Volume 19, Issue 4 (Winter 2025)
Salmand: Iranian Journal of Ageing 2025, 19(4): 630-641 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rostamnia D, Marashi T, Sadeghipour Roudsari M, Namdari M. Investigating the Prevalence of Frailty in Community-dwelling Older Adults Living in Tehran City, Iran. Salmand: Iranian Journal of Ageing 2025; 19 (4) :630-641
URL: http://salmandj.uswr.ac.ir/article-1-2632-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2632-en.html
1- School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Public Health, School of Public Health and Safety, Shahid Beheshti University of Medical Science, Tehran, Iran. ,marashi142002@yahoo.com
3- Department of Public Health, School of Public Health and Safety, Shahid Beheshti University of Medical Science, Tehran, Iran.
2- Department of Public Health, School of Public Health and Safety, Shahid Beheshti University of Medical Science, Tehran, Iran. ,
3- Department of Public Health, School of Public Health and Safety, Shahid Beheshti University of Medical Science, Tehran, Iran.
Full-Text [PDF 4792 kb]
(1377 Downloads)
| Abstract (HTML) (3181 Views)
Full-Text: (636 Views)
Introduction
In the recent century, according to the decreasing fertility rate and promoting health status and life expectancy, the proportion of older people has increased in most societies and aging has become an important global phenomenon [1]. In the advanced years of life, maintaining homeostasis is challenging for body systems [6]. As a result, the physiologic system of the body may become frail. Frailty syndrome is composed of sarcopenia, malnutrition, and chronic inflammation which is presented as weight loss, weakness, slow gait, low physical activity, and exhaustion. This can result in adverse outcomes, such as falls, delirium, and disability. In Iran, few studies have investigated the prevalence and related factors of frailty. This study determines the prevalence and associated factors of frailty in community-dwelling older adults covered by Shahid Beheshti University of Medical Sciences in Tehran City, Iran.
Methods
This cross-sectional study was performed on 383 older people aged 60 years and older, covered by healthcare centers of Shahid Beheshti University of Medical Sciences, Tehran, Iran in 2022. The participants were selected using random multistage cluster sampling. The covered healthcare centers were the North Health Network (consisting of 78 centers), the East Health Network (consisting of 73 centers), and Shemiranat Health Network (consisting of 23 centers). At first, 10% of the centers of each region were selected as clusters of the sampling; accordingly, 8, 8, and 3 clusters from North, East, and Shemiranat networks were respectively selected randomly. In each cluster, 20-21 participants were selected. The inclusion criteria were being 60 years old and older, not having cognitive impairment, and having the ability to communicate and answer the questions. Meanwhile, the exclusion criterion was incomplete questionnaires. In the next step, the Tilburg frailty indicator (TFI) items were asked of the participants by the researcher. Data analysis was done using the SPSS software, version 23. The prevalence of frailty among the participants was calculated. The chi-square test and the t-test were used for the relationship between frailty and other variables. In addition, logistic regression was used for multivariable analysis of the related factors as well. All the tests were considered significant at P<0.05.
Results
In this study, 383 older people with a mean age of 68.2±6.3 years participated. Among the participants, 187 people (48.8%) were female, 64 people (16.7%) were living alone, 277 people (72%) were married, 242 people (63.2%) had multiple chronic diseases, and 325 people (84.9%) were satisfied with their environmental status. About 40.5% of the participants (155 people) were frail. Frailty was significantly associated with age (P<0.003), lack of partner (P<0.001), low educational status (P<0.036), low income (P<0.012), unhealthy lifestyle (P<0.001), having multiple chronic diseases (P<0.001), and dissatisfaction with the environment (P<0.001). Among the stressful life events, the loss of loved ones, experiencing a serious illness (P<0.001), and a serious illness in beloved ones (P=0.037) were significantly related to frailty. In multivariate logistic regression (Table 1) having multiple diseases (odd ratio [OR]=1.754, P=0.034), dissatisfaction with environmental status (OR=2.035, P=0.032), having serious illness (OR=3.279, P=0.001), having unhealthy lifestyle (OR=11.61, P=0.005), and having no healthy/no unhealthy lifestyle (OR=3.115, P=0.001) had significant effect on odds of frailty.
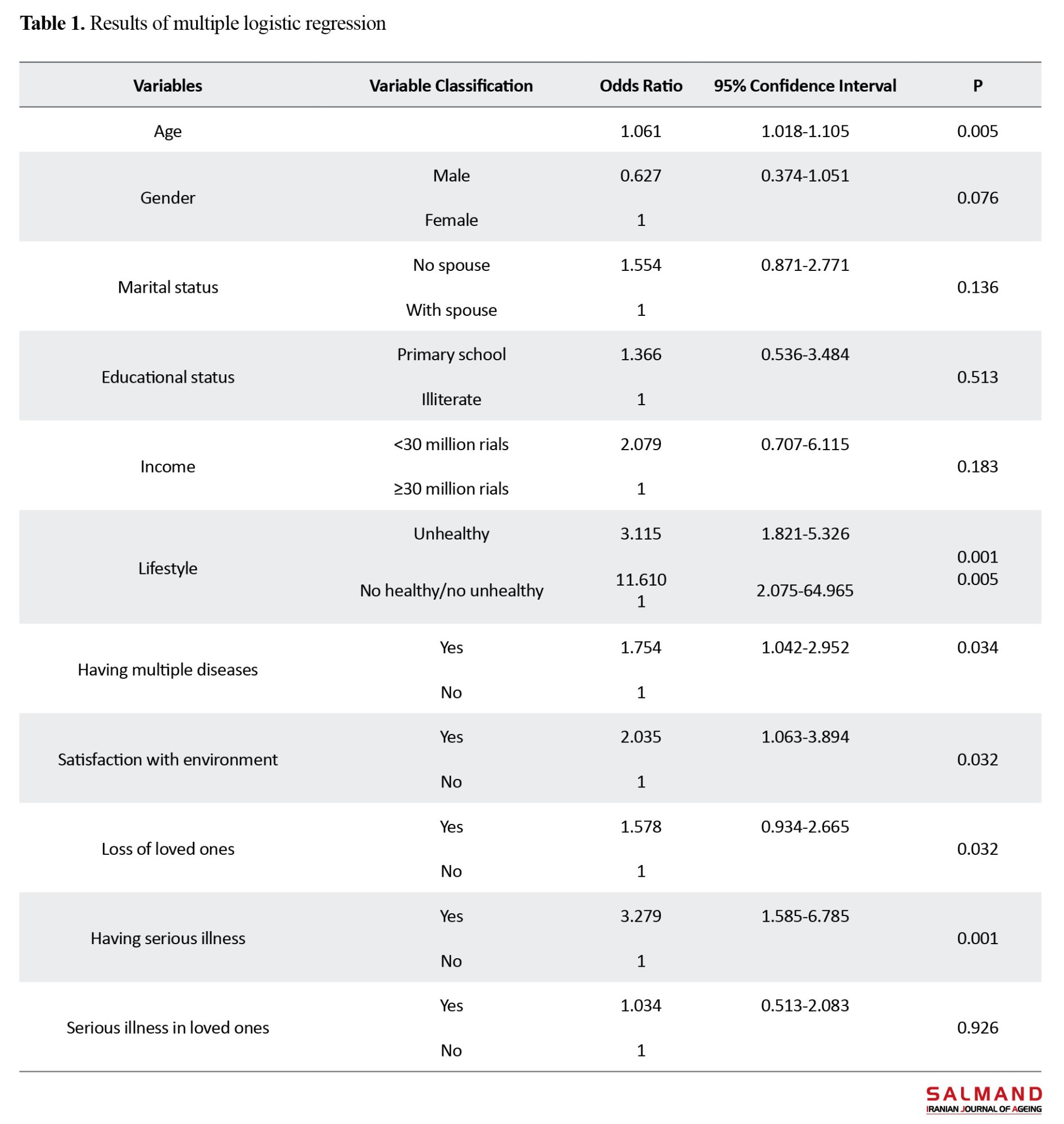
Also, for each year of increasing age, the chance of vulnerability increases by 0.06.
Conclusion
The prevalence of frailty was 40.5% using the Tilburg frailty scale. Although the differences between measurement scales and the population type in different studies result in various prevalence rates, the results of this study showed a significant prevalence rate in comparison with other studies in the world and It needs more attention. Although the sampling was randomized, we invited older people to attend healthcare centers and frail older people were more likely to be unable to come. So the prevalence may be a bit lower than the real rate. It is also the same for omitting the people who had cognitive decline. The standard diagnostic tool for assessing the prevalence of frailty is comprehensive geriatric assessment but because There was not an available professional team, the Tilburg frailty scale was used to estimate an acceptable prevalence of frailty.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (Code: IR.SBMU.PHNS.REC.1400.110).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contribute to preparing all parts of the research.
Conflicts of interest
The authors declared no conflict of interest.
References
In the recent century, according to the decreasing fertility rate and promoting health status and life expectancy, the proportion of older people has increased in most societies and aging has become an important global phenomenon [1]. In the advanced years of life, maintaining homeostasis is challenging for body systems [6]. As a result, the physiologic system of the body may become frail. Frailty syndrome is composed of sarcopenia, malnutrition, and chronic inflammation which is presented as weight loss, weakness, slow gait, low physical activity, and exhaustion. This can result in adverse outcomes, such as falls, delirium, and disability. In Iran, few studies have investigated the prevalence and related factors of frailty. This study determines the prevalence and associated factors of frailty in community-dwelling older adults covered by Shahid Beheshti University of Medical Sciences in Tehran City, Iran.
Methods
This cross-sectional study was performed on 383 older people aged 60 years and older, covered by healthcare centers of Shahid Beheshti University of Medical Sciences, Tehran, Iran in 2022. The participants were selected using random multistage cluster sampling. The covered healthcare centers were the North Health Network (consisting of 78 centers), the East Health Network (consisting of 73 centers), and Shemiranat Health Network (consisting of 23 centers). At first, 10% of the centers of each region were selected as clusters of the sampling; accordingly, 8, 8, and 3 clusters from North, East, and Shemiranat networks were respectively selected randomly. In each cluster, 20-21 participants were selected. The inclusion criteria were being 60 years old and older, not having cognitive impairment, and having the ability to communicate and answer the questions. Meanwhile, the exclusion criterion was incomplete questionnaires. In the next step, the Tilburg frailty indicator (TFI) items were asked of the participants by the researcher. Data analysis was done using the SPSS software, version 23. The prevalence of frailty among the participants was calculated. The chi-square test and the t-test were used for the relationship between frailty and other variables. In addition, logistic regression was used for multivariable analysis of the related factors as well. All the tests were considered significant at P<0.05.
Results
In this study, 383 older people with a mean age of 68.2±6.3 years participated. Among the participants, 187 people (48.8%) were female, 64 people (16.7%) were living alone, 277 people (72%) were married, 242 people (63.2%) had multiple chronic diseases, and 325 people (84.9%) were satisfied with their environmental status. About 40.5% of the participants (155 people) were frail. Frailty was significantly associated with age (P<0.003), lack of partner (P<0.001), low educational status (P<0.036), low income (P<0.012), unhealthy lifestyle (P<0.001), having multiple chronic diseases (P<0.001), and dissatisfaction with the environment (P<0.001). Among the stressful life events, the loss of loved ones, experiencing a serious illness (P<0.001), and a serious illness in beloved ones (P=0.037) were significantly related to frailty. In multivariate logistic regression (Table 1) having multiple diseases (odd ratio [OR]=1.754, P=0.034), dissatisfaction with environmental status (OR=2.035, P=0.032), having serious illness (OR=3.279, P=0.001), having unhealthy lifestyle (OR=11.61, P=0.005), and having no healthy/no unhealthy lifestyle (OR=3.115, P=0.001) had significant effect on odds of frailty.
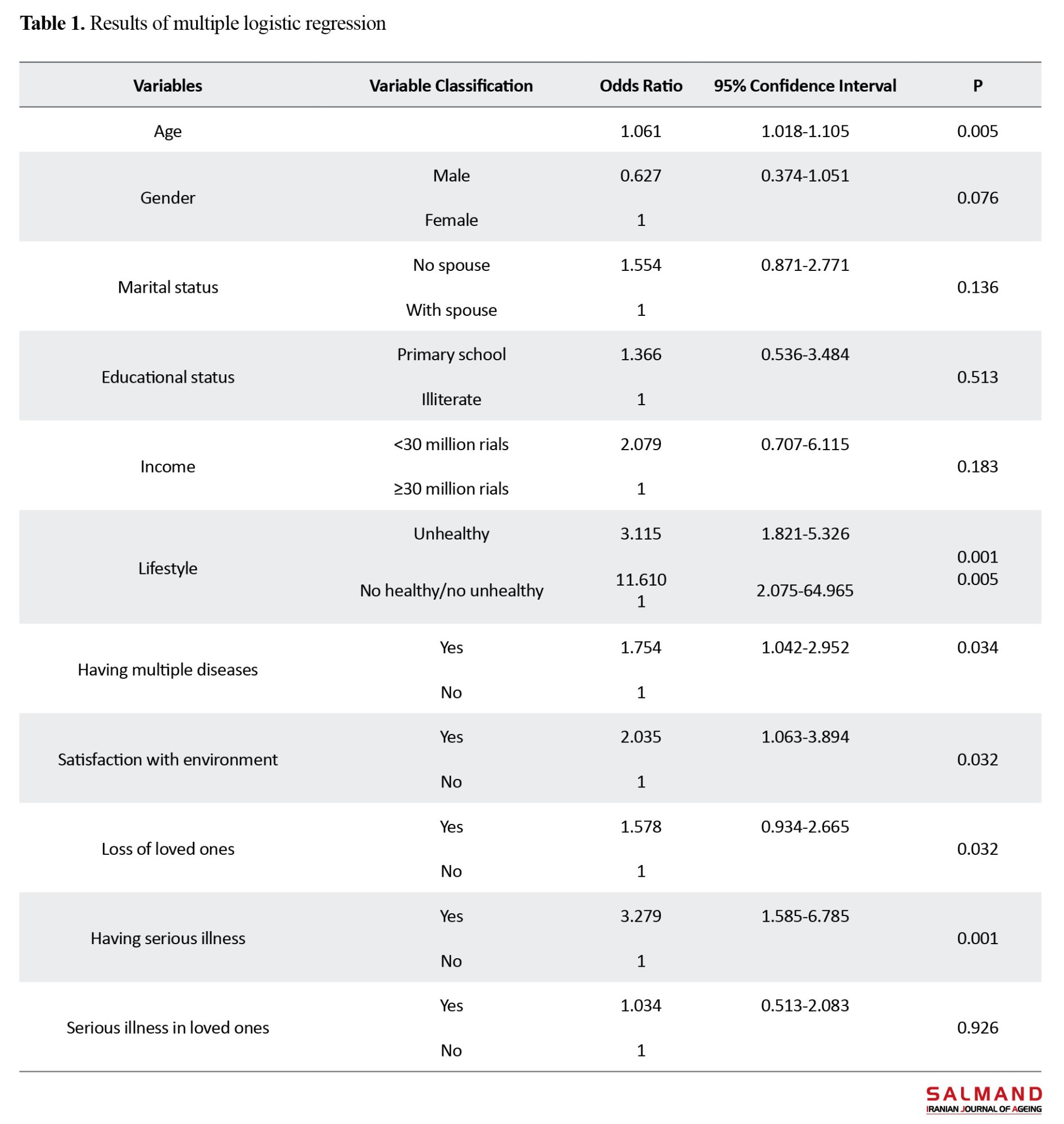
Also, for each year of increasing age, the chance of vulnerability increases by 0.06.
Conclusion
The prevalence of frailty was 40.5% using the Tilburg frailty scale. Although the differences between measurement scales and the population type in different studies result in various prevalence rates, the results of this study showed a significant prevalence rate in comparison with other studies in the world and It needs more attention. Although the sampling was randomized, we invited older people to attend healthcare centers and frail older people were more likely to be unable to come. So the prevalence may be a bit lower than the real rate. It is also the same for omitting the people who had cognitive decline. The standard diagnostic tool for assessing the prevalence of frailty is comprehensive geriatric assessment but because There was not an available professional team, the Tilburg frailty scale was used to estimate an acceptable prevalence of frailty.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (Code: IR.SBMU.PHNS.REC.1400.110).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contribute to preparing all parts of the research.
Conflicts of interest
The authors declared no conflict of interest.
References
- Namadian M, Ghobadi S. [Evaluation of mental status old ages Zanjan on 2001 (Persian)]. Tehran: Ashna Publications; 2006.
- World Health Organization (WHO). The world health report 2008: Primary health care now more than ever. Geneva: World Health Publication; 2008. [Link]
- Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults-present status and future implications. The Lancet. 2015; 385(9967):563-75. [DOI:10.1016/S0140-6736(14)61462-8]
- Ortman JM, Velkoff VA, Hogan H. An aging nation: The older population in the United States. New York: United States Census Bureau; 2014. [Link]
- Hayes N. Hazzard’s geriatric medicine and gerontology. Nursing Older People. 2010; 22(6):10-1. [DOI:10.7748/nop.22.6.10.s15]
- Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: A review. European Journal of Internal Medicine. 2016; 31:3-10. [DOI:10.1016/j.ejim.2016.03.007]
- Halter JB, Ouslander JG, Studenski S, High KP, Asthana S, Supiano MA, et al. Hazzard’s geriatric medicine and gerontology. New York: McGraw-Hill Professional Publishing; 2009. [Link]
- Dent E, Visvanathan R, Piantadosi C, Chapman I. Use of the Mini Nutritional Assessment to detect frailty in hospitalised older people. The Journal of Nutrition, Health & Aging. 2012; 16(9):764-7. [DOI:10.1007/s12603-012-0405-5]
- Kojima G, Liljas A, Iliffe S. Frailty syndrome: implications and challenges for health care policy. Risk Management and Healthcare Policy. 2019; 2019:23-30. [DOI:10.2147/RMHP.S168750]
- To TL, Doan TN, Ho WC, Liao WC. Prevalence of frailty among community-dwelling older adults in Asian countries: A systematic review and meta-analysis. Healthcare. 2022; 10(5):895. [DOI:10.3390/healthcare10050895]
- Alqahtani BA, Alshehri MM, Elnaggar RK, Alsaad SM, Alsayer AA, Almadani N, et al. Prevalence of frailty in the middle east: systematic review and meta-analysis. Healthcare. 2022; 10(1):108. [DOI:10.3390/healthcare10010108]
- Boura FT, Hosseini SR, Mouodi S, Ghadimi R, Bijani A. Frailty syndrome in older adults and related sociodemographic factors in the north of Iran: A population-based study. Iranian Red Crescent Medical Journal. 2021; 23(1):e249. [DOI:10.32592/ircmj.2021.23.1.249]
- Saeidimehr S, Delbari A, Zanjari N, Fadaye Vatan R. [Factors related to frailty among older adults in Khuzestan, Iran (Persian)]. Salmad. 2021; 16(2):202-17. [DOI:10.32598/sija.16.2.1600.1]
- Mousavi Sisi M, Shamshirgaran SM, Rezaeipandari H, Matlabi H. Multidimensional approach to frailty among rural older people: Applying the tilburg frailty indicator. Elderly Health Journal. 2019; 5(2):92-101. [DOI:10.18502/ehj.v5i2.2155]
- Khodamradi M. [Prevalence of vulnerabilities and related factors in people 50 years and older in Bukan (Persian)]. Tabriz: Tabriz University of Medical Sciences; 2017.
- Hodkinson H. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age and Ageing. 1972; 1(4):233-8. [DOI:10.1093/ageing/1.4.233]
- Santiago LM, Luz LL, Mattos IE, Gobbens RJ, van Assen MA. Psychometric properties of the Brazilian version of the Tilburg frailty indicator (TFI). Archives of Gerontology and Geriatrics. 2013; 57(1):39-45. [DOI:10.1016/j.archger.2013.03.001]
- Mazoochi F, Gobbens RJ, Lotfi M-s, Fadayevatan R. Diagnostic accuracy of the Tilburg Frailty Indicator (TFI) for early frailty detection in elderly people in Iran. Archives of Gerontology and Geriatrics. 2020; 91:104187. [DOI:10.1016/j.archger.2020.104187]
- Ge L, Yap CW, Heng BH. Prevalence of frailty and its association with depressive symptoms among older adults in Singapore. Aging & Mental Health. 2019; 23(3):319-24. [DOI:10.1080/13607863.2017.1416332]
- Yu R, Wu WC, Leung J, Hu SC, Woo J. Frailty and its contributory factors in older adults: A comparison of two asian regions (hong kong and taiwan). International Journal of Environmental Research and Public Health. 2017; 14(10):1096. [DOI:10.3390/ijerph14101096]
- Sinclair DR, Maharani A, Chandola T, Bower P, Hanratty B, Nazroo J, et al. Frailty among older adults and its distribution in England. The Journal of Frailty & Aging. 2022; 11:163-8. [DOI:10.14283/jfa.2021.55]
- Jafarian Yazdi A, Pashaii Sabet F, Moosavi Arfa N, Hasani MM. [Prevalence of frailty and factors associated with frailty in the hospitalized elderly (Persian)]. Iranian Journal of Nursing Research. 2021; 16(1):1-9. [Link]
- Gobbens RJ, van Assen MA, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Determinants of frailty. Journal of the American Medical Directors Association. 2010; 11(5):356-64. [DOI:10.1016/j.jamda.2009.11.008] [PMID]
Type of Study: Research |
Subject:
gerontology
Received: 2023/05/25 | Accepted: 2024/02/07 | Published: 2025/01/01
Received: 2023/05/25 | Accepted: 2024/02/07 | Published: 2025/01/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |