Volume 20, Issue 3 (Autumn 2025)
Salmand: Iranian Journal of Ageing 2025, 20(3): 422-437 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hosseini S R, Amini N, Bijani A, Ghadimi R, Ahangari N, Faramarzi M. Trends in Depressive Symptoms and the Factors Affecting Them in Older Adults: A Prospective Cohort Study. Salmand: Iranian Journal of Ageing 2025; 20 (3) :422-437
URL: http://salmandj.uswr.ac.ir/article-1-2858-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2858-en.html
Seyed Reza Hosseini1 

 , Nasrin Amini2
, Nasrin Amini2 

 , Ali Bijani1
, Ali Bijani1 

 , Reza Ghadimi1
, Reza Ghadimi1 

 , Neda Ahangari1
, Neda Ahangari1 

 , Mahbobeh Faramarzi *3
, Mahbobeh Faramarzi *3 




 , Nasrin Amini2
, Nasrin Amini2 

 , Ali Bijani1
, Ali Bijani1 

 , Reza Ghadimi1
, Reza Ghadimi1 

 , Neda Ahangari1
, Neda Ahangari1 

 , Mahbobeh Faramarzi *3
, Mahbobeh Faramarzi *3 


1- Social Determinants of Health Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
2- Student Research Committee, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
3- Social Determinants of Health Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran. ,mahbob330@yahoo.com
2- Student Research Committee, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
3- Social Determinants of Health Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran. ,
Full-Text [PDF 5322 kb]
(1192 Downloads)
| Abstract (HTML) (3014 Views)
Full-Text: (790 Views)
Introduction
Depression is one of the most prevalent types of mental illness in older adults, which has a negative impact on their physical health and daily functioning. Late-life depression is a complex and heterogeneous condition with a chronic course. Older adults are more likely to have cognitive and physical problems, in contrast to younger adults who show more emotional symptoms [12]. Various risk factors play a role in the onset and course of depression [10]. Monitoring depression in older adults and identifying the factors related to its onset, exacerbation, or recovery is crucial for planning timely and effective interventions in order to improve the mental health of older adults. This study aims to determine the trajectory of depressive symptoms over a five-year period in older adults from Amirkola City, Mazandaran, north of Iran, and to identify the effective factors.
Methods & Materials
In this prospective study, 800 older adults (aged 60 and above) were selected from phase 1 (2011) and phase 2 (2016) of the Amirkola health and ageing project (AHAP) cohort study using a simple random sampling. Inclusion criteria were age ≥60, residing in Amirkola, and having data available in both phases of the cohort study. Exclusion criteria were disability based on the scores of activities of daily living (ADL) and instrumental activities of daily living (IADL) questionnaires at the start of the study, or death during the study period. The study compared depressive symptoms between the participants of the two phases and assessed the relationship of these symptoms with demographic characteristics, physical activity, and cognitive status. Demographic data, including age, gender, education level, and marital status, were recorded using a demographic form. Depressive symptoms were assessed using the geriatric depression scale (GDS). A total GDS score ≥5 indicates symptoms of depression, a score of 0-4 indicates mild depression, a score of 5-8 indicates moderate depression, and a score of 9-11 indicates severe depression. Also, cognitive status was measured by the mini-mental state examination (MMSE), and physical activity by the physical activity scale for the elderly (PASE). The data were analyzed using t-test and chi-square test as well as regression analysis to find the related factors. P<0.05 was considered statistically significant. All statistical analyses were conducted in SPSS software, version 26.
Results
Among 800 older adults, 460 were male (57.5%) and 340 were female (42.5%). Their mean age was 67.4±6.36 years. The prevalence of depression in the first phase of the cohort study was 39.2%, which decreased to 35.25% in the second phase (P=0.001); however, the severity of depression showed little change (Table 1).
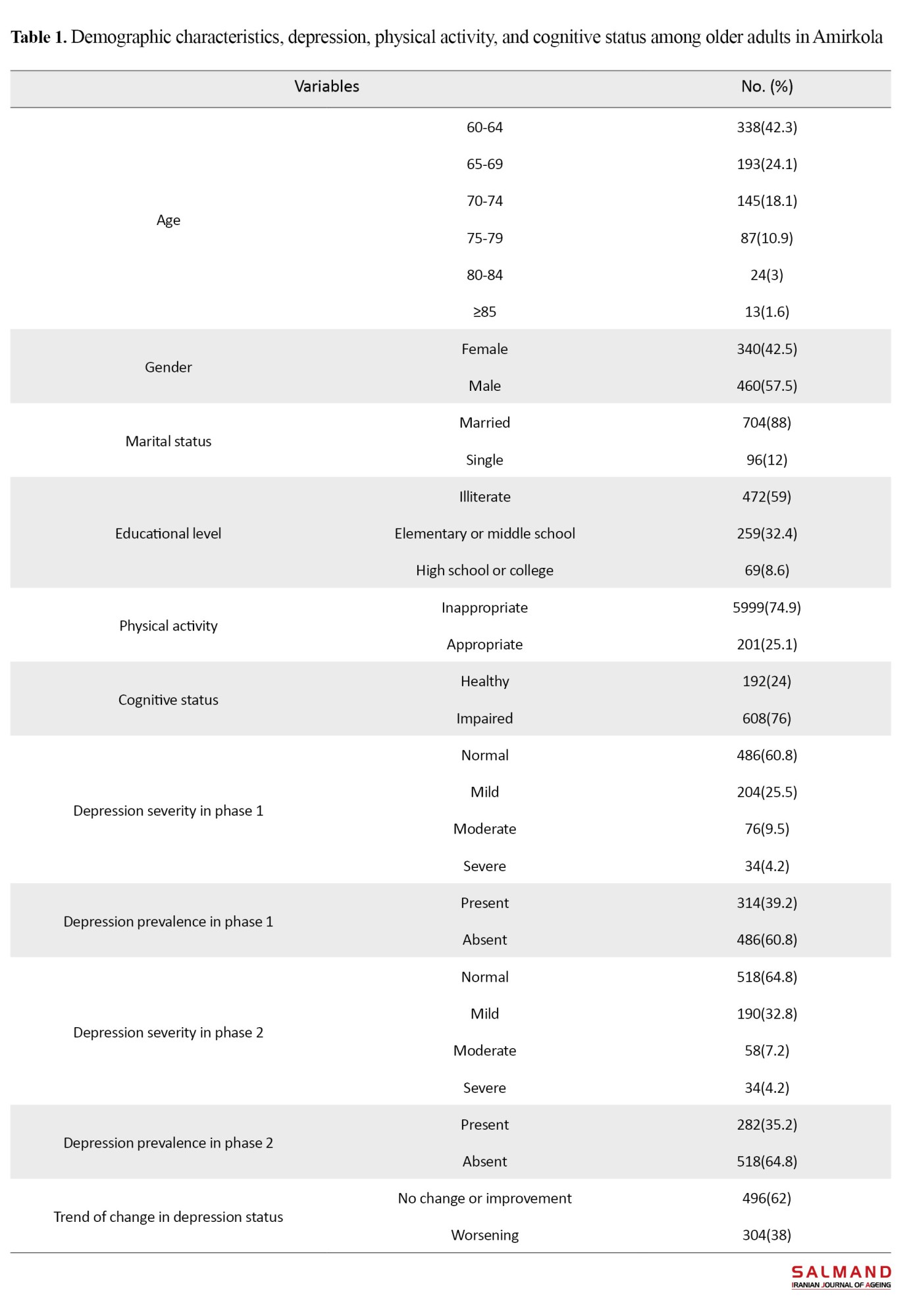
In the first phase, 25.5% of older adults had mild depression, 9.5% had moderate depression, and 4.2% had severe depression. In the second phase, these percentages shifted to 23.7%, 7.2%, and 4.2%, respectively. The mean GDS score in the first phase was 4.28±3.35, which decreased to 3.96±3.46 in the second phase, and this reduction was statistically significant (P=0.007).
The McNemar test results revealed that 20.4% of the older adults developed new depressive symptoms after 5 years, while 58.2% experienced persistent depression (P<0.001). Logistic regression model identified male gender and lower educational levels as risk factors for worsening depressive symptoms in older adults. Physical activity and cognitive status did not have a significant effect on the progression of depression. Among predicting factors, higher educational level played an important role in reducing depression, as those with a high school education or higher level were 60% less likely to experience worsening depressive symptoms.
Conclusion
Over the five-year follow-up of 800 older adults in Amirkola, 20% developed depression and 58.2% experienced persistent symptoms. Older men are at higher risk for depression compared to older women, and a higher educational level is a protective factor. As untreated depression can result in significant complications in older adults, the study emphasizes the importance of timely referrals to psychiatrists for the treatment of depression in older adults. It is recommended that all physicians regularly screen for depression during medical visits with older adults and refer suspected cases to mental health specialists.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Health Research Institute, Babol University of Medical Sciences, Babol, Iran (Code: IR.MUBABOL.HRI.REC.1401.215). All study objectives and methods were explained to participants and their written informed consent was obtained.
Funding
This study was extracted from the MD dissertation of Nasrin Amini in Medical Sciences, funded by Babol University of Medical Sciences, Babol, Iran.
Authors' contributions
Conceptualization: Seyed Reza Hosseini; design: Seyed Reza Hosseini and Mahbobeh Faramarzi; Data analysis: Ali Bijani; Investigation Nasrin Amini; Supervision: Reza Ghadimi; Writing the original draft: Neda Ahangari; Review & editing: Mahbobe Fharamarzi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research and Technology of Babol University of Medical Sciences, Babol, Iran, for the financial support, the AHAP cohort study center, and all seniors who participated in this project.
Depression is one of the most prevalent types of mental illness in older adults, which has a negative impact on their physical health and daily functioning. Late-life depression is a complex and heterogeneous condition with a chronic course. Older adults are more likely to have cognitive and physical problems, in contrast to younger adults who show more emotional symptoms [12]. Various risk factors play a role in the onset and course of depression [10]. Monitoring depression in older adults and identifying the factors related to its onset, exacerbation, or recovery is crucial for planning timely and effective interventions in order to improve the mental health of older adults. This study aims to determine the trajectory of depressive symptoms over a five-year period in older adults from Amirkola City, Mazandaran, north of Iran, and to identify the effective factors.
Methods & Materials
In this prospective study, 800 older adults (aged 60 and above) were selected from phase 1 (2011) and phase 2 (2016) of the Amirkola health and ageing project (AHAP) cohort study using a simple random sampling. Inclusion criteria were age ≥60, residing in Amirkola, and having data available in both phases of the cohort study. Exclusion criteria were disability based on the scores of activities of daily living (ADL) and instrumental activities of daily living (IADL) questionnaires at the start of the study, or death during the study period. The study compared depressive symptoms between the participants of the two phases and assessed the relationship of these symptoms with demographic characteristics, physical activity, and cognitive status. Demographic data, including age, gender, education level, and marital status, were recorded using a demographic form. Depressive symptoms were assessed using the geriatric depression scale (GDS). A total GDS score ≥5 indicates symptoms of depression, a score of 0-4 indicates mild depression, a score of 5-8 indicates moderate depression, and a score of 9-11 indicates severe depression. Also, cognitive status was measured by the mini-mental state examination (MMSE), and physical activity by the physical activity scale for the elderly (PASE). The data were analyzed using t-test and chi-square test as well as regression analysis to find the related factors. P<0.05 was considered statistically significant. All statistical analyses were conducted in SPSS software, version 26.
Results
Among 800 older adults, 460 were male (57.5%) and 340 were female (42.5%). Their mean age was 67.4±6.36 years. The prevalence of depression in the first phase of the cohort study was 39.2%, which decreased to 35.25% in the second phase (P=0.001); however, the severity of depression showed little change (Table 1).
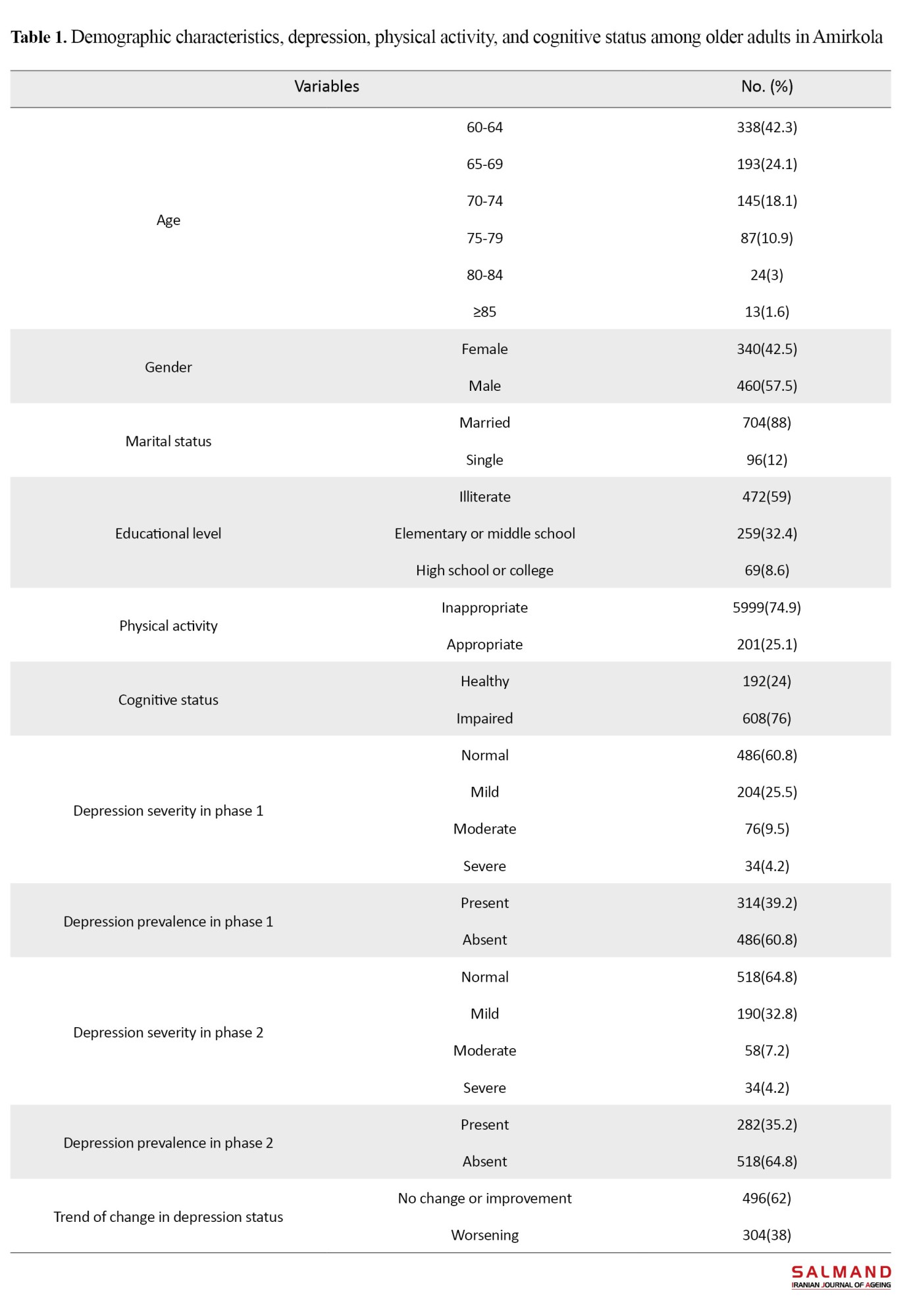
In the first phase, 25.5% of older adults had mild depression, 9.5% had moderate depression, and 4.2% had severe depression. In the second phase, these percentages shifted to 23.7%, 7.2%, and 4.2%, respectively. The mean GDS score in the first phase was 4.28±3.35, which decreased to 3.96±3.46 in the second phase, and this reduction was statistically significant (P=0.007).
The McNemar test results revealed that 20.4% of the older adults developed new depressive symptoms after 5 years, while 58.2% experienced persistent depression (P<0.001). Logistic regression model identified male gender and lower educational levels as risk factors for worsening depressive symptoms in older adults. Physical activity and cognitive status did not have a significant effect on the progression of depression. Among predicting factors, higher educational level played an important role in reducing depression, as those with a high school education or higher level were 60% less likely to experience worsening depressive symptoms.
Conclusion
Over the five-year follow-up of 800 older adults in Amirkola, 20% developed depression and 58.2% experienced persistent symptoms. Older men are at higher risk for depression compared to older women, and a higher educational level is a protective factor. As untreated depression can result in significant complications in older adults, the study emphasizes the importance of timely referrals to psychiatrists for the treatment of depression in older adults. It is recommended that all physicians regularly screen for depression during medical visits with older adults and refer suspected cases to mental health specialists.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Health Research Institute, Babol University of Medical Sciences, Babol, Iran (Code: IR.MUBABOL.HRI.REC.1401.215). All study objectives and methods were explained to participants and their written informed consent was obtained.
Funding
This study was extracted from the MD dissertation of Nasrin Amini in Medical Sciences, funded by Babol University of Medical Sciences, Babol, Iran.
Authors' contributions
Conceptualization: Seyed Reza Hosseini; design: Seyed Reza Hosseini and Mahbobeh Faramarzi; Data analysis: Ali Bijani; Investigation Nasrin Amini; Supervision: Reza Ghadimi; Writing the original draft: Neda Ahangari; Review & editing: Mahbobe Fharamarzi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research and Technology of Babol University of Medical Sciences, Babol, Iran, for the financial support, the AHAP cohort study center, and all seniors who participated in this project.
References
- Mehri N, Messkoub M, Kunkel S. Trends, determinants and the implications of population aging in Iran. Ageing International. 2020; 45(4):327-43. [DOI:10.1007/s12126-020-09364-z]
- Gomes SRBS, von Schantz M, Leocadio-Miguel M. Predicting depressive symptoms in middle-aged and elderly adults using sleep data and clinical health markers: A machine learning approach. Sleep Medicine. 2023; 102:123-31. [DOI:10.1016/j.sleep.2023.01.002] [PMID]
- Antony A, Parida SP, Behera P, Padhy SK. Geriatric depression: Prevalence and its associated factors in rural Odisha. Frontiers in Public Health. 2023; 11:1180446. [DOI:10.3389/fpubh.2023.1180446] [PMID]
- Hu T, Zhao X, Wu M, Li Z, Luo L, Yang C, et al. Prevalence of depression in older adults: A systematic review and meta-analysis. Psychiatry Research. 2022; 311:114511. [DOI:10.1016/j.psychres.2022.114511]
- Golboni F, Mahmoodi H, Baghi V, Ghanei Gheshlagh R, Valiee S, Dalvand P, et al. Prevalence of Depression among Iranian Elderly: A systematic review and Meta-analysis of Observational Studies. Journal of Preventive and Complementary Medicine. 2022; 1(2):70-80. [Link]
- Yu B, Zhang X, Wang C, Sun M, Jin L, Liu X. Trends in depression among Adults in the United States, NHANES 2005-2016. Journal of Affective Disorders. 2020; 263:609-20. [DOI:10.1016/j.jad.2019.11.036] [PMID]
- Moreno-Agostino D, Wu YT, Daskalopoulou C, Hasan MT, Huisman M, Prina M. Global trends in the prevalence and incidence of depression: A systematic review and meta-analysis. Journal of Affective Disorders. 2021; 281:235-43. [DOI:10.1016/j.jad.2020.12.035] [PMID]
- Cai H, Jin Y, Liu R, Zhang Q, Su Z, Ungvari GS, et al. Global prevalence of depression in older adults: A systematic review and meta-analysis of epidemiological surveys. Asian Journal of Psychiatry. 2023; 80:103417. [DOI:10.1016/j.ajp.2022.103417] [PMID]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet. 2007;3 70(9590):851-8. [DOI:10.1016/S0140-6736(07)61415-9] [PMID]
- Paiva TC, Soares L, Faria AL. Depression in elderly people. Encyclopedia. 2023; 3(2):677-86. [DOI:10.3390/encyclopedia3020048]
- Haigh EAP, Bogucki OE, Sigmon ST, Blazer DG. Depression among older adults: A 20-year update on five common myths and misconceptions. The American Journal of Geriatric Psychiatry. 2018; 26(1):107-22. [DOI:10.1016/j.jagp.2017.06.011] [PMID]
- Ferraz PM. [Depressão e envelhecimento (Portugal)] [MA thesis]. Coimbra: Universidade de Coimbra; 2014. [Link]
- Birk JL, Kronish IM, Moise N, Falzon L, Yoon S, Davidson KW. Depression and multimorbidity: Considering temporal characteristics of the associations between depression and multiple chronic diseases. Health Psychology. 2019; 38(9):802-11. [DOI:10.1037/hea0000737] [PMID]
- Wang Q, Tian W. Prevalence, awareness, and treatment of depressive symptoms among the middle‐aged and elderly in China from 2008 to 2015. The International Journal of Health Planning and Management. 2018; 33(4):1060-70. [DOI:10.1002/hpm.2581] [PMID]
- de la Torre-Luque A, de la Fuente J, Sanchez-Niubo A, Caballero FF, Prina M, Muniz-Terrera G, et al. Stability of clinically relevant depression symptoms in old-age across 11 cohorts: A multi-state study. Acta Psychiatrica Scandinavica. 2019; 140(6):541-51. [DOI:10.1111/acps.13107] [PMID]
- Allahyari E, Keramati M, Kamali M. [Predicting elderly depression prevalence in different Iranian ethnicities and associated factors (Persian)]. Iranian Journal of Ageing. 2020; 15 (1):94-103. [DOI:10.32598/sija.2020.3.130]
- Richards D. Prevalence and clinical course of depression: A review. Clinical Psychology Review. 2011; 31(7):1117-25. [DOI:10.1016/j.cpr.2011.07.004] [PMID]
- Pengpid S, Peltzer K, Anantanasuwong D. Prevalence and determinants of incident and persistent depressive symptoms among middle-aged and older adults in Thailand: Prospective cohort study. BJPsych open. 2023; 9(3):e99. [DOI:10.1192/bjo.2023.72] [PMID]
- Muhammad T, Meher T. Association of late-life depression with cognitive impairment: Evidence from a cross-sectional study among older adults in India. BMC Geriatrics. 2021; 21(1):364. [DOI:10.1186/s12877-021-02314-7]
- Bijani A, Ghadimi R, Mikaniki E, Kheirkhah F, Mozaffarpur SA, Motallebnejad M, et al. Cohort profile update: The Amirkola Health and Ageing Project (AHAP). Caspian Journal of Internal Medicine. 2017; 8(3):205-12. [PMID]
- Hosseini SR, Cumming RG, Kheirkhah F, Nooreddini H, Baiani M, Mikaniki E, et al. Cohort profile: the Amirkola Health and Ageing Project (AHAP). International Journal of Epidemiology. 2014; 43(5):1393-400. [DOI:10.1093/ije/dyt089] [PMID]
- Khodadadi S, Pourhadi S, Hosseini SR, Sum S, Kheirkhah F, Mohammadi Z. [Investigating the relationship between social support, cognitive status, and depression with daily life activities of the elderly in Amirkola City (Persian)]. Salmand: Iranian Journal of Ageing 2022; 17 (1) :2-15. [DOI:10.32598/sija.2021.593.4]
- Malakouti SK, Fatollahi P, Mirabzadeh A, Salavati M, Zandi T. Reliability, validity and factor structure of the GDS‐15 in Iranian elderly. International Journal of Geriatric Psychiatry. 2006; 21(6):588-93. [DOI:10.1002/gps.1533] [PMID]
- Ansari NN, Naghdi S, Hasson S, Valizadeh L, Jalaie S. Validation of a Mini-Mental State Examination (MMSE) for the Persian population: A pilot study. Applied Neuropsychology. 2010; 17(3):190-5. [PMID]
- Taheri Tanjani P, Azadbakht M. [Psychometric properties of the Persian version of the activities of daily living scale and instrumental activities of daily living scale in elderly (Persian)]. Journal of Mazandaran University of Medical Sciences. 2016; 25(132):103-12. [Link]
- Hatami O, Aghabagheri M, Kahdouei S, Nasiriani K. Psychometric properties of the Persian version of the Physical Activity Scale for the Elderly (PASE). BMC Geriatrics. 2021; 21(1):383. [DOI:10.1186/s12877-021-02337-0] [PMID]
- Lee SL, Pearce E, Ajnakina O, Johnson S, Lewis G, Mann F, et al. The association between loneliness and depressive symptoms among adults aged 50 years and older: A 12-year population-based cohort study. The lancet. Psychiatry. 2021; 8(1):48-57. [DOI:10.1016/S2215-0366(20)30383-7] [PMID]
- Basta M, Micheli K, Simos P, Zaganas I, Panagiotakis S, Koutra K, et al. Frequency and risk factors associated with depression in elderly visiting Primary Health Care (PHC) settings: Findings from the Cretan Aging Cohort. Journal of Affective Disorders Reports. 2021; 4:100109. [DOI:10.1016/j.jadr.2021.100109]
- Van As BAL, Imbimbo E, Franceschi A, Menesini E, Nocentini A. The longitudinal association between loneliness and depressive symptoms in the elderly: A systematic review. International Psychogeriatrics. 2022; 34(7):657-69. [DOI:10.1017/S1041610221000399] [PMID]
- Du M, Dai W, Liu J, Tao J. Less social participation is associated with a higher risk of depressive symptoms among Chinese older adults: A community-based longitudinal prospective cohort study. Frontiers in Public Health. 2022; 10:781771. [DOI:10.3389/fpubh.2022.781771] [PMID]
- de la Torre-Luque A, Ayuso-Mateos JL. The course of depression in late life: A longitudinal perspective. Epidemiology and Psychiatric Sciences. 2020; 29:e147. [DOI:10.1017/S204579602000058X] [PMID]
- Comijs HC, Nieuwesteeg J, Kok R, van Marwijk HW, van der Mast RC, Naarding P, et al. The two-year course of late-life depression; results from the Netherlands study of depression in older persons. BMC Psychiatry. 2015; 15:20. [DOI:10.1186/s12888-015-0401-5] [PMID]
- Zenebe Y, Akele B, W/Selassie M, Necho M. Prevalence and determinants of depression among old age: A systematic review and meta-analysis. Annals of General Psychiatry. 2021; 20(1):55. [DOI:10.1186/s12991-021-00375-x] [PMID]
- Maier A, Riedel-Heller SG, Pabst A, Luppa M. Risk factors and protective factors of depression in older people 65+. A systematic review. Plos One. 2021; 16(5):e0251326. [DOI:10.1371/journal.pone.0251326] [PMID]
- Comijs HC, van Marwijk HW, van der Mast RC, Naarding P, Oude Voshaar RC, Beekman AT, et al. The Netherlands study of depression in older persons (NESDO); A prospective cohort study. BMC Research Notes. 2011; 4:524. [DOI:10.1186/1756-0500-4-524] [PMID]
- Yang X, Pan A, Gong J, Wen Y, Ye Y, Wu JH, et al. Prospective associations between depressive symptoms and cognitive functions in middle-aged and elderly Chinese adults. Journal of Affective Disorders. 2020; 263:692-7. [DOI:10.1016/j.jad.2019.11.048] [PMID]
- Bulloch AGM, Williams JVA, Lavorato DH, Patten SB. The depression and marital status relationship is modified by both age and gender. Journal of Affective Disorders. 2017; 223:65-8. [DOI:10.1016/j.jad.2017.06.007] [PMID]
- Paul R, Muhammad T, Rashmi R, Sharma P, Srivastava S, Zanwar PP. Depression by gender and associated factors among older adults in India: Implications for age-friendly policies. Scientific Reports. 2023; 13(1):17651. [DOI:10.1038/s41598-023-44762-8] [PMID]
Type of Study: Research |
Subject:
gerontology
Received: 2024/06/15 | Accepted: 2024/10/22 | Published: 2025/10/01
Received: 2024/06/15 | Accepted: 2024/10/22 | Published: 2025/10/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |