology. 2005; 1(4):299-312. [Link]
- Salimi AR, Jokar B, Nikpour R. [Internet communication in life: investigating the role of social support perception and loneliness in Internet use (Persian)]. Journal of Psychological Studies. 2009; 5(3):81-102. [Link]
- Ghaderi S, Sahaf R, Mohammadi Shahbalaghi F, Ansari G, Gharanjic A, Ashrafi K, et al. [Prevalence of depression in elderly kurdish community residing in Boukan, Iran (Persian)]. Salmand. 2012; 7(1):57-66. [Link]
- Montazeri N, Sorbi M, Ahmadi S, Yazdanpoor S. [Comparative study of depression, anxiety and stress among athletic elderly versus nonathletic elderly in 1392 (Persian)]. The Scientific Journal of Rehabilitation Medicine. 2014; 3(2):15-22. [Link]
- Sobhani A, Shahnazi H, Mostafavi F. (2019). [The efficiency of theory-based education on mental health subscales in elders: Application of theory of planned behavior (Persian)]. Iranian Journal of Health Education and Health Promotion. 2019; 6(4):367-75. [DOI:10.30699/acadpub.ijhehp.6.4.367]
- Taheri Gharagzlu T, Safavi M, Fesharaki M. [The effect of employee’s humor training on depression, anxiety and stress of the elderly residents in Tehran’s nursing homes: A randomized clinical trial (Persian)]. Medical Science Journal of Islamic Azad University Tehran Medical Branch. 2020; 30(3):287-98. [DOI:10.29252/iau.30.3.287]
- Nazari S, Sharifi F, Gashtili N. [The relationship between aging perception with stress, anxiety and depression in the elderly members of the Tehran’s social security retirees in 2020 (Persian)]. Journal of Gerontology. 2021; 6(3):78-88. [Link]
- Fattahi Ardakani M, Mohammad Rezaei ZH, Saeed Jadgal M, Khodavandi S, Zareipour MA. [Investigating stress, anxiety and depression and its relationship with social support in military elderly (Persian)]. Journal of Military Medicine. 2021; 23(9):730-7. [DOI:10.30491/JMM.23.9.730]
- Marsa R, Younesi SJ, Barekati S, Ramshini M, Ghyasi H. [A comparative study on stress, anxiety and depression between nursing-home elderly residents and home-dwelling elderly people (Persian)]. Salmand. 2020; 15(2):176-87. [DOI:10.32598/sija.13.10.500]
- Soudagar S, Rambod M. [Prevalence of stress, anxiety and depression and their associations with spiritual well-being in patients with diabetes (Persian)]. Sadra Medical Science Journal. 2018; 6(1):1-10. [Link]
- Park JH, Yoo MS, Bae SH. Prevalence and predictors of poor sleep quality in Korean older adults. International Journal of Nursing Practice. 2013; 19(2):116-23. [DOI:10.1111/ijn.12047] [PMID]
- Roepke SK, Ancoli-Israel S. Sleep disorders in the elderly. The Indian Journal of Medical Research. 2010; 131:302-10. [PMID]
- Kaya H, Ayık B, Tasdelen R, Ercis M, Ertekin E. Social support promotes mental health during the COVID-19 outbreak: A cross-sectional study from Turkey. Psychiatria Danubina. 2021; 33(2):217-24. [DOI:10.24869/psyd.2021.217] [PMID]
- Tatsuno J, Unoki T, Sakuramoto H, Hamamoto M. Effects of social support on mental health for critical care nurses during the coronavirus disease 2019 (COVID-19) pandemic in Japan: A web-based cross-sectional study. Acute Medicine & Surgery. 2021; 8(1):e645. [DOI:10.1002/ams2.645] [PMID]
- Qi M, Zhou SJ, Guo ZC, Zhang LG, Min HJ, Li XM, et al. The effect of social support on mental health in chinese adolescents during the outbreak of COVID-19. The Journal of Adolescent Health. 2020; 67(4):514-8. [DOI:10.1016/j.jadohealth.2020.07.001]
- Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry. 2018; 18(1):156. [DOI:10.1186/s12888-018-1736-5] [PMID]
- Berkman LF, Kawachi I. Social epidemiology. Oxford: Oxford University Press; 2000. [DOI:10.1093/oso/9780195083316.001.0001]
- Adams MH, Bowden AG, Humphrey DS, McAdams LB. Social support and health promotion lifestylesof rural women. Online Journal of Rural Nursing and Health Care. 2000; 1(1):43-65. [DOI:10.14574/ojrnhc.v1i1.501]
- El-Zoghby SM, Soltan EM, Salama HM. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. Journal of Community Health. 2020; 45(4):689-95. [DOI:10.1007/s10900-020-00853-5] [PMID]
- Hajihasani M, Naderi N. [Death anxiety in the elderly: The role of spiritual health and perceived social support (Persian)]. Aging Psychology. 2021; 6(4):309-19. [Link]
Type of Study: Research |
Subject:
gerontology
Received: 2022/10/22 | Accepted: 2023/07/24 | Published: 2024/01/01
Received: 2022/10/22 | Accepted: 2023/07/24 | Published: 2024/01/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |