Volume 20, Issue 1 (Spring 2025)
Salmand: Iranian Journal of Ageing 2025, 20(1): 136-155 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Asiri S, Rahimi H, Kazemnezhad Leyli E, Pourvakhshoori N. Investigating the Effects of Sleep Health Education Based on Mobile Application on Sleep Quality of the Elderly: A Quasi-Experimental Study. Salmand: Iranian Journal of Ageing 2025; 20 (1) :136-155
URL: http://salmandj.uswr.ac.ir/article-1-2917-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2917-en.html
1- Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Biostatistics, Road Trauma Research Center, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. & Medical Education Research Center, Education Development Center, Guilan University of Medical Sciences, Rasht, Iran. ,nvakhshoori@gums.ac.ir
2- Department of Biostatistics, Road Trauma Research Center, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. & Medical Education Research Center, Education Development Center, Guilan University of Medical Sciences, Rasht, Iran. ,
Full-Text [PDF 9118 kb]
(1473 Downloads)
| Abstract (HTML) (3022 Views)
Full-Text: (1232 Views)
Introduction
The aging population is a global phenomenon, and addressing the needs arising from it is one of the most pressing concerns in today’s world [1]. Periodic censuses from the Iranian Statistics Center indicate that the elderly population has increased at twice the rate of the overall population over the past 60 years. According to the latest official statistics from the National Statistics Center of Iran in 2018, the elderly population in Guilan City, Iran, exceeds the national average, constituting approximately 13.25% of the total population [5]. Sleep disorders are prevalent issues that significantly affect the quality of life for the elderly. Sleep hygiene training, which aims to modify beliefs and habits related to sleep, is a non-pharmacological approach to treating these disorders [11]. The use of mobile phones represents a cost-effective and efficient method to promote self-care among patients [9]. This study investigates the effect of sleep health education delivered via a mobile application on the sleep quality of elderly individuals covered by the national pension fund in Rasht City, Iran, in 2022.
Methods & Materials
This semi-experimental study was conducted in two phases. Initially, 330 elderly individuals were recruited, and their sleep quality was assessed using a designated tool. Subsequently, 96 individuals with low sleep quality were randomly divided into two groups of 48 subjects, namely an intervention group and a control group. The inclusion criteria were having 60 years of age or higher, not suffering from substance abuse disorders, membership in the Rasht State Pension Fund, possessing minimum literacy, and having the ability to communicate through sight and hearing. Meanwhile, the exclusion criteria in the first phase included incomplete or improperly completed questionnaires.
The data collection tool comprised a two-part questionnaire, including personal-social information and the Pittsburgh sleep quality index (PSQI). The Pittsburgh sleep quality index includes seven scales measuring subjective sleep quality, sleep onset delay, sleep duration, sleep adequacy, sleep disorders, use of sleeping medications, and daily functioning disorders [26]. The intervention group received training on using the mobile-based sleep health educational application during two face-to-face sessions and was instructed to implement its programs daily for four weeks. A training booklet related to the application was also provided. The researcher followed up by phone twice a week. After four weeks, the sleep quality questionnaire was completed again for both groups, and after the research was completed, the educational application and sleep health educational booklet were provided to the control group. Data analysis included the Chi-square tests and the 1-way analysis of variance to compare baseline characteristics between groups, paired t-tests for within-group comparisons, and analysis of covariance (multivariate analysis of covariance) to compare means between groups post-intervention. The data were analyzed using the SPSS software, version 24, considering a significance level of 0.05.
Results
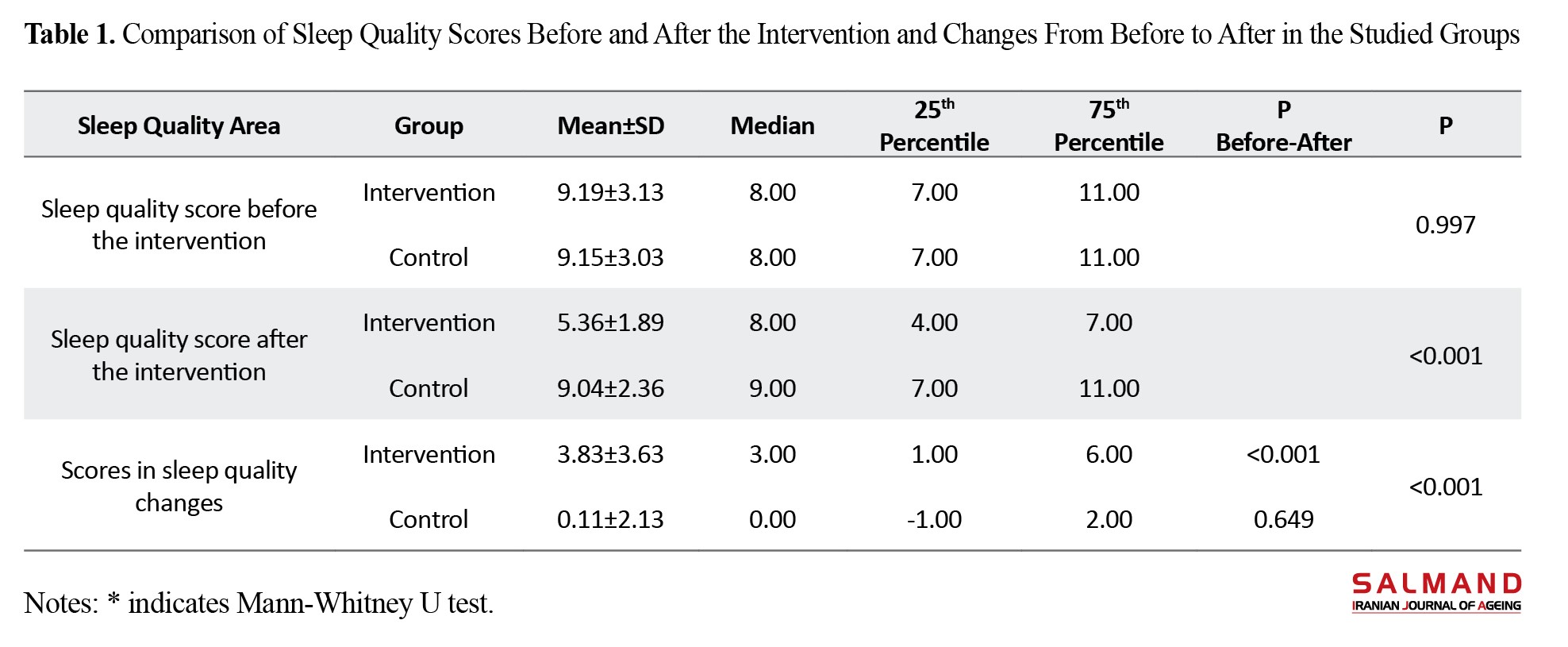
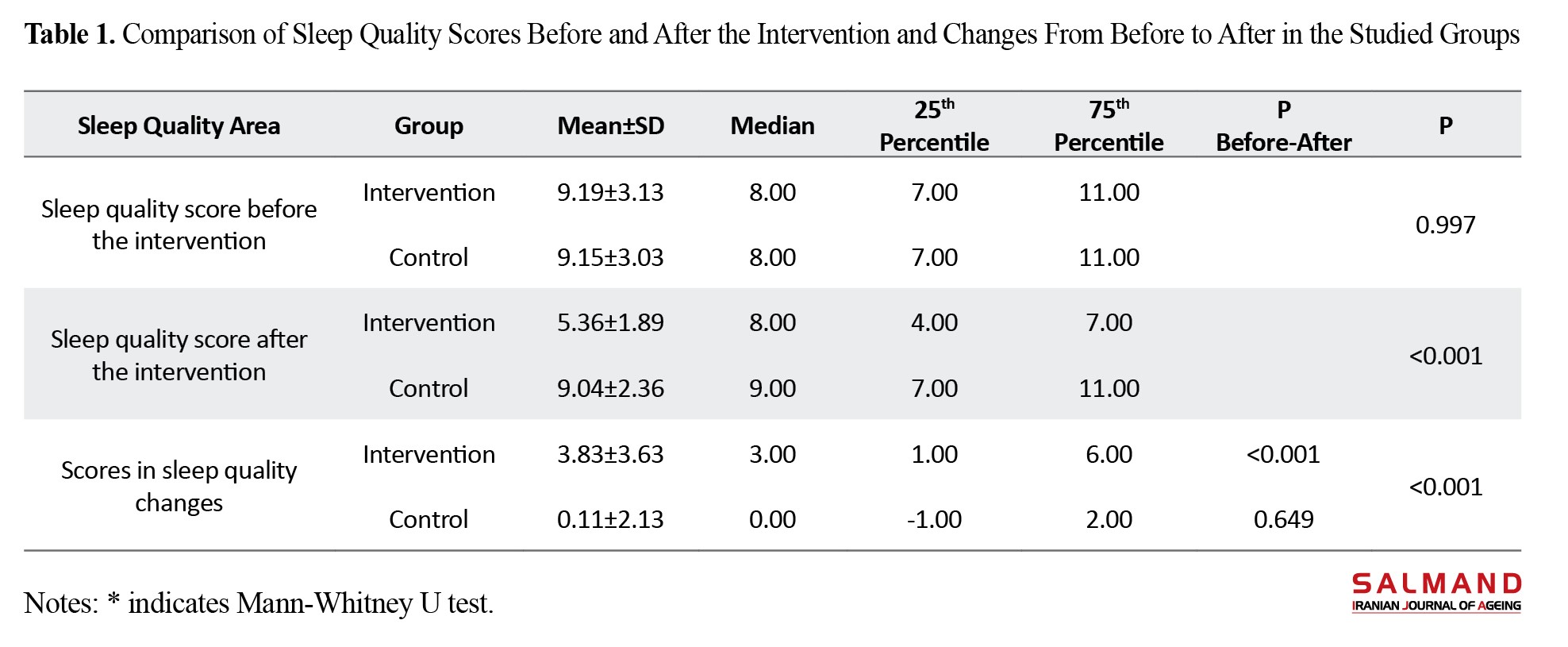
The results indicated that the average age of elderly participants was 68.98±6.52 years, with a majority being female (60.1%), married (83.3%), living in urban areas (91.5%), and possessing a university education (52%). The mean sleep quality score for the elderly was 5.37±3.88, influenced by various factors, including gender, education level, marital status, living arrangements, underlying health conditions, and employment status (P≤0.05). Among various aspects of sleep quality, sleep onset delay and use of sleep medications were identified as having the most and least issues, respectively. The comparison of changes in sleep quality domains between the two groups revealed significant differences in mental quality of sleep, sleep onset delay, sleep duration, use of sleeping pills, and daily dysfunction (P>0.100). The control group did not exhibit significant changes in these areas. Intra-group comparisons showed significant improvements in the intervention group across all areas except for sleep duration (P=0.830). Conversely, the control group showed no significant changes or, if any, an increase in sleep quality scores. In the control group, only the sleep disorder (P=0.100) and sleep efficiency (P=0.024) domains showed a statistically significant decline. Comparing the sleep quality score before and after the intervention and the changes in the two groups shows no statistically significant difference between the two groups before the intervention (P=0.997); however, after the intervention, there was a significant difference (P<0.001). The mean and median scores of sleep quality in the control group were higher than in the intervention group.
Also, the changes in sleep quality scores from before to after were significant between the two groups (P<0.001). The decreasing changes in the mean and median of the intervention group were significantly higher than the control group. Also, in the comparison between the two groups, sleep quality scores decreased significantly from before to after in the intervention group (P<0.001); nevertheless, these changes were not significant in the control group (P=649) (Table 1).
Notably, after the intervention, 96% of the control group reported poor sleep quality, while only 43% of the intervention group did. Multivariate analysis of covariance analysis indicated that sleep hygiene education significantly improved sleep quality across all areas, except for sleep efficiency (P≥0.05).
Conclusion
Sleep health education utilizing accessible and practical methods enhances the sleep quality of the elderly. The global proliferation of mobile phone technology has been accompanied by the development of educational applications that enhance health education and self-care. This method offers the benefits of increasing access to educational, self-care, and medical services quickly and simply. Mobile applications are particularly important for the elderly, who may be more vulnerable and have limited mobility. Although the number of studies in this field remains limited, existing research, including this study, demonstrates promising results regarding mobile phone-based interventions aimed at improving sleep quality among the elderly. These findings support the use of such interventions to alleviate insomnia symptoms in elderly individuals who cannot access face-to-face interventions. Given the high prevalence of sleep disorders and their associated complications in this demographic, this model is recommended as a non-pharmacological treatment for managing sleep disorders, targeting healthcare workers, the elderly, and their caregivers.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1401.322) and Iranian Registry of Clinical Trials (IRCT) (Code: IRCT20220926056042N1).
Funding
This article was extracted from the master’s thesis of Hananeh Rahimi in community health nursing funded by Guilan University of Medical Sciences and was done with the financial support of the Research Vice-Chancellor of this university.
Authors' contributions
Study design and investigation: Shahla Asiri, Hananeh Rahimi, and Negar Pourvakhshoori; Data analysis: Ehsan Kazemnejad; original draft preparation: Negar Pourvakhshoori; Review and editing: Shahla Asiri
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all participants in this research for their cooperation.
References
The aging population is a global phenomenon, and addressing the needs arising from it is one of the most pressing concerns in today’s world [1]. Periodic censuses from the Iranian Statistics Center indicate that the elderly population has increased at twice the rate of the overall population over the past 60 years. According to the latest official statistics from the National Statistics Center of Iran in 2018, the elderly population in Guilan City, Iran, exceeds the national average, constituting approximately 13.25% of the total population [5]. Sleep disorders are prevalent issues that significantly affect the quality of life for the elderly. Sleep hygiene training, which aims to modify beliefs and habits related to sleep, is a non-pharmacological approach to treating these disorders [11]. The use of mobile phones represents a cost-effective and efficient method to promote self-care among patients [9]. This study investigates the effect of sleep health education delivered via a mobile application on the sleep quality of elderly individuals covered by the national pension fund in Rasht City, Iran, in 2022.
Methods & Materials
This semi-experimental study was conducted in two phases. Initially, 330 elderly individuals were recruited, and their sleep quality was assessed using a designated tool. Subsequently, 96 individuals with low sleep quality were randomly divided into two groups of 48 subjects, namely an intervention group and a control group. The inclusion criteria were having 60 years of age or higher, not suffering from substance abuse disorders, membership in the Rasht State Pension Fund, possessing minimum literacy, and having the ability to communicate through sight and hearing. Meanwhile, the exclusion criteria in the first phase included incomplete or improperly completed questionnaires.
The data collection tool comprised a two-part questionnaire, including personal-social information and the Pittsburgh sleep quality index (PSQI). The Pittsburgh sleep quality index includes seven scales measuring subjective sleep quality, sleep onset delay, sleep duration, sleep adequacy, sleep disorders, use of sleeping medications, and daily functioning disorders [26]. The intervention group received training on using the mobile-based sleep health educational application during two face-to-face sessions and was instructed to implement its programs daily for four weeks. A training booklet related to the application was also provided. The researcher followed up by phone twice a week. After four weeks, the sleep quality questionnaire was completed again for both groups, and after the research was completed, the educational application and sleep health educational booklet were provided to the control group. Data analysis included the Chi-square tests and the 1-way analysis of variance to compare baseline characteristics between groups, paired t-tests for within-group comparisons, and analysis of covariance (multivariate analysis of covariance) to compare means between groups post-intervention. The data were analyzed using the SPSS software, version 24, considering a significance level of 0.05.
Results
The results indicated that the average age of elderly participants was 68.98±6.52 years, with a majority being female (60.1%), married (83.3%), living in urban areas (91.5%), and possessing a university education (52%). The mean sleep quality score for the elderly was 5.37±3.88, influenced by various factors, including gender, education level, marital status, living arrangements, underlying health conditions, and employment status (P≤0.05). Among various aspects of sleep quality, sleep onset delay and use of sleep medications were identified as having the most and least issues, respectively. The comparison of changes in sleep quality domains between the two groups revealed significant differences in mental quality of sleep, sleep onset delay, sleep duration, use of sleeping pills, and daily dysfunction (P>0.100). The control group did not exhibit significant changes in these areas. Intra-group comparisons showed significant improvements in the intervention group across all areas except for sleep duration (P=0.830). Conversely, the control group showed no significant changes or, if any, an increase in sleep quality scores. In the control group, only the sleep disorder (P=0.100) and sleep efficiency (P=0.024) domains showed a statistically significant decline. Comparing the sleep quality score before and after the intervention and the changes in the two groups shows no statistically significant difference between the two groups before the intervention (P=0.997); however, after the intervention, there was a significant difference (P<0.001). The mean and median scores of sleep quality in the control group were higher than in the intervention group.
Also, the changes in sleep quality scores from before to after were significant between the two groups (P<0.001). The decreasing changes in the mean and median of the intervention group were significantly higher than the control group. Also, in the comparison between the two groups, sleep quality scores decreased significantly from before to after in the intervention group (P<0.001); nevertheless, these changes were not significant in the control group (P=649) (Table 1).
Notably, after the intervention, 96% of the control group reported poor sleep quality, while only 43% of the intervention group did. Multivariate analysis of covariance analysis indicated that sleep hygiene education significantly improved sleep quality across all areas, except for sleep efficiency (P≥0.05).
Conclusion
Sleep health education utilizing accessible and practical methods enhances the sleep quality of the elderly. The global proliferation of mobile phone technology has been accompanied by the development of educational applications that enhance health education and self-care. This method offers the benefits of increasing access to educational, self-care, and medical services quickly and simply. Mobile applications are particularly important for the elderly, who may be more vulnerable and have limited mobility. Although the number of studies in this field remains limited, existing research, including this study, demonstrates promising results regarding mobile phone-based interventions aimed at improving sleep quality among the elderly. These findings support the use of such interventions to alleviate insomnia symptoms in elderly individuals who cannot access face-to-face interventions. Given the high prevalence of sleep disorders and their associated complications in this demographic, this model is recommended as a non-pharmacological treatment for managing sleep disorders, targeting healthcare workers, the elderly, and their caregivers.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1401.322) and Iranian Registry of Clinical Trials (IRCT) (Code: IRCT20220926056042N1).
Funding
This article was extracted from the master’s thesis of Hananeh Rahimi in community health nursing funded by Guilan University of Medical Sciences and was done with the financial support of the Research Vice-Chancellor of this university.
Authors' contributions
Study design and investigation: Shahla Asiri, Hananeh Rahimi, and Negar Pourvakhshoori; Data analysis: Ehsan Kazemnejad; original draft preparation: Negar Pourvakhshoori; Review and editing: Shahla Asiri
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all participants in this research for their cooperation.
References
- Abdi A, Tarjoman A, Borji M. Prevalence of elder abuse in Iran: A Systematic review and meta-analysis. Asian Journal of Psychiatry. 22019; 39:120-7. [DOI:10.1016/j.ajp.2018.12.005] [PMID]
- Vizeshfar F, Ghelbash Z. Effect of a self-care training program using smartphones on general health, nutrition status, and sleep quality in the elderly. Psychogeriatrics. 2021; 21(6):910-9. [DOI:10.1111/psyg.12766] [PMID]
- Piroozi B, Mohamadi-Bolbanabad A, Shokri A.The growth of aging population in Iran: An achievement or a challenge? Journal of Gerontological Social Work. 2024; 67(6):711-4. [DOI:10.1080/01634372.2024.2340725] [PMID]
- Beard JR, Officer AM, Cassels AK. The world report on ageing and health. Gerontologist. 2016; 56 (Suppl 2):S163-6. [PMID]
- Fathi, E., The phenomenon of population aging in Iran. Iranian Journal of Official Statistics Studies. 2020; 30(2):387-413. [Link]
- Sarrami Foroushani N, Mohammadkhani P, Rasti J. [The effectiveness of mindfulness-based cognitive therapy on the symptoms of pain perception in older women (Persian)]. Salmand: Iranian Journal of Ageing. 2024; 19(2):242-57. [DOI:10.32598/sija.2023.3669.1]
- Rahimi F, Shakibazadeh E, Ashoorkhani M, Foroughan M. [Facilitators of elderly care at home and the educational needs of the family caregivers of older adults in the South of Tehran, Iran: A qualitative study (Persian)]. Iranian Journal of Ageing. 2024; 19(2):222-41. [DOI:10.32598/sija.2023.3668.1]
- Mahmoudzadeh H, Aghayari Hir T, Hatami D. [Study and analysis of the elderly population of the Iran (Persian)]. Geographical Researches. 2022; 37(1):111-25. [Link]
- Bahador F, Mahfoozpour S, Masoudi Asl I, Vahdat S. [Identifying the Main Factors of Providing Primary Preventive Care Services to the Elderly in Iran (Persian)]. Iranian Journal of Ageing. 2023; 17(4):506-21. [DOI:10.32598/sija.2022.3180.3]
- Doshmangir L, Khabiri R, Gordeev VS. Policies to address the impact of an ageing population in Iran. The Lancet. 2023; 401(10382):1078. [DOI:10.1016/S0140-6736(23)00179-4] [PMID]
- Thomas ES, Mathew G, Prajnashree, George SM, Nandakumar UP, Subramanya C. Assessment of factors affecting sleep quality in geriatric patients: A cross-sectional single centre study. Sleep and Vigilance. 2024; 8(1):89-97. [DOI:10.1007/s41782-023-00260-5]
- Torabi A, Ilali E S, Emadian SO, Mousavinasab N. [Comparison of the effect of sleep hygiene education with the cognitive and behavioral method on the quality of sleep in elderly (Persian)]. Journal of Gerontology. 2019; 4(3):9-17. [DOI:10.29252/joge.4.2.9]
- Song Y, Dong Q, Chang Z, Song C, Cui K, Wu S, et al. The impact of sleep quality and its change on the long-term risk of stroke in middle-aged and elderly people: Findings from the English Longitudinal Study of Ageing. Sleep Medicine. 2023; 107:281-8. [DOI:10.1016/j.sleep.2023.04.032] [PMID]
- Takemura N, Cheung DST, Fong DYT, Lee AWM, Lam TC, Ho JC, et al. Effectiveness of Aerobic Exercise and Tai Chi interventions on sleep quality in patients with advanced lung cancer: A randomized clinical trial. JAMA Oncology. 2024; 10(2):176-84. [DOI:10.1001/jamaoncol.2023.5248] [PMID]
- Ou-Yang CL, Ma LB, Wu XD, Ma YL, Liu YH, Tong L, et al. Association of sleep quality on the night of operative day with postoperative delirium in elderly patients: A prospective cohort study. European Journal of Anaesthesiology. 2024; 41(3):226-33. [DOI:10.1097/EJA.0000000000001952] [PMID]
- Nasiri K, Shriniy M, Pashaki NJ, Aghamohammadi V, Saeidi S, Mirzaee M, et al., The effect of foot bath on sleep quality in the elderly: A systematic review. BMC Geriatrics. 2024; 24(1):191. [DOI:10.1186/s12877-023-04590-x] [PMID]
- Moradzadeh R, Sadeghniiat-Haghighi K, Najafi A, Sharifi H, Abdolmohamadi N, Hadavandsiri F, et al. Sleep quality and associated factors among people who inject drugs in Iran: A nationwide survey using respondent-driven sampling. BMC Public Health. 2024; 24(1):2119. [DOI:10.1186/s12889-024-19368-y] [PMID]
- Amato L, Giannetta N, Taborri S, Dionisi S, Panattoni N, Di Simone E, et al. Sleep quality and medication adherence in older adults: A systematic review. Clocks & Sleep. 2024; 6(3):488-98. [DOI:10.3390/clockssleep6030032] [PMID]
- Kamat D, Al-Ajlouni YA, Hall RCW. The therapeutic impact of plant-based and nutritional supplements on anxiety, depressive symptoms and sleep quality among adults and elderly: A systematic review of the literature. International Journal of Environmental Research and Public Health. 2023; 20(6):5171. [DOI:10.3390/ijerph20065171] [PMID]
- Yan M, Fan J, Liu X, Li Y, Wang Y, Tan W, et al. Acupuncture and sleep quality among patients with parkinson disease: A randomized clinical trial. JAMA Network Open. 2024; 7(6):e2417862. [DOI:10.1001/jamanetworkopen.2024.17862] [PMID]
- Haggerty D, Contreras DA, Carter A, Drake C, Tucker RM. SLeep Education for Everyone Program (SLEEp) results in sustained improvements in sleep outcomes at six months. Behavioral Sleep Medicine. 2023; 21(5):601-7. [DOI:10.1080/15402002.2022.2146693] [PMID]
- United Nations. International day of older persons. New York: United Nations ; 2021. [Link]
- Liu S, Lu Y, Wang D, He X, Ren W, Kong D, et al. Impact of digital health literacy on health-related quality of life in Chinese community-dwelling older adults: The mediating effect of health-promoting lifestyle. Frontiers in Public Health. 2023; 11:1200722. [DOI:10.3389/fpubh.2023.1200722] [PMID]
- Zafari E, Rokhafroz D, Dashtbozorgi B, Maraghi E. [The effectiveness of based-mobile education on anxiety of patients candidate coronary angiography (Persian)]. Journal of Critical Care Nursing. 2019; 12(2):35-41. [Link]
- Taheri Tanjani P, Khodabakhshi H, Etemad K, Mohammadi M. [Effect of sleep hygiene education on sleep quality and general health of elderly women with sleep disorders living in Birjand City, Iran, in 2016 (Persian)]. Iranian Journal of Ageing. 2019; 14(2):248-59. [Link]
- Mohammad Gholi Mezerji N, Naseri P, Omraninezhad Z, Shayan Z. The reliability and validity of the Persian Version of Pittsburgh Sleep Quality Index in Iranian People. Avicenna Journal of Neuro Psycho Physiology. 2017; 4(3):95-102. [DOI: 10.32598/ajnpp.4.3.95]
- Ahmadi S, Khankeh H, Mohammadi F, Fallahi Khoshknab M, Reza Soltani P. [The effect of sleep restriction treatment on quality of sleep in the elders (Persian)]. Salmand: Iranian Journal of Ageing . 2010; 5(2):7-15. [Link]
- Luo J, Zhu G, Zhao Q, Guo Q, Meng H, Hong Z, et al. Prevalence and risk factors of poor sleep quality among Chinese elderly in an urban community: Results from the Shanghai aging study. PLoS One. 2013; 8(11):e81261. [DOI:10.1371/journal.pone.0081261] [PMID]
- Borji M, Jahani S, Shiri P, Azami M. [Assessing the status of sleep quality in elderly city of Ilam in 2015 (Persian)]. Journal of Geriatric Nursing. 2016; 2(3):44-53. [DOI:10.21859/jgn.2.3.44]
- Tel H. Sleep quality and quality of life among the elderly people. Neurology, Psychiatry and Brain Research. 2013; 19(1):48-52. [DOI:10.1016/j.npbr.2012.10.002]
- Bahrami M, Dehdashti AR, Karami M. [A survey on sleep quality in elderly people living in a nursing home in Damghan city in 2017: A short report (Persian)]. Journal of Rafsanjan University of Medical Sciences. 2017; 16(6):581-90. [Link]
- Li N, Xu G, Chen G, Zheng X. Sleep quality among Chinese elderly people: A population-based study. Archives of Gerontology and Geriatrics. 2020; 87:103968. [DOI:10.1016/j.archger.2019.103968] [PMID]
- Wang P, Song L, Wang K, Han X, Cong L, Wang Y, et al. Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area: A population-based study. Aging Clinical and Experimental Research, 2020; 32(1):125-31. [DOI:10.1007/s40520-019-01171-0] [PMID]
- Ulusoy Kaymak S, Peker S, Şahin Cankurtaran E, Soygür AH. [Sleep Problems in the Geriatric Population (Turkish)]. Journal of Academic Geriatrics. 2010; 2(2):61-70. [Link]
- Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: 1. Sleep disorders commonly found in older people. CMAJ : Canadian Medical Association Journal. 2007; 176(9):1299-304. [DOI:10.1503/cmaj.060792] [PMID]
- Hoch CC, Reynolds CF 3rd, Buysse DJ, Monk TH, Nowell P, Begley AE, et al. Protecting sleep quality in later life: A pilot study of bed restriction and sleep hygiene. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2001; 56(1):P52-9. [DOI:10.1093/geronb/56.1.P52] [PMID]
- Moradi M, Mohammadzadeh H, Noori R, Basiri Moghadam K, Sadeghmoghadam L. [Effect of a sleep hygiene education program using telephone follow-up method on the sleep quality of the elderly (Persian)]. Salmand: Iranian Journal of Ageing. 2021; 15(4):484-95. [DOI:10.32598/sija.15.4.2895.1]
- Montazeri lemrasky M, Shamsalinia A, Hajiahmadi M, Nasiri M. [The effectiveness of education on factors affecting elderly women's sleep (Persian)] Caspian Journal of Health and Aging. 2018; 3(1):59-68. [DOI: 10.22088/cjhaa.3.1.59]
- Mottaghi R, Maredpour AR, Kharamin S. [The effectiveness of sleep health education on sleep quality, blood pressure, heart rate and oxygen saturation in blood of the elderly with insomnia (Persian)]. Aging Psychology. 2021; 7(3):282-69. [DOI:10.22126/jap.2021.6498.1538]
- Rezaei B, Shooshtarizadeh S. [Factors related to sleep quality among elderly residing at Isfahan nursing homes (Persian)]. Journal of Geriatric Nursing. 2016; 2(2):37-49. [Link]
- Chung K, Kim S, Lee E, Park JY. Mobile App use for insomnia self-management in urban community-dwelling older Korean Adults: Retrospective intervention study. JMIR mHealth and uHealth. 2020; 8(8):e17755. [DOI:10.2196/17755] [PMID]
- de Almondes KM, Leonardo MEM, Moreira AMS. Effects of a cognitive training program and sleep hygiene for executive functions and sleep quality in healthy elderly. Dementia & Neuropsychologia, 2017; 11(1):69-78. [PMID]
- Sharma K, Srivastava S. The effectiveness of sleep hygiene program on sleep quality and stress level in elderly population. Journal of Mental Health and Aging. 2018; 2(1):29-32. [DOI:10.35841/mental-health-aging.2.1.29-32]
- Wei Y, Guo X. Impact of smart device use on objective and subjective health of older adults: Findings from four provinces in China. Frontiers in Public Health. 2023; 11:1118207. [DOI:10.3389/fpubh.2023.1118207] [PMID]
- Dai H, Sun C, Chen J, Zhou X, Li H, Martin P, et al. The mediating effect of eHealth literacy on the relationship between health personality and quality of life in community-dwelling older adults. Geriatric Nursing. 2024; 56:237-43. [DOI:10.1016/j.gerinurse.2024.02.002] [PMID]
- Li S, Cui G, Yin Y, Wang S, Liu X, Chen L. Health-promoting behaviors mediate the relationship between eHealth literacy and health-related quality of life among Chinese older adults: A cross-sectional study. Quality of Life Research. 2021; 30(8):2235-43. [DOI:10.1007/s11136-021-02797-2] [PMID]
- Lee S, Yu S. Effectiveness of Information and Communication Technology (ICT) interventions in elderly’s sleep disturbances: A systematic review and meta-analysis. Sensors (Basel). 2021; 21(18):6003. [DOI:10.3390/s21186003] [PMID]
- Urbanová L, Vaníček O, Červená K, Bartoš A, Evansová K. The impact of sleep education, light intervention and relaxation on sleep and mood in the elderly. Chronobiology International. 2024; 41(4):567-76. [DOI:10.1080/07420528.2024.2337007] [PMID]
- Souilm N, Elsakhy NM, Alotaibi YA, Ali SAO. Effectiveness of emotional freedom techniques (EFT) vs sleep hygiene education group therapy (SHE) in management of sleep disorders among elderly. Scientific Reports. 2022; 12(1):6521. [DOI:10.1038/s41598-022-10456-w] [PMID]
- Grotto G, Martinello M, Buja A. Use of mHealth technologies to increase sleep quality among older adults: A scoping review. Clocks & Sleep. 2024; 6(3):517-32. [DOI:10.3390/clockssleep6030034] [PMID]
- Hornung OP, Danker-Hopfe H, Heuser I. Age-related changes in sleep and memory: Commonalities and interrelationships. Experimental Gerontology. 2005; 40(4):279-85. [DOI:10.1016/j.exger.2005.02.001] [PMID]
Type of Study: Research |
Subject:
nursing
Received: 2024/08/25 | Accepted: 2024/10/20 | Published: 2025/04/01
Received: 2024/08/25 | Accepted: 2024/10/20 | Published: 2025/04/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |