Volume 20, Issue 4 (Winter 2026)
Salmand: Iranian Journal of Ageing 2026, 20(4): 514-527 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sadeghi S, Ghavami V, Amini M, Tehrani H. Predictors of Sleep Quality in Iranian Older Adults Based on the Self-regulation Theory. Salmand: Iranian Journal of Ageing 2026; 20 (4) :514-527
URL: http://salmandj.uswr.ac.ir/article-1-2928-en.html
URL: http://salmandj.uswr.ac.ir/article-1-2928-en.html
1- Student Research Committee, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Department of Biostatistics, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Internal Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Social Determinant of Health Research Center, Mashhad University of Medical Sciences, Mashhad, Iran. & Department of Health Education and Health Promotion, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran. ,tehranih@mums.ac.ir
2- Department of Biostatistics, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Internal Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Social Determinant of Health Research Center, Mashhad University of Medical Sciences, Mashhad, Iran. & Department of Health Education and Health Promotion, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran. ,
Full-Text [PDF 5140 kb]
(1465 Downloads)
| Abstract (HTML) (2937 Views)
Full-Text: (380 Views)
Introduction
The increase in the number of older adults presents significant challenges, underscoring the need for special consideration of this issue. The mental and physical health of the elderly requires particular attention. Research has shown that the prevalence of insomnia increases with age. Sleep disorders in older adults can lead to a range of serious consequences, including depression, loss of balance and risk of falls, memory disorders, reduced quality of life, cognitive impairment, fatigue, anxiety, and an increased reliance on sleeping pills. Epidemiological studies have indicated that individuals with sleep disorders require more healthcare services, and this issue imposes a significant economic burden on both patients and healthcare systems. Therefore, this study aimed to identify the factors associated with sleep quality and find its predictors among Iranian older adults, based on the social cognitive theory of self-regulation.
Methods & Materials
This is a cross-sectional, descriptive study that was conducted in 2024. The participants were 335 older adults, who were selected using a multi-stage cluster random sampling method from three comprehensive health centers in Neishabur, Iran. The inclusion criteria were age over 60 years, willingness to participate in the study, and the ability to answer the questionnaire. The individuals who failed to complete the questionnaires entirely were excluded. The data collection tools included a demographic form, a researcher-made questionnaire to assess self-regulation scores, and the pittsburgh sleep quality index (PSQI) to measure sleep quality, with higher scores indicating more severe sleep disorders. The questionnaire designed based on the social cognitive theory of self-regulation consisted of 31 items and four dimensions: goal setting (6 items), self-reaction (7 items), self-monitoring (12 items), and judgment of a behavior (6 items). Its content validity index (CVI) was 0.86, and the content validity ratio (CVR) was 0.73. The Cronbach’s alpha coefficient was calculated to be 0.93, and its test, re-test reliability was ICC=0.93. SPSS software version 26 was utilized to analyze the collected data using both descriptive and inferential statistics. For all tests, the significance level was set at 0.05.
Results
The majority of participants were female (51%) and married (73%). Their mean age was 74.00±8.97 years. In terms of education, 70% had less than a high school diploma. Also, 65% had private bedrooms, while 16% did not have bedrooms. The majority did not smoke (73%) and had an underlying disease (82%).
The results indicated that 70.4% of older adults had poor sleep quality. Their mean self-regulation score was 81.96±17.26, and the mean PSQI score was 8.54±4.65. The total PSQI score for those who took sleeping pills was 12.50±2.82, while for those who did not take sleeping pills, it was 5.51±3.30. This indicates that users of sleeping pills had significantly lower sleep quality (P<0.001). There was no significant difference in sleep quality between smokers and non-smokers (P=0.095). Spearman’s correlation coefficient test revealed a direct and significant correlation between age and total PSQI score (P<0.001). Among the PSQI components, sleep efficiency had the highest score, indicating that the participants had poor sleep efficiency. In contrast, sleep duration had the lowest score, indicating that the participants had better sleep duration.
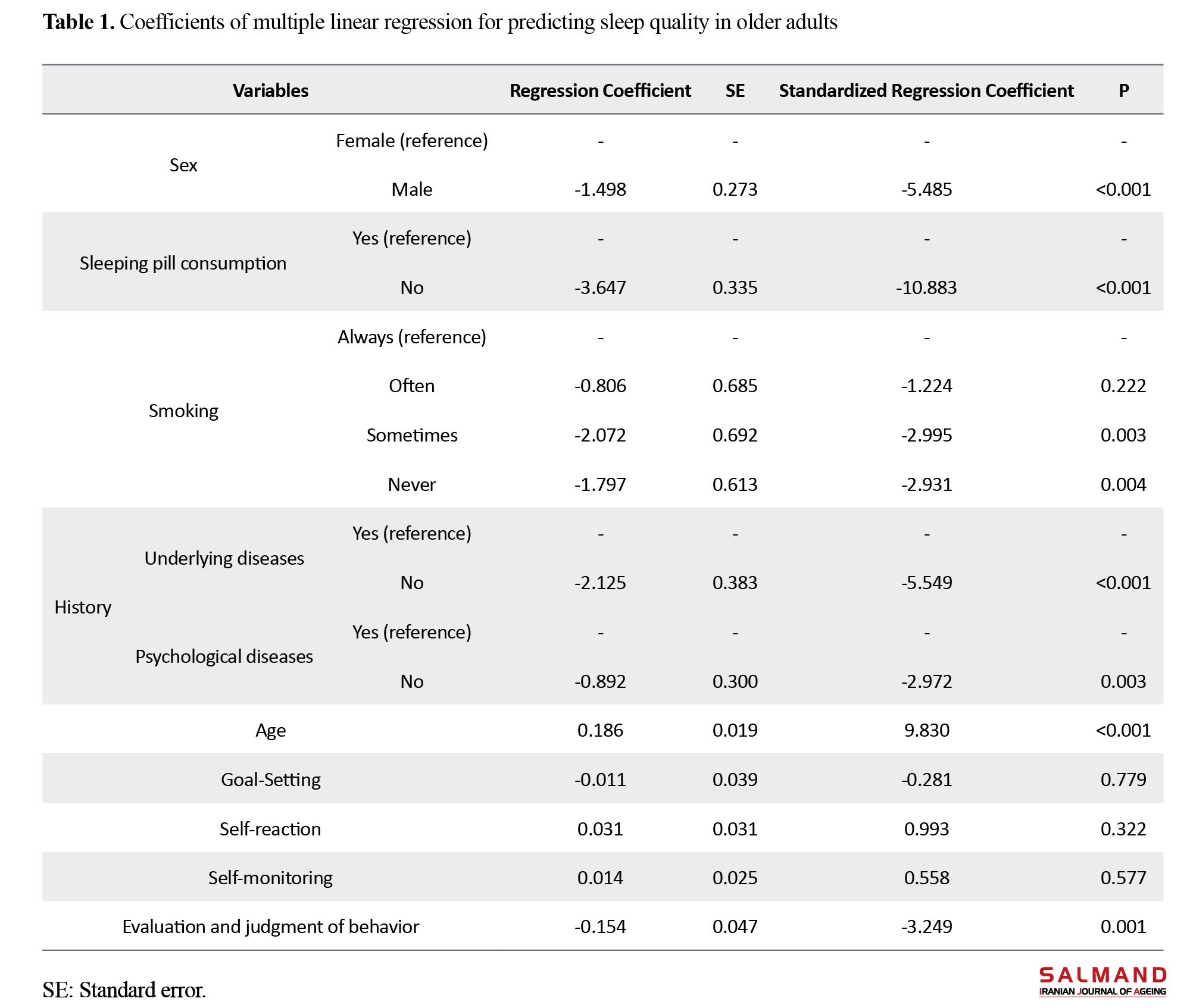
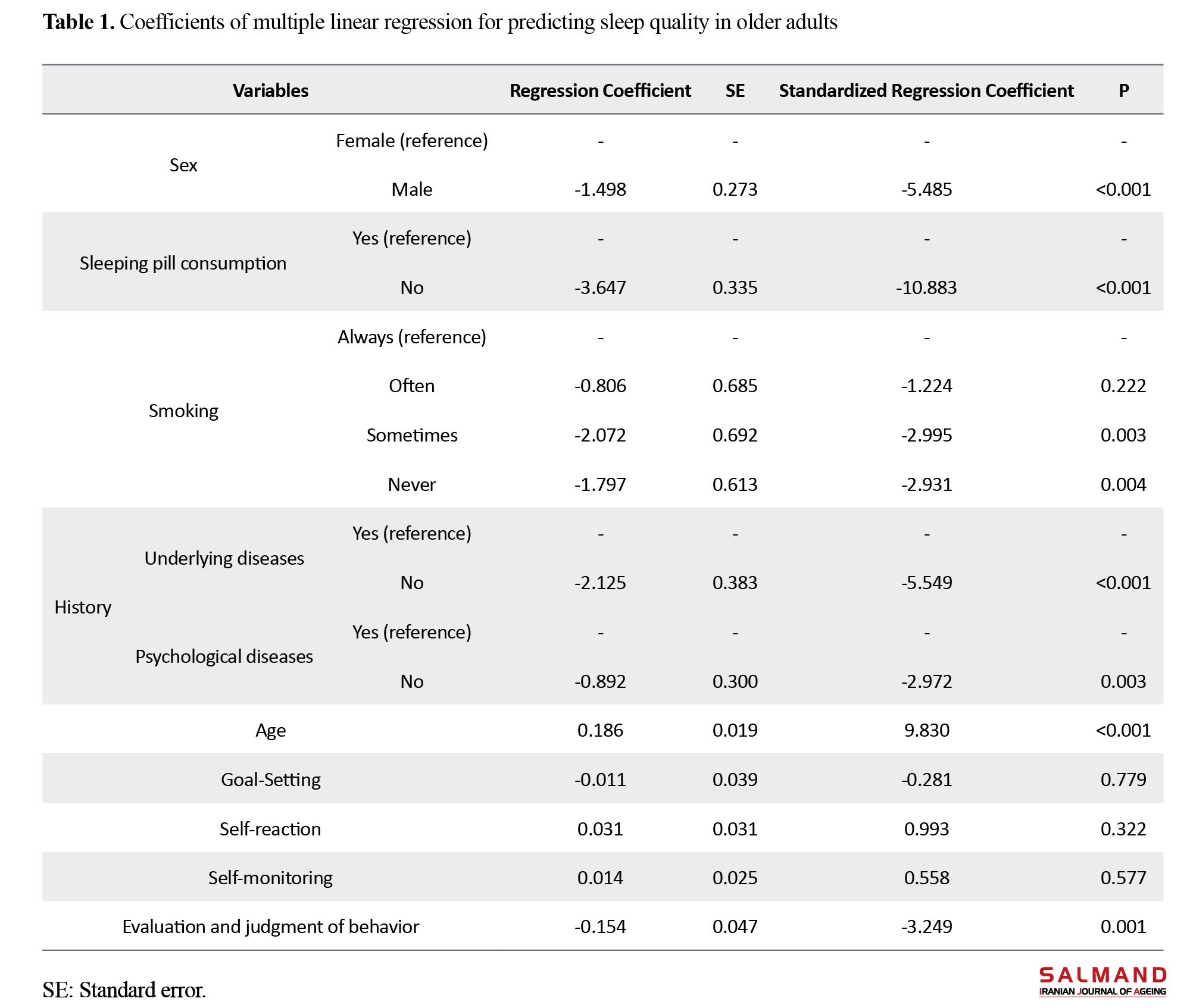
Based on the results of the univariate linear regression, behavior evaluation and judgment (P<0.001), goal setting (P=0.001), and self-monitoring (P=0.009) were the most effective predictors of sleep quality in older adults. Based on the results of multiple regression, non-use of sleeping pills (β=-10.883, P<0.001), age (β=9.830, P<0.001), no history of underlying disease (β=-5.549, P<0.001), male gender (β=-5.485, P<0.001), behavior evaluation and judgment (β=-3.249, P<0.001), no history of psychological diseases (β=-2.972, P=0.003) and non-smoking (β=-2.931, P=0.004) were predictors of sleep quality (Table 1).
This final regression model explained 78% of the variance in sleep quality.
Conclusion
The results indicated that poor sleep efficiency was higher among older adults compared to other components of sleep quality. Among the dimensions of self-regulation theory, behavior evaluation and judgment had the highest power in predicting sleep quality, compared to goal-setting and self-monitoring domains. This finding indicates that older adults who are better at evaluating and judging their behavior tend to have better sleep quality. Therefore, it is recommended to design appropriate interventions aimed at empowering older adults to promote their health and improve their sleep quality, focusing on these strategies of self-regulation theory. Among the demographic variables, the non-use of sleeping pills had the highest power in predicting sleep quality of older adults. Based on these results, the use of non-pharmacological methods, such as behavioral interventions, stimulus control, sleep hygiene practices, and cognitive techniques, is recommended to prevent and manage sleep disorders in this group.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Ethics Committee of Mashhad University of Medical Sciences (Code: IR.MUMS.REC.1402.100). Participants provided written informed consent after receiving explanations about the study objectives and methods, and were assured of the confidentiality of their information.
Funding
This article was extracted from the master’s thesis of Sara Sadeghi, funded by Mashhad University of Medical Sciences.
Authors' contributions
Design and conceptualization: Hadi Tehrani, Mahnaz Amini, and Vahid Ghavami; data collection, writing the initial draft: Hadi Tehrani and Sara Sadeghi: data analysis and interpretation: Vahid Ghavami; review & editing: All authors.
Conflicts of interest
The authors declare no competing interests.
Acknowledgments
The authors would like to thank the Vice-Chancellor for Research of Mashhad University of Medical Sciences, the management and staff of comprehensive health centers in Neyshapour, and all participants for their support and cooperation.
References
The increase in the number of older adults presents significant challenges, underscoring the need for special consideration of this issue. The mental and physical health of the elderly requires particular attention. Research has shown that the prevalence of insomnia increases with age. Sleep disorders in older adults can lead to a range of serious consequences, including depression, loss of balance and risk of falls, memory disorders, reduced quality of life, cognitive impairment, fatigue, anxiety, and an increased reliance on sleeping pills. Epidemiological studies have indicated that individuals with sleep disorders require more healthcare services, and this issue imposes a significant economic burden on both patients and healthcare systems. Therefore, this study aimed to identify the factors associated with sleep quality and find its predictors among Iranian older adults, based on the social cognitive theory of self-regulation.
Methods & Materials
This is a cross-sectional, descriptive study that was conducted in 2024. The participants were 335 older adults, who were selected using a multi-stage cluster random sampling method from three comprehensive health centers in Neishabur, Iran. The inclusion criteria were age over 60 years, willingness to participate in the study, and the ability to answer the questionnaire. The individuals who failed to complete the questionnaires entirely were excluded. The data collection tools included a demographic form, a researcher-made questionnaire to assess self-regulation scores, and the pittsburgh sleep quality index (PSQI) to measure sleep quality, with higher scores indicating more severe sleep disorders. The questionnaire designed based on the social cognitive theory of self-regulation consisted of 31 items and four dimensions: goal setting (6 items), self-reaction (7 items), self-monitoring (12 items), and judgment of a behavior (6 items). Its content validity index (CVI) was 0.86, and the content validity ratio (CVR) was 0.73. The Cronbach’s alpha coefficient was calculated to be 0.93, and its test, re-test reliability was ICC=0.93. SPSS software version 26 was utilized to analyze the collected data using both descriptive and inferential statistics. For all tests, the significance level was set at 0.05.
Results
The majority of participants were female (51%) and married (73%). Their mean age was 74.00±8.97 years. In terms of education, 70% had less than a high school diploma. Also, 65% had private bedrooms, while 16% did not have bedrooms. The majority did not smoke (73%) and had an underlying disease (82%).
The results indicated that 70.4% of older adults had poor sleep quality. Their mean self-regulation score was 81.96±17.26, and the mean PSQI score was 8.54±4.65. The total PSQI score for those who took sleeping pills was 12.50±2.82, while for those who did not take sleeping pills, it was 5.51±3.30. This indicates that users of sleeping pills had significantly lower sleep quality (P<0.001). There was no significant difference in sleep quality between smokers and non-smokers (P=0.095). Spearman’s correlation coefficient test revealed a direct and significant correlation between age and total PSQI score (P<0.001). Among the PSQI components, sleep efficiency had the highest score, indicating that the participants had poor sleep efficiency. In contrast, sleep duration had the lowest score, indicating that the participants had better sleep duration.
Based on the results of the univariate linear regression, behavior evaluation and judgment (P<0.001), goal setting (P=0.001), and self-monitoring (P=0.009) were the most effective predictors of sleep quality in older adults. Based on the results of multiple regression, non-use of sleeping pills (β=-10.883, P<0.001), age (β=9.830, P<0.001), no history of underlying disease (β=-5.549, P<0.001), male gender (β=-5.485, P<0.001), behavior evaluation and judgment (β=-3.249, P<0.001), no history of psychological diseases (β=-2.972, P=0.003) and non-smoking (β=-2.931, P=0.004) were predictors of sleep quality (Table 1).
This final regression model explained 78% of the variance in sleep quality.
Conclusion
The results indicated that poor sleep efficiency was higher among older adults compared to other components of sleep quality. Among the dimensions of self-regulation theory, behavior evaluation and judgment had the highest power in predicting sleep quality, compared to goal-setting and self-monitoring domains. This finding indicates that older adults who are better at evaluating and judging their behavior tend to have better sleep quality. Therefore, it is recommended to design appropriate interventions aimed at empowering older adults to promote their health and improve their sleep quality, focusing on these strategies of self-regulation theory. Among the demographic variables, the non-use of sleeping pills had the highest power in predicting sleep quality of older adults. Based on these results, the use of non-pharmacological methods, such as behavioral interventions, stimulus control, sleep hygiene practices, and cognitive techniques, is recommended to prevent and manage sleep disorders in this group.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Ethics Committee of Mashhad University of Medical Sciences (Code: IR.MUMS.REC.1402.100). Participants provided written informed consent after receiving explanations about the study objectives and methods, and were assured of the confidentiality of their information.
Funding
This article was extracted from the master’s thesis of Sara Sadeghi, funded by Mashhad University of Medical Sciences.
Authors' contributions
Design and conceptualization: Hadi Tehrani, Mahnaz Amini, and Vahid Ghavami; data collection, writing the initial draft: Hadi Tehrani and Sara Sadeghi: data analysis and interpretation: Vahid Ghavami; review & editing: All authors.
Conflicts of interest
The authors declare no competing interests.
Acknowledgments
The authors would like to thank the Vice-Chancellor for Research of Mashhad University of Medical Sciences, the management and staff of comprehensive health centers in Neyshapour, and all participants for their support and cooperation.
References
- Madan Jha V. The prevalence of sleep loss and sleep disorders in young and old adults. Aging Brain. 2022; 3:100057. [DOI:10.1016/j.nbas.2022.100057] [PMID]
- Beyrami M, Alizadeh Goradel J, Ansarhosein S, Ghahraman Moharrampour N. [Comparing sleep quality and general health among the elderly living at home and at nursing home (Persian)]. Iranian Journal of Ageing. 2014; 8(4):47-55. [Link]
- Streatfeild J, Smith J, Mansfield D, Pezzullo L, Hillman D. The social and economic cost of sleep disorders. Sleep. 2021; 44(11):zsab132. [DOI:10.1093/sleep/zsab132] [PMID]
- Mastin DF, Bryson J, Corwyn R. Assessment of sleep hygiene using the Sleep Hygiene Index. Journal of Behavioral Medicine. 2006; 29(3):223-7. [DOI:10.1007/s10865-006-9047-6] [PMID]
- Sagayadevan V, Abdin E, Binte Shafie S, Jeyagurunathan A, Sambasivam R, Zhang Y, et al. Prevalence and correlates of sleep problems among elderly Singaporeans. Psychogeriatrics. 2017; 17(1):43-51. [DOI:10.1111/psyg.12190] [PMID]
- Niu J, Han H, Wang Y, Wang L, Gao X, Liao S. Sleep quality and cognitive decline in a community of older adults in Daqing City, China. Sleep Medicine. 2016; 17:69-74. [DOI:10.1016/j.sleep.2015.07.033] [PMID]
- Shamshri M, Moshki M, Mogharab M. [The survey of sleep quality and its relationship to mental health of hospital nurses (Persian)]. Iran Occupational Health Journal. 2014; 11(3):96-104. [Link]
- Tanaka H, Tamura N. Sleep education with self-help treatment and sleep health promotion for mental and physical wellness in Japan. Sleep and Biological Rhythms. 2016; 14:89-99. [DOI:10.1007/s41105-015-0018-6] [PMID]
- Lima P, Medeiros A, Araujo J. Sleep-wake pattern of medical students: Early versus late class starting time. Brazilian Journal of Medical and Biological Research. 2002; 35(11):1373-7. [DOI:10.1590/S0100-879X2002001100016] [PMID]
- Sneha O, Pawar AA, Patil SS, Shinde M, Dhanshri H, Udaykumar K. Quality of Sleep Among Old Age Patients. Journal of Pharmaceutical Negative Results. 2022; 596-600. [DOI:10.47750/pnr.2022.13.S06.085]
- Amrahi Tabieh A, Sarbakhsh P, Namjoo S, Akbari H, Allahverdipour H. [Investigating the relationship between sleep quality, sleep duration, and frailty syndrome among older adults in Naqadeh, 2020 (Persian)]. Iranian Journal of Epidemiology. 2024; 19(4):280-9. [Link]
- Hariri M, Shamshirgaran SM, Amini A, Abasi H, Gholami A. Sleep duration and quality are associated with health-related quality of life in adults aged 60 years and older. Irish journal of Medical Science. 2024; 193(4):1929-37. [DOI:10.1007/s11845-024-03656-y] [PMID]
- Heidari P, Siabani S, Siabani S, Mahaki B, Heidari N. [Designing, Implementing, and Evaluation a Health Promotion Program Using PRECEDE-PROCEED Model on the Participation Rate of Mothers, with Preschool Children (3-6 year), in Fluoride Varnish Program (Persian)]. Iranian Journal of Health Education and Health Promotion. 2024; 12(2):155-70. [DOI: 10.22034/12.2.6]
- Wilandika A, Yusuf A, Kurniawati ND, Sari DN. HIV Health Literacy (HALTRA) Model: A new model based on information and motivation to eradicate social stigma. Journal of Health Literacy. 2024; 9(2):23-39. [Link]
- Hosseini FS, Hatamnezhad O. [Relationship between self-regulation and balance-confidence in active and inactive elderly men (Persian)]. Iranian Journal of Ageing. 2018; 12(4):470-81. [DOI:10.21859/sija.12.4.470]
- Bandura A. Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes. 1991; 50(2):248-87. [DOI:10.1016/0749-5978(91)90022-L]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004; 31(2):143-64. [DOI:10.1177/1090198104263660] [PMID]
- Soleimani S, Ghaffari M, Rakhshanderou S. [The effect of theory based educational intervention on self-efficacy and activities of daily living in the older people resident in nursing homes in Isfahan city (Persian)]. Iranian Journal of Health Education and Health Promotion. 2023; 11(3):262-74. [DOI: 10.22034/11.3.262]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989; 28(2):193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Momeni KH, Karimi H. [The comparison of general health of the residents/non residents in the elder house (Persian)]. Salmand: Iranian Journal of Ageing . 2010; 5(17):23-9. [Link]
- Hasanzadeh M, Alavi KN, Ghalehbandi M, Yad EZ, Gharaei B, Sadeghikia A. Sleep quality in Iranian drivers recognized as responsible for severe road accidents. Journal of Research in Behavioral Sciences. 2008; 6(2):97-107. [Link]
- Desjardins S, Lapierre S, Hudon C, Desgagné A. Factors involved in sleep efficiency: A population-based study of community-dwelling elderly persons. Sleep. 2019; 42(5):zsz038. [DOI:10.1093/sleep/zsz038] [PMID]
- Izadi Avanji FS, Adib Hajbaghery M, Afazel MR. [Quality of sleep and it's related factors in the hospitalized elderly patients of Kashan hospitals in 2007 (Persian)]. Feyz Medical Sciences Journal. 2009; 12(4):52-60. [Link]
- Braund H, Timmons K. Operationalization of self-regulation in the early years: comparing policy with theoretical underpinnings. International Journal of Child Care and Education Policy. 2021; 15(1):8. [DOI:10.1186/s40723-021-00085-7]
- Yue Z, Zhang Y, Cheng X, Zhang J. Sleep quality among the Elderly in 21st Century Shandong Province, China: A ten-year comparative study. International Journal of Environmental Research and Public Health. 2022; 19(21):14296. [DOI:10.3390/ijerph192114296] [PMID]
- Redeker NS. Sleep in acute care settings: An integrative review. Journal of Nursing Scholarship. 2000; 32(1):31-8. [DOI:10.1111/j.1547-5069.2000.00031.x] [PMID]
- Chu HS, Oh J, Lee K. The relationship between living arrangements and sleep quality in older adults: Gender differences. International Journal of Environmental Research and Public Health. 2022; 19(7):3893. [DOI:10.3390/ijerph19073893] [PMID]
- Fatima Y, Doi SA, Najman JM, Mamun AA. Exploring gender difference in sleep quality of young adults: findings from a large population study. Clinical Medicine & Research. 2016; 14(3-4):138-44. [DOI:10.3121/cmr.2016.1338] [PMID]
- Borji M, Jahani S, Shiri P, Azami M. [Assessing sleep quality among the elderly people in Ilam city in 2015 (Persian)]. 2018; 2(3):44-53. [Link]
- Seo YM, Kim JS, Je NJ. Factors relating quality of sleep: Comparison between young-old people and old-old people. Journal of the Korea Academia-Industrial cooperation Society. 2019; 20(6):332-41. [Link]
- Bahrami M, Dehdashti AR, Karami M. [A survey on sleep quality in elderly people living in a Nursing Home in Damghan City in 2017: A short report (Persian)]. Journal of Rafsanjan University of Medical Sciences. 2017; 16(6):581-90. [Link]
- Habibi P, Moudi S, Ghadimi R. [Factors affecting sleep quality in older adults in Amol, Iran: A causal study (Persian)]. Journal of Mazandaran University of Medical Sciences. 2023; 33(222):67-76.[Link]
Type of Study: Research |
Subject:
gerontology
Received: 2024/09/05 | Accepted: 2024/11/04 | Published: 2026/03/01
Received: 2024/09/05 | Accepted: 2024/11/04 | Published: 2026/03/01
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |